
How to use Pomalidomide Grindeks
Leaflet attached to the packaging: patient information
Pomalidomide Grindeks, 1 mg, hard capsules
Pomalidomide Grindeks, 2 mg, hard capsules
Pomalidomide Grindeks, 3 mg, hard capsules
Pomalidomide Grindeks, 4 mg, hard capsules
Pomalidomide
It should be expected that Pomalidomide Grindeks will cause severe birth defects and may lead to fetal death.
- The medicine should not be taken if the patient is pregnant or may become pregnant.
- Contraceptive advice presented in this leaflet must be followed.
Read the leaflet carefully before taking the medicine, as it contains important information for the patient.
- The leaflet should be kept in case it needs to be read again.
- In case of any doubts, the doctor or pharmacist should be consulted.
- The medicine has been prescribed to a specific person. It should not be given to others. The medicine may harm another person, even if the symptoms of their disease are the same.
- If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet
- 1. What is Pomalidomide Grindeks and what is it used for
- 2. Important information before taking Pomalidomide Grindeks
- 3. How to take Pomalidomide Grindeks
- 4. Possible side effects
- 5. How to store Pomalidomide Grindeks
- 6. Contents of the packaging and other information
1. What is Pomalidomide Grindeks and what is it used for
Pomalidomide Grindeks contains the active substance "pomalidomide". This medicine is similar to thalidomide and belongs to a group of medicines that affect the immune system (the body's natural defense).
What is Pomalidomide Grindeks used for
Pomalidomide Grindeks is used to treat adults with a type of cancer called "multiple myeloma".
Pomalidomide Grindeks is used in combination with:
- two other medicines, bortezomib (a type of chemotherapy) and dexamethasone (an anti-inflammatory medicine) in patients who have already received at least one other type of treatment containing lenalidomide.
or
- one other medicine, dexamethasone in patients with multiple myeloma that has worsened despite previous treatment with at least two other types of treatment containing lenalidomide and bortezomib.
What is multiple myeloma
Multiple myeloma is a cancer that attacks a type of blood cell (called plasma cells). These cells grow uncontrollably and accumulate in the bone marrow, causing damage to bones and kidneys.
In principle, multiple myeloma is incurable. However, treatment can alleviate the symptoms of the disease or make them disappear for a while - this is called a "response" to treatment.
How does Pomalidomide Grindeks work
Pomalidomide Grindeks works in several ways:
- by inhibiting the growth of myeloma cells,
- by stimulating the immune system to attack cancer cells,
- by inhibiting the formation of blood vessels that feed cancer cells.
Benefits of using Pomalidomide Grindeks with bortezomib and dexamethasone
Pomalidomide Grindeks, when used in combination with bortezomib and dexamethasone in patients who have already received at least one other type of treatment, may inhibit the progression of multiple myeloma.
Pomalidomide Grindeks used with bortezomib and dexamethasone usually delayed the recurrence of multiple myeloma by 11 months - compared to 7 months in patients who received only bortezomib and dexamethasone.
Benefits of using Pomalidomide Grindeks with dexamethasone
Pomalidomide Grindeks, when used in combination with dexamethasone in patients who have already received at least two other types of treatment, may inhibit the progression of multiple myeloma.
Pomalidomide Grindeks used with dexamethasone usually delayed the recurrence of multiple myeloma by 4 months - compared to 2 months in patients who received only dexamethasone.
2. Important information before taking Pomalidomide Grindeks
When not to take Pomalidomide Grindeks
- if the patient is pregnant, suspects she is pregnant, or plans to become pregnant, as it should be expected that Pomalidomide Grindeks will harm the fetus.
- if the patient may become pregnant, unless all necessary contraceptive methods are used (see "Pregnancy, contraception, and breastfeeding - information for women and men" below).
- if the patient is allergic to pomalidomide or any of the other ingredients of this medicine listed in section 6.
If the patient is unsure whether any of the above situations apply to them, they should consult their doctor, pharmacist, or nurse before starting treatment with Pomalidomide Grindeks.
