
Rivastigmine Milan
Ask a doctor about a prescription for Rivastigmine Milan

How to use Rivastigmine Milan
Package Leaflet: Information for the User
Rivastigmine Mylan, 4.6 mg/24 h, transdermal system, patch
Rivastigmine Mylan, 9.5 mg/24 h, transdermal system, patch
Rivastigmine
Read the package leaflet carefully before using the medicine, as it contains important information for the patient.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If you experience any side effects, including any not listed in this leaflet, tell your doctor or pharmacist. See section 4.
Table of Contents of the Leaflet
- 1. What is Rivastigmine Mylan and what is it used for
- 2. Important information before using Rivastigmine Mylan
- 3. How to use Rivastigmine Mylan
- 4. Possible side effects
- 5. How to store Rivastigmine Mylan
- 6. Contents of the pack and other information
1. What is Rivastigmine Mylan and what is it used for
The active substance of Rivastigmine Mylan is rivastigmine.
Rivastigmine belongs to a group of substances called cholinesterase inhibitors. In patients with Alzheimer's disease, there is a decrease in the number of nerve cells in the brain, which leads to a decrease in the production of acetylcholine, a neurotransmitter (a substance that enables nerve cells to communicate with each other). Rivastigmine works by blocking the enzymes that break down acetylcholine: acetylcholinesterase and butyrylcholinesterase. By blocking the action of these enzymes, rivastigmine increases the concentration of acetylcholine in the brain, which helps to alleviate the symptoms of Alzheimer's disease.
Rivastigmine Mylan is used to treat adult patients with mild to moderately severe Alzheimer's disease, a progressive brain disease that gradually disrupts memory, intellectual abilities, and behavior.
2. Important information before using Rivastigmine Mylan
When not to use Rivastigmine Mylan
- if the patient is allergic to rivastigmine (the active substance of Rivastigmine Mylan) or any of the other ingredients of this medicine (listed in section 6);
- if the patient has an allergic reaction to similar medicines (carbamate derivatives);
- if the patient has a skin reaction that extends beyond the area of skin covered by the patch, if the local reaction has worsened (e.g., blisters, exacerbation of skin inflammation, swelling) or if these changes have not resolved within 48 hours after removal of the patch.
If any of these situations apply to the patient, they should inform their doctor and not apply the Rivastigmine Mylan patch.
Warnings and precautions
Before starting treatment with Rivastigmine Mylan, the patient should discuss with their doctor or pharmacist if:
- the patient has or has had heart disease, such as irregular or slow heart rhythm, prolonged QT interval, family history of prolonged QT interval, torsades de pointes, or low potassium or magnesium levels in the blood;
- the patient has heart failure;
- the patient has had a heart attack;
- the patient has or has had decreased potassium or magnesium levels in the blood;
- the patient has or has had an active stomach ulcer;
- the patient has or has had difficulty urinating;
- the patient has or has had seizures;
- the patient has or has had asthma or severe respiratory disease;
- the patient has muscle tremors;
- the patient has a low body weight;
- the patient has gastrointestinal reactions, such as nausea (vomiting), vomiting, and diarrhea. The patient may become dehydrated (lose too much fluid) if vomiting or diarrhea persists for a longer period;
- the patient has liver function disorders.
If any of these situations apply to the patient, closer monitoring by the doctor may be necessary during treatment with this medicine.
Children and adolescents
Rivastigmine Mylan should not be used in children and adolescents for the treatment of Alzheimer's disease.
Rivastigmine Mylan and other medicines
The patient should tell their doctor or pharmacist about all medicines they are taking or have recently taken, as well as any medicines they plan to take, including those available without a prescription.
Rivastigmine Mylan may enhance the effects of certain medicines that lower blood pressure, such as beta-blockers (e.g., atenolol), calcium channel blockers (e.g., amlodipine, nifedipine), anti-arrhythmic medicines (e.g., sotalol, amiodarone), digitalis glycosides, and pilocarpine (used to treat glaucoma). This may lead to fainting.
Caution should be exercised when Rivastigmine Mylan is used with other medicines that may affect heart rhythm or the heart's conduction system (prolonged QT interval).
