EMEND 125 mg POWDER FOR ORAL SUSPENSION

How to use EMEND 125 mg POWDER FOR ORAL SUSPENSION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
EMEND 125mg powder for oral suspension
aprepitant
Read all of this leaflet carefully before you start giving this medicine to your child because it contains important information for them.This leaflet has been written for the parent or caregiver who will be giving this medicine to the child. Read this information carefully.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for your child only. Do not give it to others, even if they have the same symptoms. It may harm them.
- If your child experiences side effects, consult your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is EMEND and what is it used for
- What you need to know before you start giving EMEND
- How to give EMEND
- Possible side effects
- Storing EMEND
- Package contents and further information
1. What is EMEND and what is it used for
EMEND contains the active substance aprepitant. It belongs to a group of medicines called 'neurokinin 1 (NK1) receptor antagonists'. The brain has a specific area that controls nausea and vomiting. EMEND works by blocking the signals to this area, reducing nausea and vomiting. The oral suspension is used in children from 6 months to less than 12 years of age, in combinationwith other medicinesto prevent nausea and vomiting caused by a type of chemotherapy (cancer treatment) that induces strong and moderate nausea and vomiting (such as cisplatin, cyclophosphamide, doxorubicin, or epirubicin).
2. What you need to know before you start giving EMEND
Do not give EMEND
- if your child is allergic to aprepitant or any of the other ingredients of this medicine (listed in section 6).
- if your child is taking medicines that contain 'pimozide' (for mental health problems).
- if your child is taking 'terfenadine' or 'astemizole' (for allergic rhinitis and other allergies).
- if your child is taking 'cisapride' (for digestion problems).
Do not give this medicine if your child is in any of the above situations and inform your child's doctor if they are taking any of the medicines mentioned above. This is because their treatment may need to be modified before starting treatment with this medicine. If you are not sure, consult your doctor, pharmacist, or nurse before giving this medicine.
Warnings and precautions
Consult your doctor, pharmacist, or nurse before giving this medicine to your child.
Liver problems
If your child has liver problems, consult your doctor before starting treatment with EMEND. This is because the liver is important for removing the medicine from the body. Your doctor may need to monitor your child's liver condition during treatment.
Children and adolescents
Do not give EMEND oral suspension to children under 6 months of age or weighing less than 6 kg or to adolescents between 12 and 18 years of age, as the oral suspension has not been studied in this population.
Other medicines and EMEND
Tell your doctor, pharmacist, or nurse if your child is taking, has recently taken, or might take any other medicines. This is because EMEND may affect the activity of other medicines during and after treatment with EMEND. Also, some medicines may affect how this medicine works.
Do not give EMEND and inform your doctor or pharmacist if your child is taking any of the following medicines (see also 'Do not give EMEND'). This is because their treatment may need to be modified before starting EMEND:
- pimozide – for mental health problems,
- terfenadine and astemizole – for allergic rhinitis and other allergies,
- cisapride – for digestion problems.
Do not give this medicine and consult your doctor or pharmacist if any of the above applies to your child (or if you are unsure).
Inform your doctor, pharmacist, or nurse if your child is taking any of the following medicines:
- medicines that affect the immune system – such as cyclosporine, tacrolimus, sirolimus, everolimus,
- alfentanil, fentanyl – for pain,
- quinidine – for irregular heartbeats,
- cancer medicines – such as irinotecan, etoposide, vinorelbine, ifosfamide,
- medicines that contain 'ergot-derived alkaloids' - such as ergotamine or dihydroergotamine – for migraines,
- blood-thinning medicines – such as warfarin, acenocoumarol. Your child may need blood tests during treatment with EMEND,
- antibiotics for infections – such as rifampicin, clarithromycin, telithromycin,
- phenytoin – for seizures,
- carbamazepine – for depression and epilepsy,
- midazolam, triazolam, phenobarbital – for sedation or to help with sleep,
- St. John's Wort – a herbal medicine for depression,
- protease inhibitors – for HIV infections,
- ketoconazole, except for shampoo (used to treat Cushing's syndrome – when the body produces too much cortisol),
- antifungal medicines such as itraconazole, voriconazole, posaconazole,
- nefazodone – for depression,
- corticosteroids – such as dexamethasone and methylprednisolone,
- anxiety medicines such as alprazolam,
- tolbutamide – for diabetes,
- contraceptives that include pills, patches, implants, and some intrauterine devices (IUDs) that release hormones. These may not work properly when taken with this medicine. You may need to use a different or additional non-hormonal method of contraception during treatment with this medicine and for up to 2 months after treatment has finished.
