
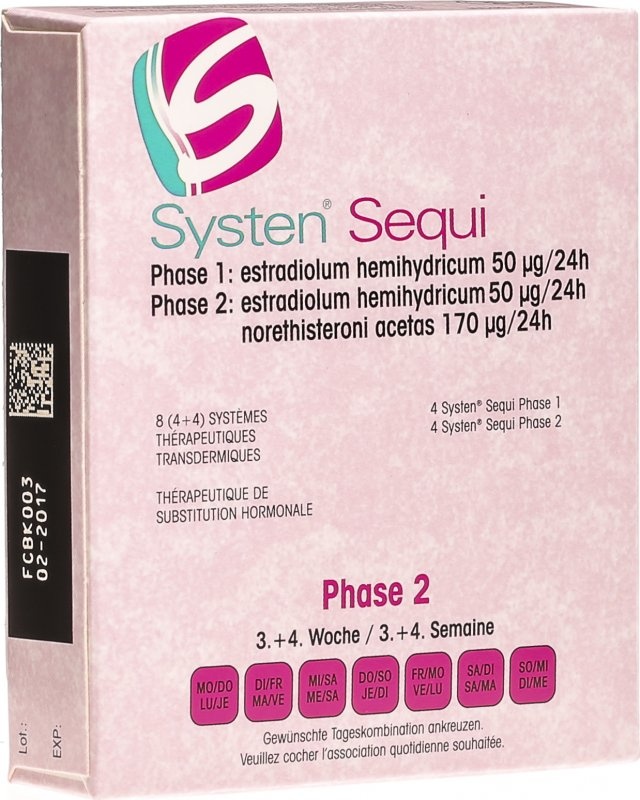
Sisten Sequi
Ask a doctor about a prescription for Sisten Sequi

How to use Sisten Sequi
Leaflet accompanying the packaging: information for the user
SYSTEN SEQUI:
Systen 50; 3.2 mg, transdermal system, patch
Estradiol
Systen Conti; 3.2 mg + 11.2 mg, transdermal system, patch
Estradiol + Norethisterone acetate
You should carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient.
- You should keep this leaflet, so that you can read it again if you need to.
- If you have any doubts, you should consult a doctor or pharmacist.
- This medicine has been prescribed specifically for you. Do not pass it on to others. The medicine may harm another person, even if their symptoms are the same.
- If the patient experiences any side effects, including any not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet:
1 .What is Systen Sequi and what is it used for.
- 2. Important information before using Systen Sequi.
- 3. How to use Systen Sequi.
- 4. Possible side effects.
- 5. How to store Systen Sequi.
- 6. Contents of the packaging and other information.
1. What is Systen Sequi and what is it used for
Each package of Systen Sequi contains 4 transdermal systems, Systen 50 patches, and 4 transdermal systems, Systen Conti patches.
Systen Sequi is a medicine used in hormone replacement therapy (HRT). It is a transdermal system in the form of a patch, for application to the skin. It contains estradiol, a female hormone belonging to estrogens, and norethisterone acetate, which is a progestogen. The estradiol in the medicine is identical to the hormone naturally produced by the ovaries in women before menopause.
Systen Sequi is used to:
relieve symptoms associated with menopause
During menopause, the amount of estrogen produced in a woman's body decreases, which can cause symptoms such as a feeling of heat on the face, neck, and chest ("hot flashes"), sleep problems, irritability, and depression. Systen Sequi relieves these symptoms associated with menopause. Systen Sequi may be prescribed to a patient only if the symptoms significantly interfere with her daily life.
Experience in treating women over 65 years of age is limited.
2. Important information before using Systen Sequi
Medical history and regular medical examinations
The use of HRT involves risks that should be considered when a patient decides whether to use hormone replacement therapy or continue its use.
Experience in treating women in premature menopause (due to ovarian failure or surgical procedure) is limited. If a patient is experiencing premature menopause, the risk associated with HRT may differ. You should talk to your doctor.
Before starting (or resuming) HRT, the doctor should take a medical history, including a family history. The doctor may decide to perform tests, including a breast examination and/or a gynecological examination, if necessary.