If the patient is taking any of the following medicines, the doctor may perform regular heart checks to ensure that the heart is working properly:
- medicines used to treat mental disorders, known as antipsychotics, e.g., chlorpromazine, levomepromazine, sulpiride, amisulpride, tiapride, veralipride, pimozide, haloperidol, droperidol,
- cisapride (used to treat indigestion),
- citalopram (used to treat depression),
- difemanil (used to treat stomach ulcers),
- halofantrine (used to treat malaria),
- mizolastine (used to treat allergies),
- methadone (a pain-relieving medicine, also used for heroin addiction),
- erythromycin IV, pentamidine, moxifloxacin (antibiotics).
Rivastigmine Mylan may affect the action of anticholinergic medicines, some of which are used to relieve stomach cramps (e.g., dicyclomine), to treat Parkinson's disease (e.g., amantadine), to treat overactive bladder (e.g., oxybutynin, tolterodine), or to prevent motion sickness (e.g., diphenhydramine, scopolamine, or meclizine).
Rivastigmine Mylan transdermal system should not be used at the same time as metoclopramide (a medicine used to relieve or prevent nausea and vomiting).
Taking these two medicines together may cause disorders such as stiffness of the limbs and hand tremors.
If the patient is to undergo surgery during treatment with Rivastigmine Mylan, they should inform their doctor, as it may be necessary to stop treatment, as it may enhance the effects of certain muscle relaxants used during anesthesia.
Pregnancy and breastfeeding
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a child, they should consult their doctor or pharmacist before using this medicine.
If the patient is pregnant, the benefits of using Rivastigmine Mylan should be weighed against the potential effects of the medicine on the unborn child. Rivastigmine Mylan should not be used during pregnancy unless absolutely necessary.
The patient should not breastfeed while using Rivastigmine Mylan.
Driving and using machines
The doctor will inform the patient whether their condition allows them to drive or use machines safely. Rivastigmine Mylan may cause fainting or severe dizziness. If the patient feels weak or disoriented, they should not drive, operate machinery, or perform other tasks that require concentration.
3. How to use Rivastigmine Mylan
This medicine should always be used exactly as the doctor or pharmacist has instructed. If the patient is unsure, they should ask their doctor or pharmacist.
IMPORTANT:
- Before applying ONE NEW PATCH, remove the previous patch.
- Use only ONE Rivastigmine Mylan patch per day.
- Do not cut the patch into smaller pieces.
- Press the patch firmly with the palm of your hand for at least
30 seconds.
- Avoid touching your eyes after applying the patch.
How to start treatment
The doctor will inform the patient which Rivastigmine Mylan patches are best for their condition.
- Treatment usually starts with Rivastigmine Mylan 4.6 mg/24 h.
- The recommended, usually used daily dose of Rivastigmine Mylan is 9.5 mg/24 h. If the patient's condition does not improve after at least 6 months, the doctor may consider increasing the dose to 13.3 mg/24 h (this dose cannot be achieved with this product). In cases where such a dose is required, the patient should ask their pharmacist for advice.
- Apply only one patch at a time and change it for a new one every 24 hours.
During treatment, the doctor may adjust the dose of the medicine to the individual patient's needs.
If the patient has not applied a patch for three days or more, they should not apply a new patch until they have spoken to their doctor, as they may be more likely to experience side effects. Treatment can be resumed using the same dose if the break in treatment does not exceed three days. Otherwise, the doctor may recommend continuing treatment with a dose of 4.6 mg/24 h Rivastigmine Mylan.
Where to apply the Rivastigmine Mylan patch
- Before applying the patch, make sure the skin in the area where the patch is to be applied is clean, dry, and hairless, free from powder, oils, creams, or lotions that could prevent the patch from sticking properly, free from cuts, rashes, and/or irritations,
- Remove any previously applied patches carefully before applying a new one.Applying multiple patches to the skin may expose the patient to too much medicine, which can be dangerous.
- Apply ONEpatch per day to ONLY ONEof the following areas, as shown in the diagrams:
- upper part of the left arm orupper part of the right arm
- upper part of the chest on the left side oron the right side (avoid applying patches to the breast)
- upper part of the back on the left side oron the right side
- lower part of the back on the left side oron the right side
After 24 hours, remove the old patch before applying ONE NEW PATCH to ONLY ONE of the indicated areas.
