Pulmicort


How to use Pulmicort
Leaflet accompanying the packaging: patient information
Pulmicort, 0.125 mg/ml, nebulizer suspension
Pulmicort, 0.250 mg/ml, nebulizer suspension
Pulmicort, 0.500 mg/ml, nebulizer suspension
Budesonide
You should carefully read the contents of this leaflet before using the medicine, as it contains important information for the patient.
- You should keep this leaflet, so that you can read it again if you need to.
- If you have any doubts, you should consult your doctor or pharmacist.
- This medicine has been prescribed specifically for you. Do not pass it on to others. The medicine may harm another person, even if their symptoms are the same as yours.
- If the patient experiences any side effects, including any side effects not listed in this leaflet, they should inform their doctor or pharmacist. See section 4.
Table of contents of the leaflet:
- 1. What is Pulmicort and what is it used for
- 2. Important information before using Pulmicort
- 3. How to use Pulmicort
- 4. Possible side effects
- 5. How to store Pulmicort
- 6. Contents of the packaging and other information
1. What is Pulmicort and what is it used for
Budesonide, the active substance of Pulmicort, belongs to a group of medicines called corticosteroids. Medicines in this group have local anti-inflammatory effects. Pulmicort is used:
- in patients with bronchial asthma who require long-term administration of corticosteroids to control the inflammatory process in the respiratory system. The cause of asthma is inflammation of the respiratory system. Nebulizers are recommended when the use of pressurized inhalers (pMDI) or powder inhalers (DPI) is unsatisfactory or unjustified.
- in patients with croup syndrome - acute laryngitis, tracheitis, and bronchitis - regardless of etiology, associated with significant narrowing of the upper airways, shortness of breath, or "barking" cough, leading to respiratory disorders.
- in the treatment of exacerbations of chronic obstructive pulmonary disease (COPD), when the use of budesonide in the form of a nebulizer suspension is justified. COPD is a chronic lung disease that causes shortness of breath and cough.
2. Important information before using Pulmicort
When not to use Pulmicort
- if the patient is hypersensitive (allergic) to budesonide or any of the other ingredients of Pulmicort (listed in section 6). The patient should inform their doctor about any worrying reactions that occurred after taking a medicine containing budesonide or any ingredient of Pulmicort.
Warnings and precautions
Pulmicort is intended for long-term treatment, but it does not provide quick relief of acute asthma attacks, in which the administration of short-acting bronchodilators is indicated. If there is no noticeable improvement after using short-acting bronchodilators or if they need to be used more frequently than usual, the patient should consult their doctor. In such cases, the doctor may consider using more effective anti-inflammatory treatment, for example, by increasing the dose of inhaled budesonide or starting treatment with an oral corticosteroid. Particular caution should be exercised when changing treatment from oral corticosteroids to inhaled products. During this period, transient adrenal insufficiency may occur. Patients who have required emergency treatment with high doses of oral corticosteroids or long-term treatment with the highest recommended doses of inhaled corticosteroids are also at increased risk of adrenal insufficiency when exposed to stressful situations. The patient should inform their doctor about anticipated stressful situations (e.g., exams) or planned surgical procedures. The doctor may consider increasing the dose of oral corticosteroids. Warning. If the treatment is changed from oral corticosteroids to Pulmicort in the form of a nebulizer suspension, the following symptoms may occur: runny nose, rash, muscle and joint pain. In the case of allergic reactions, such as runny nose or rash, the doctor may recommend treatment with antihistamines and/or local-acting medicines. If any of the symptoms are severe or worrying, or if symptoms such as headache, fatigue, nausea, or vomiting occur, the patient should contact their doctor. The doctor may recommend periodic increases in the dose of oral corticosteroids. Regular monitoring of growth in children and adolescents taking corticosteroids, regardless of the route of administration, is recommended due to the risk of growth retardation. If growth is slowed, the doctor may verify the treatment method by reducing the dose of corticosteroids. Before starting treatment, the patient should inform their doctor about other diseases or conditions, especially:
- active or recent infections,
- liver function disorders. The patient should also consult their doctor if the above warnings apply to past situations.
As with other inhaled medicines, paradoxical bronchospasm may occur immediately after using Pulmicort. If a severe reaction occurs, the patient should stop using the medicine immediately and consult their doctor without delay. When using inhaled corticosteroids, fungal infections of the mouth and throat may occur. These infections may require appropriate antifungal therapy and, in some patients, discontinuation of inhaled corticosteroids. The patient should also consult their doctor if the symptoms of the disease do not improve despite regular use of the recommended doses of the medicine. If the patient experiences blurred vision or other vision disturbances, they should contact their doctor.