If a patient starts using Systen Sequi, she should regularly undergo medical examinations (at least once a year). During these examinations, she should discuss with her doctor the benefits and risks of continuing to use Systen Sequi.
The patient should regularly undergo breast examinations, in accordance with the doctor's recommendations.
When not to use Systen Sequi:
In case of any of the following diseases or in case of doubt, you should tell your doctorbefore using Systen Sequi.
Do not start using Systen Sequi:
- if you are allergic to estradiol, norethisterone acetateor any of the other ingredients of this medicine (listed in section 6);
- if you have or have had breast canceror if it is suspected;
- if you have or are suspected of having an estrogen-dependent tumor(e.g. endometrial cancer);
- if you have untreated endometrial hyperplasia(excessive growth of the endometrium)
- endometrial hyperplasia;
- if you have unexplained vaginal bleeding;
- if you are pregnant or breastfeeding;
- if you have or have had liver disease, and liver function test results have not returned to normal;
- if you have or have had blood clots in the veins(venous thromboembolic disease, e.g. deep vein thrombosis, pulmonary embolism);
- if you have blood coagulation disorders(deficiency of protein C, protein S, or antithrombin);
- if you have or have had arterial thromboembolic disorders(e.g. stroke, angina pectoris, myocardial infarction);
- if you have a rare, inherited blood disease - porphyria.
If any of the above conditions occur for the first time during the use of Systen Sequi, you should stop using it and consult a doctor.
Warnings and precautions
Before starting treatment, you should inform your doctor about any of the following diseases that you have had, as they may recur or worsen during the use of Systen Sequi.
In such a case, your doctor may decide that you need more frequent monitoring:
- uterine fibroids;
- endometriosis (presence of fragments of the endometrium in atypical locations for this tissue) or endometrial hyperplasia (excessive growth of the endometrium) in the past;
- increased risk of blood clots (see below "Blood clots in the veins (venous thromboembolic disease)");
- thromboembolic disorders in the history or presence of risk factors for these disorders;
- increased risk of estrogen-dependent tumors, e.g. breast cancer in the mother, sister, or grandmother;
- hypertension;
- liver disease (e.g. liver tumor);
- diabetes;
- gallstones;
- migraine or (severe) headaches;
- immune system disease affecting many organs (systemic lupus erythematosus);
- epilepsy;
- asthma;
- otosclerosis (ear disease leading to gradual hearing loss);
- mastopathy
- high triglyceride levels in the blood;
- fluid retention due to impaired heart or kidney function;
- a condition in which the thyroid gland does not produce enough thyroid hormones (hypothyroidism) and the patient is taking thyroid hormone replacement therapy;
- a hereditary and acquired condition that causes recurring episodes of swelling (hereditary and acquired angioedema) or a history of sudden swelling of the hands, face, feet, lips, eyes, tongue, throat (respiratory tract obstruction) or gastrointestinal tract.
In case of the following diseases during the use of HRT, you should stop using Systen Sequi and immediately consult a doctor:
- if any of the conditions listed in the "When not to use Systen Sequi" section occur;
- if the skin or whites of the eyes turn yellow (jaundice), which may be a sign of liver function disorders;
- significant increase in blood pressure (symptoms may include: headache, fatigue, and dizziness);
- if a migraine-type headache occurs for the first time;
- if pregnancy is detected;
- if facial swelling, tongue, and/or throat swelling and/or difficulty swallowing or hives occur, along with difficulty breathing, suggesting angioedema;
- if symptoms of blood clots occur, such as:
- painful swelling and redness of the lower limbs,
- sudden chest pain,
- breathing difficulties. For more information, see the section "Blood clots in the veins (venous thromboembolic disease)".
Note:Systen Sequi is not a contraceptive. If it has been less than 12 months since the last menstrual period or the patient is under 50 years of age, additional contraception may be necessary. You should talk to your doctor.
Hormone replacement therapy and cancer
Endometrial hyperplasia (excessive growth of the endometrium) and endometrial cancer
The use of only estrogens in HRT increases the risk of endometrial hyperplasia and endometrial cancer.