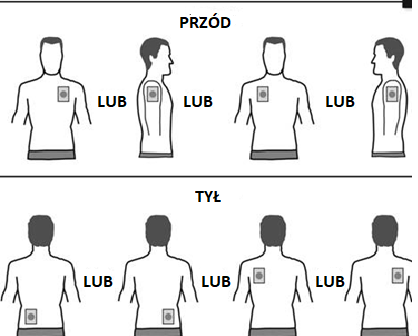
When changing the patch, remove the patch from the previous day before applying a new patch to a different area (e.g., one day on the right side of the body, the next day on the left, one day on the chest or upper part of the body, the next day on the lower part of the back). Do not apply a patch to the same area before 14 days have passed.
How the patient should apply the Rivastigmine Mylan patches
Rivastigmine Mylan is a thin, light-brown patch made of plastic, which is stuck to the skin. Each patch is in a sealed protective sachet. Do not open the sachet or remove the patch from the sachet until it is time to apply it to the skin.
Carefully remove the old patch before applying a new one.
Patients starting treatment (for the first time) and patients restarting treatment after a break should start with the actions shown in the second diagram.
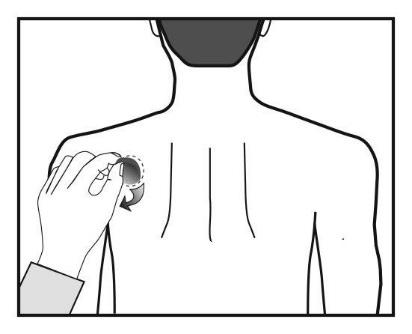
Each patch is in a sealed protective sachet. The sachet should be opened just before using the patch.
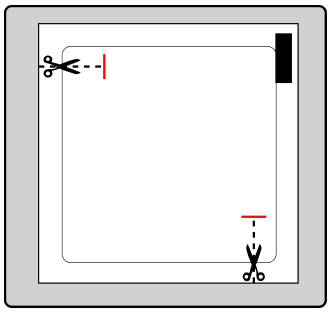
Cut the sachet at both marked points with scissors, but no further than the indicated line. Tear the sachet to open it. Do not cut the sachet along its entire length to avoid damaging the patch.
Remove the patch from the sachet.
Remove the protective backing (colored) from the top of the patch and discard it.
The adhesive side of the patch is protected by a protective layer.
Remove one part of the protective layer without touching the adhesive side of the patch.
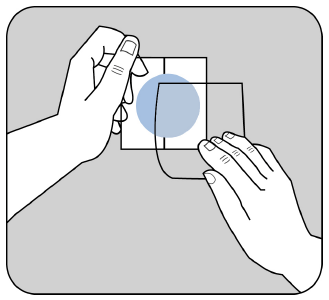
Apply the adhesive side of the patch to the upper or lower part of the back, upper part of the arm, or chest, and then remove the second part of the protective layer.
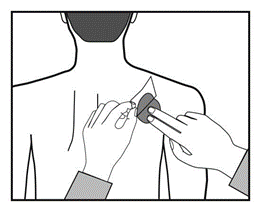
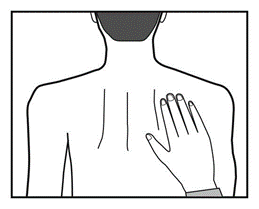
Press the patch firmly with your hand for at least 30 seconds, making sure the edges are well stuck to the skin.
You can now sign the patch with a pen, e.g., with the day of the week.
The patch should be worn continuously until it is time to change it for a new one. The patient can try different application sites for the new patch (choosing from the indicated areas) to find the most convenient and least exposed to abrasion by clothing.
How the patient should remove the Rivastigmine Mylan patch
Gently pull one edge of the patch and slowly peel it off the skin. If any adhesive residue remains on the skin, it can be removed by washing the area with warm water and mild soap or baby oil. Do not use alcohol or other solvents (nail polish remover or other products).
Washing hands
After removing or applying the patch, wash your hands with soap and water. If the medicine comes into contact with the eyes or if the eyes become red after contact with the patch, rinse them immediately with plenty of water, and if the symptoms do not disappear, consult a doctor.
Can the patient use Rivastigmine Mylan patches while bathing, swimming, or in the sun?
- Bathing, swimming, or showering should not affect the action of the patch. Make sure the patch does not come loose during these activities.
