

Oekolp

Ask a doctor about a prescription for Oekolp

How to use Oekolp
Package Leaflet: Information for the Patient
OEKOLP, 1 mg/g, vaginal cream
Estriol
Read the package leaflet carefully before using the medicine, as it contains important information for the patient.
- Keep this leaflet, you may need to read it again.
- In case of any doubts, consult a doctor or pharmacist.
- This medicine has been prescribed specifically for you. Do not pass it on to others. The medicine may harm them, even if their symptoms are the same as yours.
- If the patient experiences any side effects, including those not listed in this leaflet, they should inform their doctor or pharmacist. See section 4.
Table of Contents of the Leaflet
- 1. What is Oekolp and what is it used for
- 2. Important information before using Oekolp
- 3. How to use Oekolp
- 4. Possible side effects
- 5. How to store Oekolp
- 6. Contents of the pack and other information
1. What is Oekolp and what is it used for
Oekolp belongs to a group of medicines called hormone replacement therapy (HRT) for vaginal use. The medicine contains the female sex hormone estriol (estrogen). Oekolp is used in postmenopausal women, at least 12 months after the last natural menstrual period.
Oekolp is used to alleviate menopausal symptoms in the vagina, such as dryness or irritation. In medical terminology, this phenomenon is referred to as "atrophic vaginitis". It is caused by a decrease in estrogen levels in the body and occurs naturally after menopause.
If the ovaries are surgically removed before menopause (a procedure called oophorectomy), estrogen production decreases very quickly.
Estrogen deficiency can cause dryness and increased sensitivity of the vaginal walls, which is the cause of painful intercourse and the occurrence of inflammatory conditions and severe itching of the vagina. Estrogen deficiency can also cause symptoms of urinary incontinence and recurrent urinary tract infections. These symptoms often disappear after the use of estrogen-containing medications. Noticeable improvement usually occurs within a few days or weeks after starting treatment.
Oekolp works by replacing estrogen, which is normally produced by the woman's ovaries.
The medicine is administered vaginally, and the hormone is released where it is needed. This can alleviate discomfort in the vagina.
Improvement may only be noticeable after a few days or even weeks.
In addition to the above indications, Oekolp cream may also be used to:
- accelerate the healing of postoperative wounds in women who have undergone vaginal surgery,
- facilitate the accurate assessment of cervical smears in postmenopausal women.
2. Important information before using Oekolp
Medical history and regular check-ups
The use of HRT is associated with a risk that should be considered when deciding to start or continue therapy.
Experience with the treatment of women who have premature menopause (due to ovarian failure or after surgery) is limited. In women with premature menopause, the risk associated with HRT may be varied. Always consult a doctor.
Before starting (or resuming) HRT, the doctor will take a medical history and may decide to perform a physical examination, including a breast examination and/or gynecological examination through the vagina, if necessary.
After starting Oekolp, regular check-ups with the doctor should be scheduled (at least once a year). During the check-up, the benefits and risks associated with continuing Oekolp therapy should be discussed with the doctor.
Regular breast examinations should be performed as recommended by the doctor.
When not to use Oekolp
Oekolp should not be used if any of the following conditions apply to the patient. In case of uncertainty, consult a doctor before using Oekolp.
Do not use Oekolp:
- If the patient is allergic to estriol or any of the other ingredients of this medicine (listed in section 6).
- If breast cancer is present or has been diagnosed in the past, or if there is a suspicion of breast cancer.
- If an estrogen-dependent tumor is present, such as endometrial cancer (cancer of the lining of the uterus), or if there is a suspicion of such a tumor.
- If there is vaginal bleeding of unknown cause.
- If there is untreated excessive thickening of the lining of the uterus (endometrial hyperplasia).
- If blood clots in blood vessels (venous thrombosis) have occurred currently or in the past, such as deep vein thrombosis or pulmonary embolism.
- If there are blood clotting disorders (such as protein C or protein S deficiency, or antithrombin deficiency).
- If there are currently or recently occurred diseases caused by blood clots in arteries, such as heart attack, stroke, or angina pectoris.
- If there is currently or has been a liver disease, and liver function tests have not returned to normal.
- If there is a rare blood disease called porphyria, which is inherited by family members.
If any of the above health conditions occur for the first time while using Oekolp, treatment should be stopped immediately and a doctor consulted.