The progestogen in Systen Sequi helps reduce this additional risk.
Comparison
In women aged 50-65 with an intact uterus who do not use HRT, endometrial cancer is diagnosed in an average of 5 out of 1000 women.
In women aged 50-65 with an intact uterus who use estrogen-only HRT, the number of cases ranges from 10 to 60 per 1000 women, depending on the duration of treatment and the dose of estrogen used (i.e. from 5 to 55 additional cases).
Irregular bleeding
During the first 3 to 6 months of using Systen Sequi, irregular bleeding or spotting may occur. However, if irregular bleeding:
- persists for more than 6 months;
- occurs after using Systen Sequi for more than 6 months;
- persists after stopping Systen Sequi; you should consult a doctor as soon as possible.
Breast cancer
Data confirm that taking hormone replacement therapy (HRT) in the form of a combination of estrogen and progestogen or estrogen alone increases the risk of breast cancer. The additional risk depends on how long the patient uses HRT. This additional risk becomes apparent after 3 years of HRT use. After stopping HRT, the additional risk will decrease over time, but the risk may persist for 10 years or more if HRT lasted more than 5 years.
Comparison
In the case of women aged 50-54 who do not use HRT, breast cancer is diagnosed in an average of 13 to 17 out of 1000 women over a period of 5 years.
In the case of women aged 50 who start 5-year estrogen-only HRT, the number of cases is 16-17 per 1000 patients (i.e. 0 to 3 additional cases).
In the case of women aged 50 who start 5-year combined estrogen-progestogen HRT, the number of cases is 21 per 1000 patients (i.e. 4 to 8 additional cases).
In the case of women aged 50-59 who do not use HRT, breast cancer is diagnosed in an average of 27 out of 1000 women over a period of 10 years.
In the case of women aged 50 who start 10-year estrogen-only HRT, the number of cases is 34 per 1000 patients (i.e. 7 additional cases).
In the case of women aged 50 who start 10-year combined estrogen-progestogen HRT, the number of cases is 48 per 1000 patients (i.e. 21 additional cases).
You should regularly examine your breasts. You should consult a doctor if you notice any of the following changes:
- wrinkling of the skin;
- changes in the nipple;
- any noticeable or palpable lumps.
In addition, it is recommended to participate in offered breast cancer screening programs.
It is important to inform the nurse or medical staff performing the X-ray examination that you are taking hormone replacement therapy, as this medicine may increase breast density, which can affect the result of the mammogram. Not all lumps can be detected during a mammogram in areas with increased breast density.
Ovarian cancer
Ovarian cancer is less common than breast cancer. In some epidemiological studies, during long-term (at least 5 to 10 years) use of hormone replacement therapy, including only estrogens, in women after hysterectomy, an increased risk of ovarian cancer was found. Some studies, including the WHI study, suggest that long-term use of combined HRT may cause similar or slightly lower risk.
Hormone replacement therapy and its effect on the heart and circulation
Blood clots in the veins (venous thromboembolic disease)
The use of HRT is associated with an increased risk of developing venous thromboembolic disease, i.e. deep vein thrombosis or pulmonary embolism.
Studies have shown a 2-3-fold increase in the risk of venous thromboembolic disease in women taking hormone replacement therapy compared to women who do not use it.
The occurrence of this complication is more likely in the first year of HRT use than later.
Blood clots can be life-threatening and if they move to the lungs, they can cause chest pain, shortness of breath, loss of consciousness, and even death.
The risk of blood clots in the veins is higher if you are older and if you have any of the following factors. You should inform your doctor if:
- you are unable to walk for a long time due to severe injuries or surgical procedures (see section 3. If surgery is planned);
- you are obese (body mass index - BMI >30 kg/m);
- you have thromboembolic disorders that require long-term use of anticoagulant medications;
- any of your close relatives have had blood clots in the past;
- you have systemic lupus erythematosus.
If symptoms of blood clots occur, see In case of the following diseases during the use of HRT, you should stop using Systen Sequi and immediately consult a doctor.