- Do not expose the patch to prolonged external heat sources (e.g., excessive sun exposure, sauna, solarium).
What to do if the patch comes off
If the patch comes off, apply a new one for the rest of the day, and then change it at the usual time the next day.
When and for how long should the patient use Rivastigmine Mylan patches
- To get the most out of the treatment, apply a new patch every day, preferably at the same time every day.
- Apply only one Rivastigmine Mylan patch at a time and change it for a new one every 24 hours.
What to do if the patient uses more Rivastigmine Mylan than they should
If the patient accidentally applies more than one patch, they should remove all patches and inform their doctor. The patient may need medical attention.
In some people who have accidentally taken too much rivastigmine, the following symptoms have occurred: decreased pupil size (miosis), skin redness, and a feeling of heat (hot flashes), abdominal pain, nausea, vomiting, diarrhea, slow heart rate, sudden breathing difficulties (bronchospasm), increased mucus production, increased sweating, loss of bladder control, crying, low blood pressure, increased saliva production, dizziness, tremors, headache, drowsiness, confusion, high blood pressure, hallucinations, and lack of energy. In severe cases, muscle weakness, muscle spasms, seizures, and slowing or stopping of breathing have been observed.
What to do if the patient forgets to use Rivastigmine Mylan
If the patient realizes they have forgotten to apply a patch, they should apply it immediately. The next patch can be applied at the usual time the next day. Do not apply two patches to make up for a missed dose.
What to do if the patient stops using Rivastigmine Mylan
If the patient stops using the medicine, they should inform their doctor or pharmacist.
If the patient does not apply a patch for three days or more, they should not start using a new patch before consulting their doctor, as they may be more likely to experience side effects.
If the patient has any further questions about using this medicine, they should ask their doctor or pharmacist.
4. Possible side effects
Like all medicines, Rivastigmine Mylan can cause side effects, although not everybody gets them.
Side effects are more common during the initial treatment period or when the dose is increased. Side effects usually disappear slowly as the body gets used to the treatment.
If the patient experiences any of the following side effects, they should remove the patch and tell their doctor immediately, as these effects can be serious:
- seizures
- changes in heart rhythm, which may be observed as very fast heart rate or feeling of missed heartbeats
- stomach ulcers - the patient may experience stomach pain and vomiting may contain fresh blood or look like coffee grounds
- pancreatitis - symptoms include severe pain in the upper part of the stomach, often with nausea or vomiting
- severe dizziness, which may be accompanied by seeing, hearing, or feeling things that do not exist (hallucinations), loss of contact with reality (delusions), and increased or decreased activity (delirium)
- liver function disorders - the patient may experience yellowing of the skin, eyes, abnormal darkening of urine, or unexplained nausea, vomiting, fatigue, and loss of appetite
Other side effects:
Common(may affect up to 1 in 10 people):
- headache
- loss of appetite, weight loss
- feeling anxious, depression, dizziness
- fainting
- nausea, vomiting, diarrhea, indigestion/heartburn, stomach pain
- agitation, fatigue, general weakness, fever
- skin rash and allergic skin reactions such as eczema-like reactions, redness, itching, swelling, and irritation
- urinary tract infection - may cause pain when urinating or more frequent urination than normal
- urinary incontinence - inability to hold urine
Uncommon(may affect up to 1 in 100 people):
- heart problems, such as slow heart rate
- dehydration (loss of too much fluid)
- hyperactivity (high level of activity, restlessness)
- aggression
Rare(may affect up to 1 in 1,000 people):
- fainting
Very rare(may affect up to 1 in 10,000 people):
- stiffness of the arms or legs, restlessness, muscle spasms, tremors, such as hand tremors
Frequency not known(frequency cannot be estimated from the available data):
- allergic reaction, such as blisters or skin inflammation, itching, hives, or redness
- worsening of Parkinson's disease symptoms - such as tremors, stiffness, drowsiness, and shuffling gait
- fast heart rate
- high blood pressure
- changes in liver function test results
- feeling anxious
- seeing or hearing things that do not exist (hallucinations)
- nightmares
Other side effects observed with rivastigmine capsules or oral solution, which may also occur with patches:
Common(may affect up to 1 in 10 people):
- general malaise
- feeling confused
- increased sweating
Rare(may affect up to 1 in 1,000 people):
- intestinal ulcer disease
- chest pain - may be caused by coronary artery spasm
Very rare(may affect up to 1 in 10,000 people):
- gastrointestinal bleeding - manifested as blood in the stool or vomit
Frequency not known(frequency cannot be estimated from the available data):
- severe vomiting, which may lead to rupture of the esophagus
Reporting side effects
If the patient experiences any side effects, including any not listed in this leaflet, they should tell their doctor or pharmacist. Side effects can be reported directly to the Department of Drug Safety Monitoring, Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, Tel.: +48 22 49 21 301, Fax: +48 22 49 21 309, website: https://smz.ezdrowie.gov.pl. Side effects can also be reported to the marketing authorization holder. By reporting side effects, more information can be gathered on the safety of this medicine.