Inform your doctor, pharmacist, or nurse before giving this medicine to your child if any of the above applies to them (or if you are unsure).
Pregnancy and breastfeeding
Do not use this medicine during pregnancy and breastfeeding unless clearly necessary.
For information related to pregnancy, breastfeeding, and contraception, ask your doctor for advice.
Driving and using machines
It should be taken into account that some people may feel dizzy and sleepy after taking EMEND. If your child feels dizzy or sleepy, they should not ride a bike or use tools or machines.
EMEND contains sucrose and lactose
The oral suspension contains sucrose and lactose. If your doctor has told you that your child has an intolerance to some sugars, consult them before giving this medicine to your child.
EMEND contains sodium
This medicine contains less than 23 mg of sodium (1 mmol) per dose; this is essentially 'sodium-free'.
3. How to give EMEND
Healthcare professionals: See the end of this leaflet for instructions for healthcare professionals on preparing the oral suspension. It tells you how to prepare the dose of EMEND as an oral suspension.
Parents and caregivers: Follow the administration instructions for this medicine exactly as indicated for your child by their doctor, pharmacist, or nurse. If you are unsure, consult your child's doctor, pharmacist, or nurse again.
It is very important that this medicine is given exactly as indicated below.
For each dose of EMEND, you will have a pre-loaded oral dispenser that contains the prescribed dose for your child.
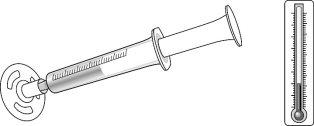
Keep the oral dispenser in the refrigerator (between 2 °C and 8 °C) until you give the medicine to your child.
Use this medicine during the 2 days following receipt of the medicine from the healthcare professional.
Before administration, the medicine can be stored at room temperature (not above 30 °C) for up to 3 hours.
The color of the medicine in the oral dispenser may be different shades of pink (from light pink to dark pink). This is normal and the medicine can be used.
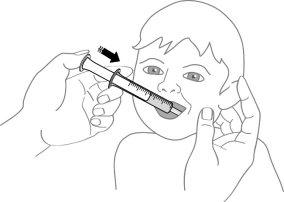
- Remove the cap from the oral dispenser.
- Place the tip of the oral dispenser in the child's mouth on the inner side of the cheek, on the right or left side.
- Slowly push the plunger all the way down the oral dispenser to give the child all the medicine from the dispenser.
If your child cannot take the full dose, call your child's healthcare professional.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of the packaging and any unused medicine. This will help protect the environment.
How much to give
- The doctor will calculate the correct dose of oral suspension based on your child's weight.
- Do not change the dose or stop treatment without consulting your doctor, pharmacist, or nurse first.
When to give
Day 1:
- Give this medicine 1 hour before the start of the chemotherapy session.
Day 2 and Day 3:
- If your child is not having chemotherapy – give this medicine in the morning.
- If your child is having chemotherapy – give this medicine 1 hour before the start of the chemotherapy session.
EMEND can be given with or without food.
Always give this medicine with other medicines to prevent nausea and vomiting. After treatment with EMEND, your doctor may advise your child to continue taking other medicines to prevent nausea and vomiting, such as:
- a corticosteroid – such as dexamethasone and
- a '5-HT3 antagonist' – such as ondansetron
If you are unsure, ask your doctor, pharmacist, or nurse.
If you give more EMEND than you should
Do not give your child more medicine than prescribed by the doctor. If you give your child more than they should, contact your doctor immediately.
If you forget to give EMEND
If your child misses a dose of this medicine, consult your doctor.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Serious side effects
Stop giving this medicine and seek medical help immediately if you or your child notice any of the following serious side effects – your child may need urgent medical treatment:
- allergic reaction – signs may include rash, hives, itching, difficulty breathing or swallowing (frequency not known).
Stop giving this medicine and seek medical help immediately if you notice any of the serious side effects listed above.