There is no consensus on the potential role of varicose veins in venous thromboembolic disease.
Women already taking anticoagulant therapy should discuss the balance of benefits and risks of HRT with their doctor.
If, after starting treatment, you experience, for example, painful swelling of a limb, sudden chest pain, shortness of breath, which may be symptoms of venous thromboembolic disease, you should stop using the medicine and immediately consult a doctor.
Hormone replacement therapy and coronary heart disease
There is no evidence that HRT prevents myocardial infarction.
In women over 60 years of age who use combined estrogen-progestogen HRT, the risk of coronary heart disease is slightly higher than in women who do not use HRT.
Hormone replacement therapy and stroke
The risk of stroke is about 1.5 times higher in women using HRT compared to women who do not use it. The number of additional cases of stroke caused by HRT will increase with age.
Comparison
In women aged 50-59 who do not use HRT, the estimated number of stroke cases over 5 years is 8 per 1000 women. In women aged 50-59 who use HRT, the number of cases over 5 years is 11 per 1000 women (i.e. 3 additional cases).
Conditions requiring observation during estrogen therapy:
- liver disorders or mild liver failure;
- jaundice with bile stasis in the history;
- HRT does not improve cognitive function. There is evidence of an increased risk of probable dementia in women starting continuous, combined, or estrogen-only therapy at an age over 65. In women with an intact uterus taking unopposed estrogen therapy, an increased risk of endometrial hyperplasia and endometrial cancer has been found. Therefore, to reduce the risk of hyperplasia and endometrial cancer in women with an intact uterus, it is recommended to administer estrogen in combination with a progestogen, as in the case of Systen Sequi. Systen Sequi should be kept out of the reach of children and pets.
Children and adolescents
Systen Sequi should not be used in children.
Systen Sequi and other medicines
Some medicines may affect the efficacy of Systen Sequi, which can lead to irregular bleeding. These include:
- antiepileptic drugs (such as phenobarbital, phenytoin, and carbamazepine),
- antitubercular drugs (such as rifampicin, rifabutin),
- drugs used in HIV infection (such as nevirapine, efavirenz, ritonavir, and nelfinavir),
- drugs used in the treatment of hepatitis C virus (such as telaprevir)
- herbal products containing St. John's wort (Hypericum perforatum).
Hormone replacement therapy may affect the action of other medicines:
- antiepileptic drugs (lamotrigine), as it may increase the frequency of seizures.
- drugs used in the treatment of hepatitis C virus (HCV) such as treatment regimens using ombitasvir/paritaprevir/ritonavir and dasabuvir with ribavirin or without ribavirin, using glecaprevir/pibrentasvir or sofosbuvir/velpatasvir/voxilaprevir may cause an increase in liver enzyme parameters in laboratory blood tests (increased ALT enzyme activity) in women using combined hormonal contraceptives containing ethinyl estradiol. Systen Sequi contains estradiol instead of ethinyl estradiol. It is not known whether increased ALT enzyme activity may occur when using Systen Sequi with such a treatment regimen.
You should tell your doctor about all medicines you are currently taking or have recently taken, as well as any medicines you plan to take. Your doctor will provide you with appropriate instructions.
Lab tests
If a blood test is necessary, you should inform your doctor or laboratory staff that you are taking Systen Sequi, as this medicine may affect the results of some tests, e.g. glucose tolerance test or thyroid function tests.
Pregnancy and breastfeeding
Systen Sequi is contraindicated in pregnancy. If pregnancy is detected during the use of the medicine, it should be stopped immediately.
The use of Systen Sequi is contraindicated during breastfeeding.
Driving and using machines
No studies have been conducted on the effect of Systen Sequi on the ability to drive vehicles or operate machinery.
3. How to use Systen Sequi
This medicine should always be used as directed by your doctor. If you have any doubts, you should consult your doctor.
HRT should be continued only as long as the benefits of relieving severe symptoms outweigh the risks of HRT use.
Your doctor should prescribe the lowest possible dose for use for the shortest possible time to ensure symptom relief. If you think the dose of the medicine is too high or too low, you should consult your doctor.
Dosage
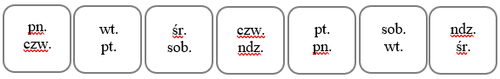
Systen 50 and Systen Conti patches should be applied to the skin of the trunk below the waist in the following sequence: first, two Systen 50 patches, one every 3 or 4 days, for 2 weeks (4 Systen 50 patches will be used in 2 weeks), then one Systen Conti patch, changing them at the same time intervals (4 Systen Conti patches will be used in the next 2 weeks). After 4 weeks, all patches from the package will be used, and a new package should be started.
The cycle of patch changes should be repeated without interruption.
For example, if the application of the first patch is on Monday, it should be replaced on Thursday, and then on the next Monday. The days can be determined based on the following table, starting from the first day of patch application:
| Day of application of the first patch | Day of patch replacement | Day of next patch replacement | ||
| Monday | → | Thursday | → | Monday |
| Tuesday | → | Friday | → | Tuesday |
| Wednesday | → | Saturday | → | Wednesday |
| Thursday | → | Sunday | → | Thursday |
| Friday | → | Monday | → | Friday |
| Saturday | → | Tuesday | → | Saturday |
To make it easier to remember the days of patch replacement, you can mark their configuration in the designated place on the package:
| Sunday | → | Wednesday | → | Sunday |
Do not remove the patch during bathing or showering. However, it is recommended to remove the patch before using a sauna, and after the sauna, apply a new patch immediately.
Using a higher dose of Systen Sequi than recommended
In case of using a higher dose of Systen Sequi than recommended, you should immediately consult a doctor or pharmacist.
Symptoms of overdose of combined estrogen and progestogen therapy may include: nausea, intermenstrual bleeding, breast pain and tenderness, abdominal cramps, and bloating. The mentioned symptoms are temporary and disappear after the patch is removed.
Missing a dose of Systen Sequi
If you forget to replace a patch, you should apply the missed patch as soon as possible. However, you should keep the same patch replacement schedule. Forgetting to use the medicine may increase the likelihood of bleeding and intermenstrual spotting.
If surgery is planned
If you are planning to have surgery, you should tell your surgeon that you are taking Systen Sequi. It may be necessary to stop using Systen Sequi 4 to 6 weeks before surgery to minimize the risk of blood clots (see section 2. Blood clots in the veins (venous thromboembolic disease)). Before resuming Systen Sequi, you should consult your doctor.
4. Possible side effects
Like all medicines, Systen Sequi can cause side effects, although not everybody gets them.
In women using HRT, there is an increased risk of developing the following diseases compared to women who do not use HRT:
- breast cancer;
- endometrial hyperplasia or cancer (excessive growth of the endometrium or endometrial cancer);
- ovarian cancer;
- blood clots in the veins of the legs or lungs (venous thromboembolic disease);
- coronary heart disease;
- stroke;
- possibly dementia if HRT is started at an age over 65.
For more information, see section 2 "Important information before using Systen Sequi".
The following side effects have been observed in clinical trials and reported after the marketing of Systen Sequi.
Very common(may affect more than 1 in 10 people):
- redness at the application site, itching at the application site, rash at the application site, reaction at the application site.
Common(may affect up to 1 in 10 people):
- depression, insomnia, emotional instability, nervousness;
- migraine, headache;
- hypertension;
- abdominal pain, gastrointestinal disorders, diarrhea, bloating, nausea;
- itching, rash;
- joint pain, back pain, muscle pain;
- breast pain, painful menstruation, heavy menstrual bleeding, menstrual disorders;
- pain, swelling, malaise;
- weight gain.
Uncommon(may affect up to 1 in 100 people):
- thrush;
- breast cancer, breast fibroadenoma;
- hypersensitivity (allergy);
- decreased libido, increased libido;
- dizziness, paresthesia, concentration disorders;
- palpitations;
- breast enlargement, endometrial hyperplasia (excessive growth of the endometrium), uterine bleeding;
- edema, fatigue.