Warnings and precautions
Before starting treatment with Pomalidomide Grindeks, the patient should discuss the following with their doctor, pharmacist, or nurse:
- if the patient has ever had blood clots in the past. During treatment with Pomalidomide Grindeks, there is an increased risk of blood clots in veins and arteries. The doctor may recommend additional treatment (e.g., warfarin) or reduce the dose of Pomalidomide Grindeks to reduce the risk of blood clots.
- if the patient has ever had an allergic reaction, such as a rash, itching, swelling, dizziness, or breathing problems, while taking similar medicines called "thalidomide" and "lenalidomide".
- if the patient has had a heart attack, has heart failure, has breathing difficulties, or smokes, has high blood pressure, or high cholesterol levels.
- if the patient has extensive cancerous changes in the body, including in the bone marrow. These changes may lead to a condition in which tumors break down, releasing abnormal levels of chemical substances, which can lead to kidney failure. The patient may also experience heart rhythm disturbances. This condition is called tumor lysis syndrome.
- if the patient has or has had nerve damage (causing numbness or pain in the hands or feet).
- if the patient has or has had a hepatitis B virus infection. Taking Pomalidomide Grindeks may cause the virus to reactivate in previously infected patients, leading to a recurrence of the infection. The doctor should check if the patient has been infected with the hepatitis B virus in the past.
- if the patient has or has had a combination of any of the following symptoms: rash on the face or widespread rash, redness of the skin, high fever, flu-like symptoms, swollen lymph nodes (observed by the patient as symptoms of a severe skin reaction called "drug reaction with eosinophilia and systemic symptoms" (DRESS) or "drug hypersensitivity syndrome", toxic epidermal necrolysis (TEN), or Stevens-Johnson syndrome (SJS), see also section 4 "Possible side effects").
It should be emphasized that in patients with multiple myeloma treated with pomalidomide, additional types of cancer may develop. Therefore, the treating doctor should carefully assess the benefits and risks associated with prescribing this medicine to the patient.
At any time during treatment or after its completion, the doctor or nurse should be informed immediately if the patient experiences: vision disturbances, loss of vision, or double vision, speech difficulties, weakness in the arms or legs, changes in gait, or balance problems, persistent numbness, decreased sensation, or loss of sensation, memory loss, or disorientation.
All of the above symptoms may indicate a severe and potentially life-threatening brain disease called progressive multifocal leukoencephalopathy. If these symptoms occurred before taking Pomalidomide Grindeks, the patient should inform their doctor about any changes in these symptoms.
After completing treatment, the patient should return any unused capsules to the pharmacy.
Pregnancy, contraception, and breastfeeding - information for women and men
As indicated below, during treatment with Pomalidomide Grindeks, pregnancy prevention program requirements must be followed. Women taking Pomalidomide Grindeks must not become pregnant, and the partner of a man being treated with pomalidomide must not become pregnant, as it should be expected that this medicine will harm the fetus. The patient and their partner should use effective contraceptive methods during treatment with this medicine.
Women
Pomalidomide Grindeks should not be taken if the patient is pregnant, suspects she is pregnant, or plans to become pregnant, as it should be expected that this medicine will harm the fetus. Before starting treatment, the patient should inform her doctor that she may become pregnant, even if she thinks it is unlikely.
If the patient may become pregnant:
- she must use effective contraceptive methods for at least 4 weeks before starting treatment, during treatment, and for at least 4 weeks after completing treatment. The patient should discuss with her doctor which contraceptive method is best for her.
If the patient becomes pregnant despite using contraceptive methods:
- she must stop treatment immediately and inform her doctor immediately.
Breastfeeding
It is not known whether Pomalidomide Grindeks passes into human milk. If the patient is breastfeeding or plans to breastfeed, she should tell her doctor. The doctor will advise whether to stop or continue breastfeeding.
Men
Pomalidomide Grindeks is present in human semen.
- If the partner is pregnant or may become pregnant, the man should use condoms during the entire treatment period and for 7 days after completing treatment.
- If the partner of a man being treated with Pomalidomide Grindeks becomes pregnant, the partner should inform the doctor immediately. The partner should see a doctor immediately.
Blood donation and blood tests
During treatment and for 7 days after completing treatment, the patient should not donate blood.
Before and during treatment with Pomalidomide Grindeks, the patient will have regular blood tests. This is because the medicine can cause a decrease in the number of blood cells (white blood cells) that help fight infections and a decrease in the number of cells (platelets) that help stop bleeding.
The doctor will schedule blood tests:
- before treatment,
- every week during the first 8 weeks of treatment,
- then at least once a month for as long as the patient takes Pomalidomide Grindeks.
The doctor may change the dose of Pomalidomide Grindeks or stop treatment based on the patient's blood test results. The doctor may also change the dose or stop treatment due to the patient's overall health.
Children and adolescents
Pomalidomide Grindeks is not recommended for use in children and adolescents under 18 years of age.
Pomalidomide Grindeks and other medicines
The patient should tell their doctor or pharmacist about all medicines they are taking or have recently taken, as well as any medicines they plan to take, as Pomalidomide Grindeks may affect the action of other medicines. Other medicines may also affect the action of Pomalidomide Grindeks.
Before taking Pomalidomide Grindeks, the patient should inform their doctor, pharmacist, or nurse, in particular, if they are taking any of the following medicines:
- certain antifungal medicines, such as ketoconazole
- certain antibiotics (e.g., ciprofloxacin, enoxacin)
- certain antidepressants, such as fluvoxamine
Driving and using machines
While taking Pomalidomide Grindeks, some people may feel tired, dizzy, faint, disoriented, or have decreased alertness. If these symptoms occur, the patient should not drive, use tools, or operate machinery.
Pomalidomide Grindeks
The medicine contains less than 1 mmol (23 mg) of sodium per capsule, which means that the medicine is considered "sodium-free".
Pomalidomide Grindeks contains azo dyes
The capsules contain azo dyes: brilliant black PN (all strengths), azorubine (all strengths), and orange yellow FCF (only 2 mg capsules). These dyes may cause allergic reactions.
3. How to take Pomalidomide Grindeks
Pomalidomide Grindeks must be administered by a doctor with experience in treating multiple myeloma.
This medicine should always be taken as directed by the doctor. If the patient has any doubts, they should consult their doctor, pharmacist, or nurse.
When to take Pomalidomide Grindeks with other medicines
Pomalidomide Grindeks with bortezomib and dexamethasone
- The patient should read the leaflets for bortezomib and dexamethasone to obtain further information on their use and action.
- Pomalidomide Grindeks, bortezomib, and dexamethasone are taken in treatment cycles. Each cycle lasts 21 days (3 weeks).
- The following table shows which medicines to take on which days of the 3-week cycle:
PMD:Pomalidomide Grindeks; BOR: bortezomib; DEX: dexamethasone
Cycles 1 to 8 Cycle 9 and subsequent
Medicine name
Day PMD BOR DEX
1
√
√
√
2
√
√
3
√
4
√
√
√
5
√
√
6
√
7
√
8
√
√
√
9
√
√
10
√
11
√
√
√
12
√
√
13
√
14
√
15
16
17
18
19
20
21
Medicine name
Day PMD BOR DEX
1
√
√
√
2
√
√
3
√
4
√
5
√
6
√
7
√
8
√
√
√
9
√
√
10
√
11
√
12
√
13
√
14
√
15
16
17
18
19
20
21
After completing each 3-week cycle, a new cycle should be started.
Pomalidomide Grindeks only with dexamethasone
- The patient should read the leaflet for dexamethasone to obtain further information on its use and action.
- Pomalidomide Grindeks and dexamethasone are taken in treatment cycles. Each cycle lasts 28 days (4 weeks).
- The following table shows which medicines to take on which days of the 4-week cycle:
PMD:Pomalidomide Grindeks; DEX: dexamethasone
Medicine name
Day PMD DEX
1
√
√
2
√
3
√
4
√
5
√
6
√
7
√
8
√
√
9
√
10
√
11
√
12
√
13
√
14
√
15
√
√
16
√
17
√
18
√
19
√
20
√
21
√
22
√
23
24
√
25
26
27
28
After completing each 4-week cycle, a new cycle should be started.
What dose of Pomalidomide Grindeks to take with other medicines
Pomalidomide Grindeks with bortezomib and dexamethasone
- The recommended starting dose of Pomalidomide Grindeks is 4 mg per day.
- The recommended starting dose of bortezomib will be determined by the doctor based on the patient's weight and body surface area (1.3 mg/m2).
- The recommended starting dose of dexamethasone is 20 mg per day. However, if the patient is over 75 years old, the recommended starting dose is 10 mg per day.
Pomalidomide Grindeks only with dexamethasone
- The recommended dose of Pomalidomide Grindeks is 4 mg per day.
- The recommended starting dose of dexamethasone is 40 mg per day. However, if the patient is over 75 years old, the recommended starting dose is 20 mg per day.
The doctor may reduce the dose of Pomalidomide Grindeks, bortezomib, or dexamethasone, or stop treatment with one or more of these medicines, depending on the patient's blood test results, overall health, use of other medicines (e.g., ciprofloxacin, enoxacin, and fluvoxamine), and if the patient experiences side effects resulting from treatment (especially rash and swelling).
If the patient has kidney problems and is on dialysis, the doctor will advise on how and when to take Pomalidomide Grindeks.
How to take Pomalidomide Grindeks
- Do not break, open, or chew the capsules. If the powder from a damaged capsule comes into contact with the skin, the skin should be washed immediately with soap and water.
- Healthcare professionals, caregivers, and family members should wear disposable gloves when handling the blister or capsule. The gloves should then be carefully removed to avoid skin exposure, placed in a sealed plastic bag, and disposed of according to local regulations. Then, the hands should be washed thoroughly with soap and water. Pregnant women or those who suspect they may be pregnant should not touch the blister or capsule.
- The capsules should be swallowed whole, preferably with water.
- The capsules can be taken with or without food.
- Pomalidomide Grindeks should be taken at approximately the same time every day.
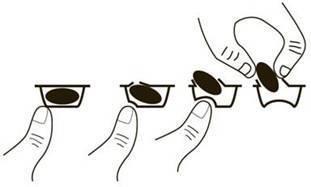
To remove a capsule from the blister, press the capsule only from one end and push it through the foil. Do not press the middle of the capsule, as this may damage it.
If the patient has kidney problems and is on dialysis, the doctor will advise on how and when to take Pomalidomide Grindeks.
Duration of treatment with Pomalidomide Grindeks
Treatment cycles should be continued until the doctor decides to stop treatment.
Taking a higher dose of Pomalidomide Grindeks than recommended
If the patient takes a higher dose of the medicine than recommended, they should immediately inform their doctor or go to the hospital. The patient should take the medicine packaging with them.
Missing a dose of Pomalidomide Grindeks
If the patient misses a dose of Pomalidomide Grindeks on the day it is due to be taken, they should take the next capsule at the scheduled time the next day. The patient should not take a double dose to make up for the missed capsule.
If the patient has any further doubts about taking this medicine, they should consult their doctor or pharmacist.
4. Possible side effects
Like all medicines, Pomalidomide Grindeks can cause side effects, although not everybody gets them.
Severe side effects
If any of the following severe side effects occur, the patient should stop taking Pomalidomide Grindeks and consult their doctor immediately - immediate treatment may be necessary.
- fever, chills, sore throat, cough, mouth ulcers, or any other signs of infection (due to a low number of white blood cells that help fight infections).
- bleeding or bruising without cause, including nosebleeds, gastrointestinal bleeding, or stomach bleeding (due to the effect of the medicine on blood cells called platelets).
- rapid breathing, rapid heartbeat, fever, and chills, passing very little or no urine, nausea, and vomiting, disorientation, loss of consciousness (due to a blood infection called sepsis or septic shock).
- severe, persistent, or bloody diarrhea (also with abdominal pain or fever) caused by bacteria called Clostridium difficile.
- chest pain or leg pain and swelling, especially in the legs and ankles (caused by blood clots).
- shortness of breath (due to severe chest infections, pneumonia, heart failure, or blood clots).
- swelling of the face, lips, tongue, and throat, which can cause breathing difficulties (due to severe allergic reactions called angioedema and anaphylaxis).
- certain types of skin cancer (squamous cell carcinoma and basal cell carcinoma) that can cause changes in the appearance of the skin or the formation of growths on the skin. If the patient notices any changes in their skin while taking Pomalidomide Grindeks, they should inform their doctor as soon as possible.
- recurrence of hepatitis B virus infection, which can cause yellowing of the skin and whites of the eyes (jaundice), dark urine, abdominal pain on the right side, fever, nausea, and vomiting. The patient should inform their doctor immediately if they notice these symptoms.
- widespread rash, high body temperature, swollen lymph nodes, and involvement of other organs (drug reaction with eosinophilia and systemic symptoms, also known as DRESS or drug hypersensitivity syndrome, toxic epidermal necrolysis, or Stevens-Johnson syndrome). If these symptoms occur, the patient should stop taking pomalidomide and consult their doctor or seek immediate medical attention.
If any of the above severe side effects occur, the patient should stop taking Pomalidomide Grindeks and consult their doctor immediately- immediate treatment may be necessary.
Other side effects
Very common(may affect more than 1 in 10 people):
- shortness of breath (dyspnea).
- lung infections (pneumonia and bronchitis).
- nose, sinus, and throat infections caused by bacteria or viruses.
- flu-like symptoms (influenza).
- decrease in red blood cell count, which can cause fatigue and weakness.
- low potassium levels in the blood (hypokalemia), which can cause weakness, muscle cramps, muscle pain, irregular heartbeat, tingling, or numbness.
- high blood sugar levels.
- rapid and irregular heartbeat (atrial fibrillation).
- loss of appetite.
- constipation, diarrhea, or nausea.
- vomiting.
- abdominal pain.
- fatigue.
- difficulty sleeping or maintaining sleep continuity.
- dizziness, tremors.
- muscle cramps, muscle weakness.
- bone pain, back pain.
- numbness, tingling, or burning sensation in the skin (peripheral sensory neuropathy).
- swelling of the body, including hands and feet.
- rash.
- urinary tract infection, which can cause burning during urination or frequent urination.
Common(may affect up to 1 in 10 people):
- dizziness.
- bleeding in the brain.
- decreased ability to move or feel in the arms, legs, hands, and feet due to nerve damage (peripheral sensory-motor neuropathy).
- tingling, itching, or burning sensation in the skin (paresthesia).
- feeling of spinning or loss of balance.
- swelling caused by fluid accumulation.
- hives.
- rash.
- itching.
- shingles.
- heart attack (chest pain radiating to the arms, neck, jaw, sweating, or shortness of breath, nausea, or vomiting).
- chest pain or lung infection.
- high blood pressure.
- decrease in the number of blood cells (pancytopenia), which can cause fatigue, weakness, and increased risk of bleeding and bruising.
- decrease in lymphocyte count (a type of white blood cell), often caused by infection (lymphopenia).
- low magnesium levels in the blood (hypomagnesemia), which can cause fatigue, general weakness, muscle cramps, irritability, and low calcium levels in the blood (hypocalcemia), which can cause numbness or tingling in the hands, feet, or lips, muscle cramps, muscle weakness, tetany, disorientation, or seizures.
- low phosphate levels in the blood (hypophosphatemia), which can cause muscle weakness and irritability or disorientation.
- high calcium levels in the blood (hypercalcemia), which can cause slowed reflexes and muscle weakness.
- high potassium levels in the blood, which can cause abnormal heart rhythm.
- low sodium levels in the blood, which can cause fatigue, disorientation, muscle tremors, seizures (convulsions), or coma.
- high uric acid levels in the blood, which can lead to gout.
- low blood pressure, which can cause dizziness or fainting.
- mouth pain or dryness.
- changes in taste.
- abdominal swelling.
- disorientation.
- depression.
- loss of consciousness, fainting.
- cataract (clouding of the eye lens).
- kidney damage.
- inability to urinate.
- abnormal liver test results.
- pelvic pain.
- weight loss.
Uncommon(may affect up to 1 in 100 people):
- stroke.
- liver inflammation, which can cause itching, yellowing of the skin and whites of the eyes (jaundice), light-colored stools, dark urine, abdominal pain, and fever.
- tumor lysis syndrome, which can lead to kidney problems.
- underactive thyroid gland, which can cause fatigue, lethargy, muscle weakness, slow heart rate, weight gain.
Frequency not known(frequency cannot be estimated from the available data):
- rejection of a transplanted organ (such as a heart or liver).
Reporting side effects
If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor, pharmacist, or nurse. Side effects can be reported directly to the Department of Drug Safety, Urząd Rejestracji Produktów Leczniczych, Wyrobów Medycznych i Produktów Biobójczych: Al. Jerozolimskie 181C, 02-222 Warszawa, tel.: + 48 22 49 21 301, fax: + 48 22 49 21 309, website: https://smz.ezdrowie.gov.pl.
Side effects can also be reported to the marketing authorization holder.
By reporting side effects, more information can be collected on the safety of this medicine.
5. How to store Pomalidomide Grindeks
The medicine should be stored out of sight and reach of children.
Do not use this medicine after the expiry date stated on the blister and carton, respectively, after: EXP or Expiry date (EXP). The expiry date refers to the last day of the month stated.
There are no special storage instructions for this medicine.
Pomalidomide Grindeks should not be used if the patient notices any damage or signs of opening.
Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Contents of the packaging and other information
What Pomalidomide Grindeks contains
Pomalidomide Grindeks, 1 mg, hard capsules
- The active substance is pomalidomide. Each capsule contains 1 mg of pomalidomide.
- The other ingredients are: maize starch, maltodextrin, crospovidone, colloidal anhydrous silica, sodium stearyl fumarate.
- The capsule shell contains: gelatin, titanium dioxide (E171), colorants (iron oxide yellow (E172), iron oxide black (E172), brilliant black PN (E151), patent blue V (E131), azorubine (E122), brilliant blue FCF (E133)), and white printing ink (shellac, titanium dioxide (E171), sodium hydroxide, propylene glycol, and povidone).
Pomalidomide Grindeks, 2 mg, hard capsules
- The active substance is pomalidomide. Each capsule contains 2 mg of pomalidomide.
- The other ingredients are: maize starch, maltodextrin, crospovidone, colloidal anhydrous silica, sodium stearyl fumarate.
- The capsule shell contains: gelatin, titanium dioxide (E171), colorants (orange yellow FCF (E110), brilliant black PN (E151), patent blue V (E131), azorubine (E122)), and white printing ink (shellac, titanium dioxide (E171), sodium hydroxide, propylene glycol, and povidone).
Pomalidomide Grindeks, 3 mg, hard capsules
- The active substance is pomalidomide. Each capsule contains 3 mg of pomalidomide.
- The other ingredients are: maize starch, maltodextrin, crospovidone, colloidal anhydrous silica, sodium stearyl fumarate.
- The capsule shell contains: gelatin, titanium dioxide (E171), colorants (brilliant black PN (E151), patent blue V (E131), azorubine (E122), brilliant blue FCF (E133), erythrosine (E127)), and white printing ink (shellac, titanium dioxide (E171), sodium hydroxide, propylene glycol, and povidone).
Pomalidomide Grindeks, 4 mg, hard capsules
- The active substance is pomalidomide. Each capsule contains 4 mg of pomalidomide.
- The other ingredients are: maize starch, maltodextrin, crospovidone, colloidal anhydrous silica, sodium stearyl fumarate.
- The capsule shell contains: gelatin, titanium dioxide (E171), colorants (brilliant blue FCF (E133), brilliant black PN (E151), patent blue V (E131), azorubine (E122), erythrosine (E127)), and white printing ink (shellac, titanium dioxide (E171), sodium hydroxide, propylene glycol, and povidone).
What Pomalidomide Grindeks looks like and contents of the pack
Pomalidomide Grindeks, 1 mg, are hard gelatin capsules, size 4 (approximately 14 mm × 5 mm), with a light gray body and a dark blue, opaque cap, with "P1" printed in white ink.
Pomalidomide Grindeks, 2 mg, are hard gelatin capsules, size 3 (approximately 16 mm × 6 mm), with an orange, opaque body and a dark blue, opaque cap, with "P2" printed in white ink.
Pomalidomide Grindeks, 3 mg, are hard gelatin capsules, size 2 (approximately 18 mm × 6 mm), with a light blue body and a dark blue, opaque cap, with "P3" printed in white ink.
Pomalidomide Grindeks, 4 mg, are hard gelatin capsules, size 1 (approximately 19 mm × 7 mm), with a blue, opaque body and a dark blue, opaque cap, with "P4" printed in white ink.
The capsules are available in packs of 14 or 21 capsules (2 or 3 blisters in a pack, with 7 capsules in each blister), in a cardboard box.
Not all pack sizes may be marketed.
Marketing authorization holder and manufacturer
AS GRINDEKS
Krustpils iela 53,
Rīga, LV-1057,
Latvia
tel.: + 371 67083205
e-mail: [email protected]
This medicine is authorized in the Member States of the European Economic Area under the following names:
Austria
Pomalidomid Grindeks 1 mg, 2 mg, 3 mg, 4 mg Hartkapseln
Belgium
Pomalidomide Grindeks 1 mg, 2 mg, 3 mg, 4 mg gélules
Bulgaria
Помалидомид Гриндекс 1 mg, 2 mg, 3 mg, 4 mg твърди капсули
Pomalidomide Grindeks 1 mg, 2 mg, 3 mg, 4 mg hard capsules
Denmark
Pomalidomid Grindeks
Estonia
Pomalidomide Grindeks
Finland
Pomalidomide Grindeks 1 mg, 2 mg, 3 mg, 4 mg kovat kapselit
France
POMALIDOMIDE GRINDEKS 1 mg, gélule POMALIDOMIDE GRINDEKS 2 mg, gélule POMALIDOMIDE GRINDEKS 3 mg, gélule POMALIDOMIDE GRINDEKS 4 mg, gélule
Greece
Pomalidomide/Grindeks
Spain
Pomalidomida Grindeks 1 mg, 2 mg, 3 mg, 4 mg cápsula dura
Netherlands
Pomalidomide Grindeks 1 mg harde capsules Pomalidomide Grindeks 2 mg harde capsules Pomalidomide Grindeks 3 mg harde capsules Pomalidomide Grindeks 4 mg harde capsules
Ireland
Pomalidomide Grindeks 1 mg, 2 mg, 3 mg, 4 mg hard capsule
Lithuania
Pomalidomide Grindeks 1 mg, 2 mg, 3 mg, 4 mg kietosios kapsulės
Latvia
Pomalidomide Grindeks 1 mg, 2 mg, 3 mg, 4 mg cietās kapsulas
Germany
Pomalidomid Grindeks 1 mg, 2 mg, 3 mg, 4 mg Hartkapseln
Norway
Pomalidomide Grindeks
Poland
Pomalidomide Grindeks
Portugal
Pomalidomida Grindeks 1 mg, 2 mg, 3 mg, 4 mg cápsula
Czech Republic
Pomalidomide Grindeks
Romania
Pomalidomidă Grindeks 1 mg capsule Pomalidomidă Grindeks 2 mg capsule Pomalidomidă Grindeks 3 mg capsule Pomalidomidă Grindeks 4 mg capsule
Slovakia
Pomalidomid Grindeks 1 mg tvrdé kapsuly Pomalidomid Grindeks 2 mg tvrdé kapsuly Pomalidomid Grindeks 3 mg tvrdé kapsuly Pomalidomid Grindeks 4 mg tvrdé kapsuly
Slovenia
Pomalidomid Grindeks 1 mg, 2 mg, 3 mg, 4 mg trde kapsule
Sweden
Pomalidomide Grindeks 1 mg, 2 mg, 3 mg, 4 mg hårda kapslar
Hungary
Pomalidomide Grindeks 1 mg, 2 mg, 3 mg, 4 mg kemény kapszula
Italy
Pomalidomide Grindeks
Date of last revision of the leaflet:04/2025
- Country of registration
- Active substance
- Prescription requiredYes
- ImporterAS Grindeks
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Pomalidomide GrindeksDosage form: Capsules, 3 mgActive substance: pomalidomidePrescription requiredDosage form: Capsules, 4 mgActive substance: pomalidomidePrescription requiredDosage form: Capsules, 1 mgActive substance: pomalidomidePrescription required
Alternatives to Pomalidomide Grindeks in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Pomalidomide Grindeks in Spain
Alternative to Pomalidomide Grindeks in Ukraine
Online doctors for Pomalidomide Grindeks
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Pomalidomide Grindeks – subject to medical assessment and local rules.