Other side effects
Tell your doctor, pharmacist, or nurse if you or your child notice any of the following side effects:
Common:may affect up to 1 in 10 people
- constipation or indigestion,
- headache,
- feeling tired,
- loss of appetite,
- hiccups,
- increase in liver enzymes in the blood (seen in blood tests).
Uncommon:may affect up to 1 in 100 people
- feeling dizzy or sleepy,
- acne, rash,
- feeling anxious,
- belching, nausea, vomiting, heartburn, stomach pain, dry mouth, flatulence,
- pain or burning when urinating,
- feeling weak, general feeling of being unwell,
- flushing/redness of the face or skin,
- rapid or irregular heartbeats,
- fever with a high risk of infection, low red blood cell count (seen in blood tests).
Rare:may affect up to 1 in 1,000 people
- difficulty thinking, lack of energy, changes in taste,
- sensitivity of the skin to sunlight, excessive sweating, oily skin, skin ulcers, itchy rash, Stevens-Johnson syndrome or toxic epidermal necrolysis (rare severe skin reactions),
- euphoria (extreme feeling of happiness), feeling confused,
- bacterial infection, fungal infection,
- severe constipation, stomach, small intestine, and colon inflammation, mouth ulcers, abdominal swelling,
- urinating more frequently or more than usual, sugar or blood in the urine,
- chest discomfort, swelling, changes in walking,
- cough, mucous at the back of the throat, throat irritation, sneezing, sore throat,
- eye discharge and itching,
- ringing in the ears,
- muscle spasms, muscle weakness,
- feeling very thirsty,
- slow heartbeats, blood vessel and vein problems,
- low white blood cell count, low sodium levels in the blood, weight loss.
Reporting of side effects
If your child experiences any side effects, consult your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly through the national reporting system listed in Appendix V. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storing EMEND
Keep this medicine out of the sight and reach of children.
Before reconstitution:
EMEND will generally be stored by healthcare professionals. If needed, the storage details are as follows:
Do not give this medicine to your child after the expiry date which is stated on the carton and blister after EXP. The expiry date is the last day of the month stated.
This medicine does not require any special storage temperature.
Keep in the original packaging to protect from moisture.
After reconstitution:
Before administration, the oral suspension can be stored at room temperature (not above 30 °C) for up to 3 hours. It can also be stored in the refrigerator (between 2 °C and 8 °C) for up to 72 hours.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of the packaging and any unused medicine. This will help protect the environment.
6. Container Contents and Additional Information
Composition of EMEND
- The active ingredient is aprepitant. Each sachet contains 125 mg of aprepitant. After reconstitution, 1 ml of oral suspension contains 25 mg of aprepitant.
- The other ingredients are hydroxypropylcellulose (E-463), sodium lauryl sulfate, sucrose, and lactose (see section 2 "EMEND contains sucrose and lactose"), red iron oxide (E-172), and sodium stearyl fumarate.
Appearance and Container Contents
The powder for oral suspension is a pink to light pink powder in a single-use sachet.
Single-use box
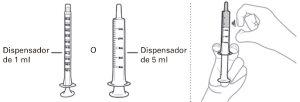
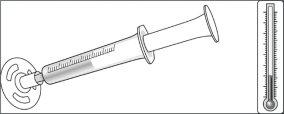
The box contains a sachet, a 1 ml oral dispenser, and a 5 ml oral dispenser (made of polypropylene with a plunger topped with a silicone ring), a cap, and a mixing cup (made of polypropylene).