Frequency not known(frequency cannot be estimated from the available data)
- endometrial cancer;
- mood swings;
- cerebrovascular incident, epilepsy;
- deep vein thrombosis, thrombosis;
- pulmonary embolism,
- abdominal distension,
- gallstones,
- rash, Stevens-Johnson syndrome,
- breast enlargement;
- peripheral edema, swelling at the application site.
* Additional side effects reported in clinical trials of Systen 50 (containing only estradiol).
Other side effects associated with oral estrogen-progestogen replacement therapy:
- dizziness;
- varicose veins;
- nausea, vomiting;
- limb pain, myasthenia;
- breast tenderness, uterine cramps, vaginal infection;
- uterine fibroids, ovarian cyst, endocervical polyps;
- increased liver enzyme activity - transaminases - in laboratory blood tests;
- gallbladder disease, jaundice;
- skin and subcutaneous tissue disorders: chloasma, erythema multiforme, erythema nodosum, purpura, acne, dry skin, alopecia;
- possible dementia in women over 65 years of age;
- dry eye syndrome;
- change in tear composition.
Reporting side effects
If you experience any side effects, including any not listed in this leaflet, you should tell your doctor or pharmacist. Side effects can be reported directly to the Department of Drug Safety Monitoring of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products
Al. Jerozolimskie 181C
02-222 Warsaw
Phone: +48 22 49 21 301
Fax: +48 22 49 21 309
Website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Systen Sequi
Store at a temperature not exceeding 25°C.
The medicine should be kept out of sight and reach of children.
This recommendation also applies to used patches.
Do not use Systen Sequi after the expiry date stated on the packaging.
The expiry date (EXP) means the last day of the specified month.
6. Contents of the packaging and other information
What Systen Sequi contains
Systen Sequi is a transdermal system, a patch consisting of:
4 transdermal systems, Systen 50 patches, each containing as an active substance:
- 3.2 mg of estradiol (Estradiol), in the form of estradiol hemihydrate;
4 transdermal systems, Systen Conti patches, each containing as active substances:
- 3.2 mg of estradiol (Estradiol), in the form of estradiol hemihydrate;
- 11.2 mg of norethisterone acetate (Norethisterone acetate).
Other ingredients of the medicine are:
- Adhesive layer: acrylic copolymer, guar gum.
- Protective layer (outer protective layer): polyester.
- Protective layer (to be removed): polyethylene terephthalate.
What Systen Sequi looks like and what the package contains
8 transdermal systems, patches (4 transdermal systems, Systen 50 patches, and 4 transdermal systems, Systen Conti patches) enclosed in foil sachets placed in a cardboard box.
The Systen 50 transdermal system, patch, with an area of 16 cm, contains 3.2 mg of estradiol and releases 50 μg of estradiol over 24 hours.
The Systen Conti transdermal system, patch, with an area of 16 cm, contains 3.2 mg of estradiol, which corresponds to the nominal release of 50 μg of estradiol over 24 hours, and 11.2 mg of norethisterone acetate, which is released in a nominal amount of 170 μg over 24 hours.
Marketing authorization holder:
Theramex Ireland Limited
3rd Floor, Kilmore House,
Park Lane, Spencer Dock,
Dublin 1
D01 YE64
Ireland
Manufacturer:
Aesica Pharmaceuticals GmbH
Alfred-Nobel-Str. 10
40789 Monheim am Rhein
Germany
To obtain more detailed information, you can contact the local representative of the marketing authorization holder at phone number: 22 307 71 66.
Date of last revision of the leaflet:August 2025
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterAesica Pharmaceuticals GmbH
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Sisten SequiDosage form: Gel, 0.5 mgActive substance: estradiolManufacturer: Orion CorporationPrescription requiredDosage form: Gel, 1 mgActive substance: estradiolManufacturer: Orion CorporationPrescription requiredDosage form: Gel, 1 mg/gActive substance: estradiolPrescription required
Alternatives to Sisten Sequi in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Sisten Sequi in Spain
Alternative to Sisten Sequi in Ukraine
Online doctors for Sisten Sequi
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Sisten Sequi – subject to medical assessment and local rules.