5. How to store Rivastigmine Mylan
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date stated on the carton and sachet after "EXP". The expiry date refers to the last day of that month.
There are no special storage instructions for the medicinal product.
Before use, the patch should be stored in the sachet.
Do not use a patch that is damaged or shows signs of opening.
After removing the patch, fold it in half with the adhesive side inwards and press firmly. Put the used patch in the sachet and then dispose of it in a place inaccessible to children. After removing the patch, do not touch your eyes with your fingers before washing your hands with soap and water.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Contents of the pack and other information
What Rivastigmine Mylan contains
- The active substance is rivastigmine.
- Rivastigmine Mylan 4.6 mg/24 h transdermal systems: each patch releases 4.6 mg of rivastigmine over 24 hours. The patch has a surface area of 4.6 cm and contains 6.9 mg of rivastigmine.
- Rivastigmine Mylan 9.5 mg/24 h transdermal systems: each patch releases 9.5 mg of rivastigmine over 24 hours. The patch has a surface area of 9.2 cm and contains 13.8 mg of rivastigmine.
- Other ingredients are: 2-ethylhexyl acrylate copolymer and vinyl acetate, medium molecular weight polyisobutene, high molecular weight polyisobutene, anhydrous colloidal silica, light liquid paraffin
Outer layer:
Polyethylene/thermoplastic resin/Aluminum coated with polyester
Protective layer (removable):
Polyester coated with fluoropolymer
Orange ink
What Rivastigmine Mylan looks like and contents of the pack
Each transdermal system is a thin patch. On the outer, light-brown layer covering the patch, the following is printed in orange ink:
- “RIV-TDS 4.6 mg/24 h”
- “RIV-TDS 9.5 mg/24 h”
Each patch is in a separate, sealed sachet. The patches are available in packs of 7 or 30 sachets and in multipacks containing 60 or 90 sachets. Not all pack sizes may be marketed.
Marketing authorization holder
Viatris Limited
Damastown Industrial Park
Mulhuddart, Dublin 15
DUBLIN
Ireland
Manufacturer
McDermott Laboratories Ltd. T/A Gerard Laboratories T/A Mylan Dublin
35/36 Baldoyle Industrial Estate
Grange Road, Dublin 13
Ireland
Mylan Hungary Kft
H-2900 Komárom
Mylan utca 1
Hungary
Luye Pharma AG
Am Windfeld 35, 83714 Miesbach,
Germany
To obtain more detailed information on the medicine and its names in the Member States of the European Economic Area, the patient should contact the representative of the marketing authorization holder:
Viatris Healthcare Sp. z o.o.
Tel: +48 22 546 64 00
Date of last revision of the leaflet: May 2024
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterLuye Pharma AG McDermott Laboratories Limited t/a Gerard Laboratories t/a Mylan Dublin Mylan Hungary Kft.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Rivastigmine MilanDosage form: System, 4.6 mg/24 hActive substance: rivastigmineManufacturer: Luye Pharma AGPrescription requiredDosage form: System, 9.5 mg/24 hActive substance: rivastigmineManufacturer: Luye Pharma AGPrescription requiredDosage form: System, 4.6 mg/24 hActive substance: rivastigminePrescription required
Alternatives to Rivastigmine Milan in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Rivastigmine Milan in Hiszpania
Alternative to Rivastigmine Milan in Ukraina
Online doctors for Rivastigmine Milan
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Rivastigmine Milan – subject to medical assessment and local rules.