Children
The medicine can be used to treat bronchial asthma in children from 6 months of age. The doctor will determine the dose of the medicine individually for each patient.
Pulmicort and other medicines
The patient should tell their doctor about all medicines they are currently taking or have recently taken, including those that are available without a prescription, as well as any medicines they plan to take. The patient should inform their doctor about any worrying reactions that have occurred after taking other medicines. In particular, the patient should inform their doctor about any antifungal medicines they are currently taking, such as ketoconazole or itraconazole (which are potent inhibitors of the CYP 3A4 isoenzyme), and HIV protease inhibitors, such as ritonavir and atazanavir, which may increase the concentration of budesonide in the blood. If concomitant use of such medicines with Pulmicort is necessary, the interval between doses of the individual medicines should be as long as possible, and the doctor may recommend reducing the dose of budesonide. No interactions have been observed between budesonide and other medicines used to treat bronchial asthma.
Pregnancy and breastfeeding
Pregnancy If the patient is pregnant or plans to become pregnant, they should consult their doctor before using the medicine - they should not use the medicine unless their doctor recommends it. If a woman being treated with Pulmicort becomes pregnant, she should not stop treatment on her own but should inform her doctor as soon as possible. Breastfeeding If the patient is breastfeeding, they should consult their doctor before using this medicine.
Driving and using machines
Pulmicort does not affect the ability to drive or use machines.
3. How to use Pulmicort
This medicine should always be used as directed by the doctor. The dosage of Pulmicort in the form of a nebulizer suspension is determined individually. If there are any doubts, the patient should consult their doctor again. Pulmicort in the form of a nebulizer suspension can only be used with a nebulizer (inhalation device). The medicine is introduced into the lungs during breathing through a mouthpiece or face mask. Before using the medicine, the patient should carefully read the "Instructions for using Pulmicort in the form of a nebulizer suspension" at the end of the leaflet and follow the instructions. The patient should remember to rinse their mouth with water after each inhalation. If a face mask was used, the patient should also wash their face after each inhalation. Not all inhalation devices (nebulizers) are suitable for administering Pulmicort in the form of a nebulizer suspension. Ultrasonic nebulizers should not be used.
Asthma
Initial dose
The recommended initial dose for children from 6 months of age is a total daily dose of 0.25 mg to 0.5 mg. If the child is taking an oral corticosteroid, the doctor may increase the daily dose to 1 mg if necessary. The recommended initial dose for adults and the elderly is 1 mg to 2 mg per day. The doctor may change the dosage after some time.
Maintenance dose
The smallest effective maintenance dose should be used. Children from 6 months of age: the total daily dose is 0.25 mg to 2 mg. Adults, including the elderly: the total daily dose is 0.5 mg to 4 mg. If the symptoms are very severe, the doctor may increase the dose of the medicine. If the daily dose is up to 1 mg, the medicine can be administered once a day in the morning or evening. If the patient feels that the effect of the medicine is too strong or too weak, they should consult their doctor. If the patient's condition improves, the doctor may decide to reduce the dose of the medicine. Improvement in the patient's condition after using Pulmicort may occur after several hours of starting treatment. The full therapeutic effect is achieved after several weeks of starting treatment. Pulmicort should be used even when there are no symptoms of the disease. Patients treated with oral corticosteroids Pulmicort in the form of a nebulizer suspension may be prescribed for a patient who is taking oral corticosteroids. Pulmicort in the form of a nebulizer suspension can partially or completely replace oral corticosteroids with the same or increased efficacy. The doctor should recommend a gradual reduction in the dose of the oral medicine. When changing treatment from oral corticosteroids to inhaled medicines, the patient should be in a stable condition. It is recommended to use high doses of Pulmicort in combination with the previously used oral corticosteroid at an unchanged dose for 10 days. Then, the dose of the oral corticosteroid should be gradually reduced by about 2.5 mg of prednisolone or an equivalent dose of another corticosteroid per month to the smallest dose that controls the symptoms of the disease. Often, the use of oral corticosteroids can be completely discontinued. Budesonide administered to the patient in the form of a nebulizer suspension is delivered to the lungs during inhalation. It is very important that the patient performs calm, even inhalations through the mouthpiece of the nebulizer or face mask.
Croup syndrome
The usual dose used in infants and children with croup syndrome is 2 mg of budesonide administered by nebulization. This dose can be administered in its entirety or divided into two doses of 1 mg each, administered 30 minutes apart. This dosing regimen can be repeated every 12 hours, up to 36 hours, or until the patient's condition improves.
COPD exacerbations
Based on limited clinical trial data, the recommended dose of Pulmicort, nebulizer suspension, is 4 to 8 mg per day, divided into 2 to 4 doses. Treatment should be continued until clinical improvement is achieved, but it is not recommended to continue treatment for more than 10 days. Method of administration Pulmicort can be mixed with 0.9% sodium chloride solution and solutions of terbutaline, salbutamol, fenoterol, acetylcysteine, sodium cromoglycate, or ipratropium. The prepared mixture should be used within 30 minutes. The dose in the plastic container can be divided to achieve the desired dose. The plastic containers, which are single-dose containers, are marked with a horizontal line (Pulmicort 0.25 mg/ml and 0.5 mg/ml). When the plastic container is turned upside down, this line indicates a volume of 1 ml. If only 1 ml is to be used, the liquid above the indicator line should be removed. The opened plastic container should be stored in a protective foil, protected from light. The contents of the opened container should be used within 12 hours. Dose (mg) Volume of Pulmicort nebulizer suspension 0.125 mg/ml 0.25 mg/ml 0.5 mg/ml 0.25 2 ml 1 ml*
- 0.5 4 ml 2 ml
- 0.75
- 3 ml
- 1.0
- 4 ml 2 ml 1.5
- 3 ml 2.0
- 4 ml *To be diluted to 2 ml with 0.9% sodium chloride solution or another recommended liquid.
Using a higher dose of Pulmicort than recommended
It is important that the patient uses the medicine as directed in the leaflet or as recommended by the doctor. The patient should not increase or decrease the dose of the medicine without consulting their doctor. If a higher dose of the medicine than recommended is taken, the patient should consult their doctor or pharmacist immediately. If a dose of Pulmicort higher than recommended is used once, it is unlikely to have harmful effects. If doses higher than those recommended by the doctor are taken for a longer period, there is a possibility of side effects, such as those that occur with oral corticosteroids, i.e., increased levels of adrenal hormones in the blood and suppression of adrenal function. In this case, the doctor should recommend continuing treatment with Pulmicort in doses that keep the symptoms of asthma under control.
Missing a dose of Pulmicort
If a dose of Pulmicort recommended by the doctor is missed, there is no need to make up for the missed dose. The patient should take the next dose of the medicine as directed by the doctor. The patient should not take a double dose to make up for the missed dose. If the patient has any further doubts about using this medicine, they should consult their doctor or pharmacist.
4. Possible side effects
Like all medicines, Pulmicort can cause side effects, although not everybody gets them.
If any of the following symptoms occur, the patient should stop using Pulmicort and consult their doctor immediately:
Pulmicort and consult their doctor immediately:
- swelling of the face, especially around the mouth, tongue, eyes, and ears, rash, itching, contact dermatitis, urticaria, and bronchospasm (constriction of the muscles in the airways, which causes wheezing). This may indicate an allergic reaction. This side effect is rare (less than 1 in 1,000 people).
- sudden onset of wheezing after inhaling the medicine. This side effect is rare (less than 1 in 1,000 people).
Other possible side effects:
Common (occurring in less than 1 in 10 people)
- thrush (fungal infections) in the mouth. To reduce the risk of this, the patient should rinse their mouth with water after using Pulmicort.
- sore throat, cough, and hoarseness, loss of voice.
- pneumonia (lung infection) in patients with COPD.
The patient should tell their doctor if they experience any of the following symptoms, which may be signs of a lung infection:
- fever or chills,
- increased production of mucus, change in the color of mucus,
- worsening cough or increased difficulty breathing.
Uncommon (occurring in less than 1 in 100 people)
- cataract (clouding of the lens of the eye).
- blurred vision.
- muscle cramps.
- muscle tremors.
- depression.
- anxiety.
Rare (occurring in less than 1 in 1,000 people)
- rash on the face after using a face mask. This can be prevented by washing the face with water after using the face mask.
- nervousness, changes in behavior (mainly in children).
- easy bruising.
- hoarseness and loss of voice (in children).
Side effects whose frequency is not known (frequency cannot be estimated from the available data):
- sleep disorders, anxiety, excessive excitement, aggression.
The use of inhaled corticosteroids may affect the normal production of steroid hormones in the body, especially if they are used for a long time in high doses. Side effects such as:
- glaucoma (increased intraocular pressure), frequency not known.
- growth retardation in children and adolescents (rare).
- effects on the adrenal glands (a small gland near the kidneys) (rare). The occurrence of these side effects after using inhaled corticosteroids is less likely than after taking oral corticosteroids.
Reporting side effects
If the patient experiences any side effects, including any side effects not listed in the leaflet, they should inform their doctor or pharmacist. Side effects can be reported directly to the Department of Drug Safety Monitoring of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products. Al. Jerozolimskie 181C 02-222 Warsaw tel.: +48 22 49 21 301 fax: +48 22 49 21 309 Website: https://smz.ezdrowie.gov.pl Side effects can also be reported to the marketing authorization holder. By reporting side effects, more information can be collected on the safety of the medicine.
5. How to store Pulmicort
The medicine should be stored out of sight and reach of children. This medicine should not be used after the expiry date stated on the packaging after "Expiry date (EXP)". The packaging should be stored at a temperature below 30°C, closed, and protected from light. The plastic single-dose containers must be stored in aluminum foil bags to protect them from light. After opening the aluminum foil bag, the medicine in the plastic single-dose containers is stable for 3 months. The contents of the plastic single-dose container should be used within 12 hours of opening. If only 1 ml of the suspension is used from the single-dose container, the remaining volume is not sterile. Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines they no longer need. This will help protect the environment.
6. Contents of the packaging and other information
What Pulmicort contains
- The active substance of Pulmicort is budesonide. 1 ml of the nebulizer suspension contains: 0.125 mg, 0.250 mg, or 0.500 mg of micronized budesonide. 1 plastic container contains 0.25 mg, 0.5 mg, or 1 mg of budesonide in 2 ml of nebulizer suspension.
- The other ingredients are: disodium edetate, sodium chloride, polysorbate 80, anhydrous citric acid, sodium citrate, purified water.
What Pulmicort looks like and contents of the packaging
A white to almost white liquid in a plastic single-dose container. 0.125 mg/ml, 0.250 mg/ml, 0.500 mg/ml: 20 plastic single-dose containers of 2 ml (4 aluminum foil bags with 5 plastic single-dose containers each) in a cardboard box. 0.250 mg/ml, 0.500 mg/ml: 5 plastic single-dose containers of 2 ml (1 aluminum foil bag with 5 plastic single-dose containers) in a cardboard box.
Marketing authorization holder and manufacturer
Marketing authorization holder: AstraZeneca AB S-151 85 Södertälje Sweden Manufacturer: AstraZeneca AB Forskargatan 18 SE-151 36 Södertälje Sweden For more detailed information, the patient should contact the representative of the marketing authorization holder: AstraZeneca Pharma Poland Sp. z o.o. ul. Postępu 14 02-676 Warsaw tel.: +48 22 245 73 00 fax: +48 22 485 30 07 Date of last revision of the leaflet:December 2022
Instructions for using Pulmicort in the form of a nebulizer suspension
- 1. Before using the contents of the plastic container, the patient should gently shake it in a circular motion.
- 2. The patient should hold the plastic container with the medicine upright (see diagram), and then open the container by twisting the "wing".
- 3. The open end of the container should be attached precisely to the nebulizer reservoir and slowly squeezed out.
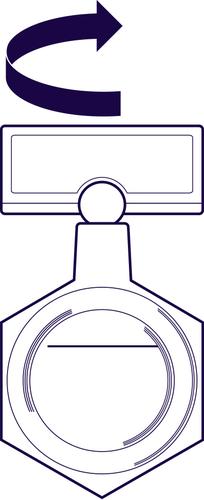
The plastic containers containing 0.25 mg/ml and 0.5 mg/ml are marked with a line indicating a volume of 1 ml when the container is turned upside down. If only 1 ml is to be used, the liquid above the indicator line should be removed. Before using the rest of the medicine, the patient should gently shake the container. The patient should write down the date of opening the aluminum foil bag. The plastic single-dose containers should not be used after 3 months from the date of opening the aluminum foil bag. The contents of the plastic single-dose container should be used within 12 hours of opening. The medicine should be stored at a temperature below 30°C. The plastic containers with the medicine should always be stored in an aluminum foil bag to protect them from light. If the entire contents of the plastic container are not used at once, the remaining amount should be protected from light. The plastic containers with the medicine should be stored upright.
WARNING
- 1. The patient should rinse their mouth after each use of the medicine.
- 2. If the patient uses a face mask, they should check that the mask fits tightly to their face during inhalation. The patient should wash their face after each use of the medicine.
CLEANING
The nebulizer chamber, mouthpiece, or face mask should be washed after each use. These parts should be washed with warm running water using a mild detergent recommended by the nebulizer manufacturer. The nebulizer chamber should then be rinsed well and dried by connecting the compressor to the outlet.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterAstraZeneca AB
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
Talk to a doctor online
Need help understanding this medicine or your symptoms? Online doctors can answer your questions and offer guidance.