Marketing Authorization Holder and Manufacturer
Merck Sharp & Dohme B.V. Waarderweg 39 2031 BN Haarlem Netherlands |
You can request more information about this medicine by contacting the local representative of the marketing authorization holder:
Belgium/België/Belgien MSD Belgium Tel: +32(0)27766211 | Lithuania UAB Merck Sharp & Dohme Tel: +370 5 2780 247 |
| Luxembourg/Luxemburg MSD Belgium Tel: +32(0)27766211 |
Czech Republic Merck Sharp & Dohme s.r.o. Tel: +420 233 010 111 | Hungary MSD Pharma Hungary Kft. Tel: +36 1 888 5300 |
Denmark MSD Danmark ApS Tel: +45 4482 4000 | Malta Merck Sharp & Dohme Cyprus Limited Tel: 8007 4433 (+356 99917558) |
Germany MSD Sharp & Dohme GmbH Tel: +49 (0)89 20 300 4500 | Netherlands Merck Sharp & Dohme B.V. Tel: 0800 9999000 (+31 23 5153153) |
Estonia Merck Sharp & Dohme OÜ Tel: +372 614 4200 | Norway MSD (Norge) AS Tel: +47 32 20 73 00 |
Greece MSD Α.Φ.Ε.Ε. Tel: +30 210 98 97 300 | Austria Merck Sharp & Dohme Ges.m.b.H. Tel: +43 (0)1 26 044 |
Spain Merck Sharp & Dohme de España, S.A. Tel: +34 91 321 06 00 | Poland MSD Polska Sp. z o.o. Tel: +48 22 549 51 00 |
France MSD France Tel: +33 (0)1 80 46 40 40 | Portugal Merck Sharp & Dohme, Lda Tel: +351 21 4465700 |
Croatia Merck Sharp & Dohme d.o.o. Tel: +385 1 6611 333 | Romania Merck Sharp & Dohme Romania S.R.L. Tel: +40 21 529 29 00 |
Ireland Merck Sharp & Dohme Ireland (Human Health) Limited Tel: +353 (0)1 2998700 | Slovenia Merck Sharp & Dohme, inovativna zdravila d.o.o. Tel: +386 1 520 4201 |
Iceland Vistor ehf. Tel: +354 535 7000 | Slovak Republic Merck Sharp & Dohme, s. r. o. Tel: +421 2 58282010 |
Italy MSD Italia S.r.l. Tel: 800 23 99 89 (+39 06 361911) | Finland MSD Finland Oy Tel: +358 (0)9 804 650 |
Cyprus Merck Sharp & Dohme Cyprus Limited Tel: 8000 6733 (+357 22866700) | Sweden Merck Sharp & Dohme (Sweden) AB Tel: +46 77 5700488 |
Latvia SIA Merck Sharp & Dohme Latvija Tel: +371 67025300 |
Date of Last Revision of this Leaflet:
Other Sources of Information
Detailed information on this medicine is available on the European Medicines Agency website: https://www.ema.europa.eu.
--------------------------------------------------------------------------------------------------------------------
This information is intended only for healthcare professionals:
Instructions for healthcare professionals on the preparation of the oral suspension
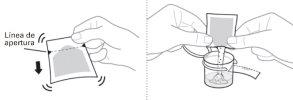
Each box of EMEND contains a sachet with the powder for oral suspension, a 1 ml oral dispenser, a 5 ml oral dispenser, a cap, and a mixing cup. |
| ||
|
| ||
Check that there is no air in the oral dispenser (if there is air, remove it). |
| ||
|
| ||
|
| ||
Hold the EMEND powder for oral suspension sachet upright and shake the contents down before opening the sachet.
|
| ||
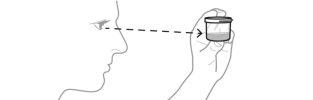
To avoid foam, do not shake the mixing cup. The mixture will be a cloudy pink to light pink color. |
| ||
|
| ||
Check that there is no air in the oral dispenser (if there is air, remove it). Check that the oral dispenser contains the prescribed dose. |
| ||
Day 1 | Day 2 | Day 3 | |
EMEND oral suspension 25 mg/ml | 3 mg/kg orally Maximum dose 125 mg | 2 mg/kg orally Maximum dose 80 mg | 2 mg/kg orally Maximum dose 80 mg |
|
| ||
Discard any leftover suspension and materials that have come into contact with it. The disposal of unused medicine and all materials that have come into contact with it will be carried out in accordance with local regulations. |
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to EMEND 125 mg POWDER FOR ORAL SUSPENSIONDosage form: CAPSULE, 125 and 80 mgActive substance: aprepitantManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: CAPSULE, 125 mgActive substance: aprepitantManufacturer: Qilu Pharma Spain S.L.Prescription requiredDosage form: CAPSULE, 125 mg/80 mgActive substance: aprepitantManufacturer: Qilu Pharma Spain S.L.Prescription required
Online doctors for EMEND 125 mg POWDER FOR ORAL SUSPENSION
Discuss questions about EMEND 125 mg POWDER FOR ORAL SUSPENSION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions