

Pulmicort Turbuhaler

Ask a doctor about a prescription for Pulmicort Turbuhaler

How to use Pulmicort Turbuhaler
Leaflet accompanying the package: patient information
Pulmicort Turbuhaler, 100 μg/inhalation dose, inhalation powder
Pulmicort Turbuhaler, 200 μg/inhalation dose, inhalation powder
Budesonide
Read the leaflet carefully before using the medicine, as it contains important information for the patient.
- Keep this leaflet, so you can read it again if you need to.
- If you have any doubts, consult your doctor or pharmacist.
- This medicine has been prescribed specifically for you. Do not pass it on to others. The medicine may harm another person, even if their symptoms are the same as yours.
- If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet:
- 1. What is Pulmicort Turbuhaler and what is it used for
- 2. Important information before using Pulmicort Turbuhaler
- 3. How to use Pulmicort Turbuhaler
- 4. Possible side effects
- 5. How to store Pulmicort Turbuhaler
- 6. Package contents and other information
1. What is Pulmicort Turbuhaler and what is it used for
Budesonide, the active substance of Pulmicort Turbuhaler, belongs to a group of medicines called glucocorticosteroids. Medicines in this group have strong local anti-inflammatory effects. Pulmicort Turbuhaler is used in:
- bronchial asthma,
- chronic obstructive pulmonary disease (COPD).
2. Important information before using Pulmicort Turbuhaler
When not to use Pulmicort Turbuhaler
- if the patient is allergic (hypersensitive) to budesonide.
Warnings and precautions
Before starting treatment with Pulmicort Turbuhaler, the patient should inform their doctor if:
- they have pneumonia,
- they have a cold or chest infection or have breathing problems,
- they have ever had tuberculosis,
- they have liver problems,
- they have other diseases or conditions besides asthma.
The patient should inform their doctor about any planned stressful situations (e.g., exams) or planned surgeries. The doctor may then consider increasing the dose of oral glucocorticosteroids. If the patient experiences blurred vision or other vision disturbances, they should contact their doctor.
Children and adolescents
The medicine is intended for use in the treatment of bronchial asthma in children aged 6 and older. Regular monitoring of growth in children and adolescents taking glucocorticosteroids is recommended, regardless of the route of administration.
Using Pulmicort Turbuhaler in patients with kidney or liver function disorders
The patient should inform their doctor about any past or present liver function disorders.
Pulmicort Turbuhaler and other medicines
The patient should inform their doctor about any worrying reactions that occurred after taking other medicines. The patient should tell their doctor about all medicines they are currently taking or have recently taken, as well as any medicines they plan to take, including those that are available without a prescription and herbal preparations. Pulmicort Turbuhaler may affect the way some medicines work, and some medicines may affect the way Pulmicort Turbuhaler works. In particular, the patient should inform their doctor if they are taking:
- steroid medicines, including estrogens or steroid contraceptives,
- medicines used to treat fungal infections (such as ketoconazole and itraconazole),
- HIV protease inhibitors (such as ritonavir and nelfinavir).
Pregnancy and breastfeeding
Pregnancy If the patient is pregnant, thinks they may be pregnant, or plans to have a child, they should consult their doctor before using this medicine. If a woman treated with Pulmicort Turbuhaler becomes pregnant, she should inform her doctor as soon as possible. Breastfeeding Before using the medicine, the patient should consult their doctor.
Driving and using machines
Pulmicort Turbuhaler does not affect the ability to drive or use machines.
3. How to use Pulmicort Turbuhaler
- This medicine should always be used as directed by the doctor. If in doubt, the patient should consult their doctor.
Bronchial asthma
The dosage of Pulmicort Turbuhaler is individual. The following are general recommendations for determining the total initial dose, the maximum total dose of Pulmicort Turbuhaler, depending on previous asthma treatment and the patient's age. As with other inhaled medicines, a paradoxical bronchospasm may occur immediately after using Pulmicort Turbuhaler. If a severe reaction occurs, the patient should see their doctor immediately. The patient should also see their doctor if the symptoms of the disease do not improve despite systematic use of the recommended doses.
Children aged 6 and older
- 100 μg to 800 μg per day, in 2 to 4 divided doses.
- If the total daily dose is not more than 400 μg, it may be given once a day.
Adults
- The usual total daily dose is from 200 μg to 800 μg and may be given in 2 to 4 divided doses.
- In severe cases, the total daily dose may be up to 1600 μg.
- If the total daily dose is not more than 400 μg, it may be given once a day.
The lowest effective maintenance dose is recommended. Due to the very small amount of inhaled powder, the patient may not feel the taste of the medicine after inhalation. Improvement in clinical condition after administration of one dose of Pulmicort Turbuhaler can be expected after a few hours of inhalation. The full therapeutic effect is achieved after several weeks of treatment. Pulmicort Turbuhaler is intended for long-term treatment and does not provide quick relief of acute asthma attacks. When changing treatment from oral glucocorticosteroids to inhaled medicines, the patient should be in a relatively stable condition. For 10 days, it is recommended to use high doses of Pulmicort Turbuhaler in combination with the previously used oral glucocorticosteroid. Then, the dose of the oral glucocorticosteroid should be gradually reduced. Often, the use of oral glucocorticosteroids can be completely stopped.
Chronic obstructive pulmonary disease (COPD)
- The recommended dose of Pulmicort Turbuhaler is 400 μg given twice a day.
In the case of patients with COPD who are taking oral glucocorticosteroids and are prescribed Pulmicort Turbuhaler, the same recommendations should be followed as for "Bronchial asthma". In the event of worsening COPD symptoms, the patient should contact their attending physician, who will recommend appropriate treatment. If there is no noticeable improvement after using short-acting bronchodilators or if they need to be used more frequently than usual, the patient should see their doctor.
Preparing the Pulmicort Turbuhaler inhaler for the first use
Before the firstuse of a newPulmicort Turbuhaler inhaler, it should be prepared for use as follows:
- Remove the cap from the inhaler. When unscrewing, a characteristic rattling sound can be heard.
- Hold the Pulmicort Turbuhaler inhaler upright with the mouthpiece down.
- Turn the wheel one way until it clicks, then turn it the other way until it clicks (the direction you start turning the wheel does not matter). A characteristic click sound will be heard.
- Repeat the above step, turning the wheel in both directions.
- The Pulmicort Turbuhaler inhaler is now ready for use.
Using the inhaler
To perform an inhalation, follow the instructions below each time. The Turbuhaler is a multi-dose inhaler for administering the medicine.
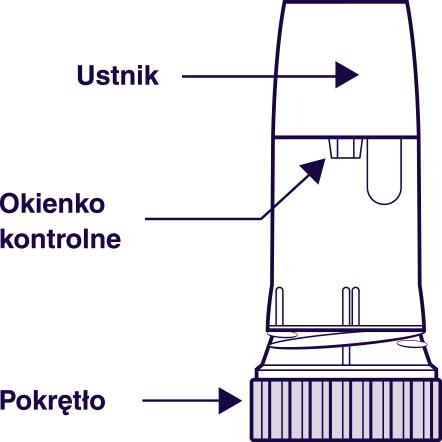
When inhaling through the Turbuhaler, the powder is released into the lungs. Therefore, it is very important to take a full, deep breath through the mouthpiece. The patient should follow the instructions below.
- 1. Remove the cap from the inhaler.
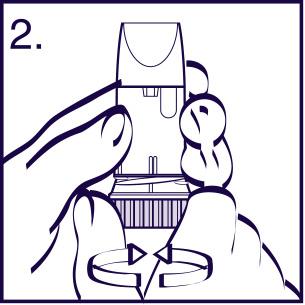
- 2. Hold the inhaler upright, with the base down (Figure 2). When loading the dose, do not hold the inhaler by the mouthpiece. To load the dose, turn the wheel until it clicks in one direction, then turn it until it clicks in the other direction(the direction you start turning the wheel does not matter). A characteristic click sound will be heard. The inhaler is now loaded and ready for use, and the patient should not repeat the above step. To take the dose, the patient should follow the rest of the instructions.
- 3. Exhale. Do notexhale through the inhaler.
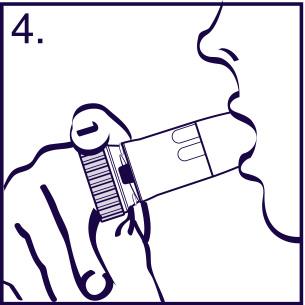
- 4. Place the mouthpiece between the teeth, close the lips, and take a deep and strong breath through the mouth. Do not chew or bite the mouthpiece. Do not use a damaged inhaler or an inhaler without a mouthpiece.
- 5. Before exhaling, remove the inhaler from the mouth. If more than one dose is prescribed, the patient should repeat the steps according to points 2-5.
- 6. Put the cap back on the inhaler and screw it on.
- 7. Rinse the mouth with water after taking the prescribed dose.
Warning!
Never EXHALEthrough the mouthpiece. After taking the medicine, the patient should always screw the cap on tightly. Due to the very small amount of powdered medicine, the patient may not feel the taste of the medicine after inhalation. However, the patient can be sure that the prescribed dose has been taken if they follow the instructions above.
Cleaning the Pulmicort Turbuhaler inhaler
The outer part of the mouthpiece should be cleaned regularly (once a week) with a dry cloth.
Do not use water to clean the mouthpiece.
When to start using a new inhaler
Dose indicator When the red mark first appears in the control window, it means that there are about 20 doses left in the device (Figure 1). When the red stripe reaches the bottom of the control window (Figure 2), it means that the inhaler can no longer be used. The dose of medicine released from the inhaler may then be too small. When shaking the inhaler, a characteristic sound of the desiccant flowing can be heard.
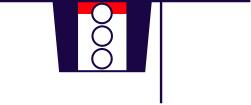
Figure 1 Figure 2 If the patient feels that the effect of Pulmicort Turbuhaler is too strong or too weak, they should consult their doctor.
Using a higher than recommended dose of Pulmicort Turbuhaler
It is important for the patient to use the medicine as directed by the doctor. The patient should not increase or decrease the dose of the medicine without consulting their doctor. If the patient takes more than the recommended dose of the medicine, they should see their doctor immediately.
Missing a dose of Pulmicort Turbuhaler
Pulmicort Turbuhaler in the form of inhalation powder should be taken as directed by the doctor and only the prescribed number of doses should be taken. The patient should not take a double dose to make up for a missed dose. If the patient has any further doubts about using this medicine, they should consult their doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Stop using Pulmicort Turbuhaler and contact your doctor immediately
if the patient experiences any of the following symptoms:severe allergic reactions, e.g., swelling of the face, especially around the mouth (tongue and/or throat) and/or difficulty swallowing or hives occurring at the same time as difficulty breathing (angioedema), bronchospasm, and/or sudden weakness (fainting).
Other side effects
Common side effects (less than 1 in 10 patients)
- fungal infections (candidiasis) of the mouth and throat. The patient should rinse their mouth with water after each dose to reduce the risk of oral candidiasis.
- irritation of the throat, cough, hoarseness,
- loss of voice,
- pneumonia (lung infection) in patients with COPD.
The patient should tell their doctor if they experience any of the following symptoms, which may be signs of a lung infection:
- fever or chills,
- increased production of mucus or change in mucus color,
- worsening cough or increased breathing difficulties.
Uncommon side effects (less than 1 in 100 patients)
- cataract,
- blurred vision,
- muscle cramps,
- muscle tremors,
- depression,
- anxiety.
Rare side effects (less than 1 in 1000 patients)
- immediate and delayed hypersensitivity reactions, including rash, contact dermatitis, urticaria, angioedema (swelling of soft tissues caused by increased vascular permeability: swelling of the eyelids, face, lips, tongue, larynx), severe allergic reactions,
- easy bruising (bruises),
- bronchospasm,
- nervousness, changes in behavior (mainly in children).
- systemic effects of glucocorticosteroids, including adrenal suppression and growth retardation (in children and adolescents),
- loss of voice (in children),
- hoarseness (in children).
Side effects with unknown frequency
- glaucoma
- sleep disturbances,
- anxiety,
- excessive psychomotor activity,
- aggression.
Systemic effects may include Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone density, cataracts, glaucoma, and less frequently, psychiatric or behavioral problems, including psychomotor hyperactivity, sleep disturbances, anxiety, depression, or aggression (especially in children). If the patient experiences any of these side effects, they should contact their doctor or go to the nearest hospital immediately.
Reporting side effects
If the patient experiences any side effects, including any side effects not listed in the leaflet, they should tell their doctor. Side effects can be reported directly to the Department of Drug Safety Monitoring, Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, Tel: +48 22 49 21 301, Fax: +48 22 49 21 309, website: https://smz.ezdrowie.gov.pl. Side effects can also be reported to the marketing authorization holder. By reporting side effects, more information can be collected on the safety of the medicine.
5. How to store Pulmicort Turbuhaler
Store at a temperature not exceeding 30°C. The medicine should be stored out of sight and reach of children. Do not use this medicine after the expiry date stated on the packaging after the "EXP" date. The expiry date refers to the last day of the month stated. Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Package contents and other information
What Pulmicort Turbuhaler contains
The active substance of Pulmicort Turbuhaler is budesonide. One dose contains 100 micrograms (μg) or 200 micrograms (μg) of budesonide.
What Pulmicort Turbuhaler looks like and what the package contains
A dose counter with a mouthpiece and a protective cap in a cardboard box. Pulmicort Turbuhaler 100 μg contains 200 doses. Pulmicort Turbuhaler 200 μg contains 100 doses. Each inhaler is also labeled with: 200 DOSES BUDESONIDE 100 μg/DOSE LOT/CH.-B/LOTE ZM 1234 EXP/VERW.BIS/CAD MM-YYYY or 100 DOSES BUDESONIDE 200 μg/DOSE LOT/CH.-B/LOTE ZM 1234 EXP/VERW.BIS/CAD MM-YYYY
Marketing authorization holder and manufacturer
Marketing authorization holder: AstraZeneca AB S-151 85 Sodertalje Sweden Manufacturer: AstraZeneca AB Forskargatan 18 151 36 Södertälje Sweden For more information, the patient should contact the representative of the marketing authorization holder: AstraZeneca Pharma Poland Sp. z o.o. ul. Postępu 14 02-676 Warsaw tel: +48 22 245 73 00 fax: +48 22 485 30 07 Date of last revision of the leaflet:November 2022
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterAstraZeneca AB
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Pulmicort TurbuhalerDosage form: Suspension, 0.125 mg/mlActive substance: budesonidePrescription requiredDosage form: Suspension, 0.25 mg/mlActive substance: budesonidePrescription requiredDosage form: Suspension, 0.5 mg/mlActive substance: budesonidePrescription required
Alternatives to Pulmicort Turbuhaler in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Pulmicort Turbuhaler in Ukraine
Alternative to Pulmicort Turbuhaler in Spain
Online doctors for Pulmicort Turbuhaler
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Pulmicort Turbuhaler – subject to medical assessment and local rules.