Warnings and precautions
Before starting treatment, the doctor should be informed if any of the following conditions are currently present or have occurred in the past, as they may recur or worsen during Oekolp treatment. If this happens, more frequent check-ups with the doctor should be scheduled:
- uterine fibroids (leiomyoma)
- endometriosis (growth of endometrial tissue outside the uterus) or a history of excessive endometrial growth (endometrial hyperplasia)
- increased risk of blood clots (see "Blood clots in veins (venous thrombosis)")
- increased risk of estrogen-dependent tumors (e.g., breast cancer in the mother, sister, or grandmother)
- high blood pressure
- liver disorders, such as liver tumors
- diabetes with or without vascular complications
- gallstones
- migraine or severe headache
- systemic immune system disease affecting multiple internal organs (systemic lupus erythematosus; chronic connective tissue disease with skin changes throughout the body)
- epilepsy
- asthma
- disease affecting the eardrum and causing hearing impairment (otosclerosis)
- fluid retention in the body due to heart or kidney disease
- hereditary and acquired angioedema.
The doctor should be informed if the patient has hepatitis C and is being treated with medications such as ombitasvir/paritaprevir/ritonavir and dasabuvir with or without ribavirin, glecaprevir/pibrentasvir, or sofosbuvir/velpatasvir/voxilaprevir. More information can be found in the "Oekolp and other medicines" section.
The doctor should be informed if any changes are observed during Oekolp treatment.
Stop using Oekolp and consult a doctor immediately,
if any of the following conditions occur while using HRT:
- any of the conditions listed in the "Do not use Oekolp" section
- yellowing of the skin and whites of the eyes (jaundice), which may be a sign of liver disease
- swelling of the face, tongue, and/or throat, and/or difficulty swallowing or hives, with difficulty breathing, suggesting angioedema
- significant increase in blood pressure (which may manifest as headache, fatigue, dizziness)
- migraine-like headaches occurring for the first time
- pregnancy
- symptoms suggesting the formation of blood clots, such as:
- painful swelling and redness of the legs
- sudden chest pain
- breathing difficulties. More information can be found in the "Blood clots in veins (venous thrombosis)" section.
Note: Oekolp is not a contraceptive. If it has been less than 12 months since the last menstrual period or the woman is under 50 years old, contraception should be used to avoid pregnancy. Consult a doctor.
If latex condoms are used during Oekolp treatment, their strength and effectiveness may be reduced.
HRT and tumors
Excessive thickening of the lining of the uterus (endometrial hyperplasia) and cancer of the lining of the uterus (endometrial cancer)
Long-term use of estrogen-only HRT in tablet form may increase the risk of developing endometrial cancer.
It is not certain whether a similar risk exists with repeated or long-term (longer than one year) use of Oekolp. However, it has been shown that Oekolp is absorbed into the bloodstream to a very small extent, and therefore, the addition of a progestogen is not necessary.
Bleeding or spotting should not usually be a cause for concern, but a doctor should be consulted. This may be a sign of endometrial thickening.
To prevent endometrial stimulation, the maximum dose should not be exceeded, and it should not be taken for longer than a few weeks (maximum 4 weeks).
The risks described below are associated with HRT medications that circulate in the blood. Oekolp, on the other hand, is intended for local use in the vagina and is absorbed into the bloodstream to a very small extent. Worsening or recurrence of the following disorders during Oekolp treatment is less likely, but if any concerns arise, a doctor should be consulted.
Breast cancer
Data indicate that Oekolp does not increase the risk of breast cancer in women who have never had breast cancer before. It is not known whether Oekolp can be safely used in women who have had breast cancer.
Regular breast examinations should be performed and a doctor consulted if any changes are noticed, such as:
- indentation or tightening of the skin
- changes in the nipples
- any visible or palpable thickening and/or lumps.
In addition, mammography screening is recommended as advised by the doctor.
Ovarian cancer
Ovarian cancer is rare – much rarer than breast cancer. The use of estrogen-only HRT is associated with a slightly increased risk of ovarian cancer.
The risk of ovarian cancer depends on age. For example, in women aged 50-54 who do not use HRT, ovarian cancer will be diagnosed in about 2 out of 2000 women over a 5-year period. In women who use HRT for 5 years, ovarian cancer will be diagnosed in about 3 out of 2000 women (i.e., about 1 additional case).
Effect of HRT on the heart or circulatory system
Blood clots in veins (venous thrombosis)
The risk of developing blood clots in veins is about 1.3 to 3 times higher in women using HRT than in those not using HRT, especially in the first year of treatment.
Venous thrombosis can have a severe course. If a clot enters the lungs, it can cause chest pain, shortness of breath, fainting, or even death.
The likelihood of developing blood clots in veins increases with age and in the following situations. If any of the following situations apply to the patient, the doctor should be informed:
- prolonged immobilization due to major surgery, injury, or illness (see also section 3 "Need for surgery")
- significant obesity (body mass index over 30 kg/m²)
- blood clotting disorders requiring long-term use of anticoagulant medications
- venous thrombosis in the legs or lungs, or other organs in a close relative
- systemic lupus erythematosus
- cancer.
Symptoms of venous thrombosis are listed in the "Stop using Oekolp and consult a doctor immediately" section.
Comparison
In the population of women over 50 years old who do not use HRT, venous thrombosis is expected to occur in about 4 to 7 out of 1000 women over a 5-year period.
In the group of women over 50 years old who used estrogen-only HRT for more than 5 years, the number of cases will be 5 to 8 out of 1000 women (i.e., 1 additional case).
Heart disease (heart attack)
In women using estrogen-only HRT, the risk of developing heart disease is not increased.
Stroke
The risk of stroke is about 1.5 times higher in women using HRT than in those not using HRT. The number of additional stroke cases associated with HRT increases with age.
Comparison
It is estimated that in women over 50 years old who do not use HRT, stroke will occur in about 8 out of 1000 women over a 5-year period, while in women of the same age using HRT, the rate will be 11 cases per 1000 women over a 5-year period (i.e., 3 additional cases).
Other disorders
HRT does not prevent memory loss. Some evidence suggests a higher risk of memory loss in women who start HRT at an age over 65. Consult a doctor.
Oekolp and other medicines
The doctor or pharmacist should be informed about all medicines currently or recently used by the patient, as well as any medicines planned to be taken, including those available without a prescription, herbal medicines, or other natural products. Other healthcare professionals who prescribe or dispense medicines should also be informed about Oekolp use.
Some medicines may affect the efficacy of Oekolp, and Oekolp may interfere with the action of other medicines, which can lead to irregular bleeding. This applies to the following medicines:
- antiepileptic drugs(such as phenobarbital, phenytoin, and carbamazepine)
- medicines used to treat tuberculosis(such as rifampicin, rifabutin)
- medicines used in HIV infection(such as nevirapine, efavirenz, ritonavir, and nelfinavir)
- herbal products containing St. John's Wort(Hypericum perforatum)
HRT may affect the action of other medicines:
- medicines for viral hepatitis C (such as combination therapy with ombitasvir/paritaprevir/ritonavir and dasabuvir with or without ribavirin; glecaprevir/pibrentasvir or sofosbuvir/velpatasvir/voxilaprevir) may cause increased liver function test results in women using combined hormonal contraceptives containing ethinyl estradiol. Oekolp contains estriol instead of ethinyl estradiol. It is not known whether increased liver function test results may occur during Oekolp treatment with such combination therapy.
Lab tests
If lab tests are required, the doctor or lab staff should be informed about Oekolp use, as it may affect the results of some tests.
Oekolp with food and drink
Food and drink do not affect the efficacy of Oekolp treatment.
Pregnancy and breastfeeding
Oekolp is intended for use in postmenopausal women only.
Pregnancy
If pregnancy occurs, Oekolp treatment should be stopped and a doctor consulted.
Breastfeeding
Women who are breastfeeding should consult a doctor before using Oekolp.
Driving and using machines
Oekolp treatment is unlikely to affect the ability to drive or use machines. However, individual reactions to the medicine may vary.
Oekolp contains propylene glycol
The medicine may cause skin irritation.
3. How to use Oekolp
This medicine should always be used as directed by the doctor or pharmacist. In case of doubts, consult a doctor or pharmacist.
For atrophic changes in the lower urinary and genital tract, 0.5 g of cream (1/2 of the applicator's volume) is usually applied once a day for the first weeks (maximum 4 weeks), then the dose is gradually reduced to 0.5 g of cream (1/2 of the applicator's volume) twice a week.
If necessary, the dose can be increased to a maximum of 1 g of cream per day (full applicator volume, equivalent to 1 mg of estriol). This dose should not be exceeded.
The cream is applied vaginally using the enclosed reusable applicator, in a supine position with legs slightly apart. Alternatively, when applied to the external genitalia, a thin layer of the appropriate amount (1/2 of the applicator's volume) of cream should be applied and rubbed in with the fingers.
To promote wound healing in postmenopausal women who have undergone vaginal surgery, 0.5 g of cream is usually applied once a day for 2 weeks before surgery and 0.5 g of cream twice a week for 2 weeks after surgery.
To facilitate the interpretation of cervical smear results in postmenopausal women, 0.5 g of cream (1/2 of the applicator's volume) is usually applied every other day in the week preceding the smear.
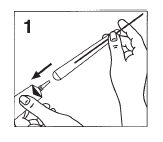
Oekolp is best inserted deep into the vagina, in the evening before bedtime, using the applicator (fig. 1-3).
- 1 - 3).
To administer 0.5 g of cream (1/2 of the applicator's volume), the green plunger of the applicator should be pulled out about halfway until a noticeable resistance is felt. The plunger will then protrude from the applicator by about 6 cm. To apply 1 g of cream (full applicator volume), the plunger should be pulled out completely until a resistance is felt. The plunger will then protrude from the applicator by about 10 cm. Then, open the tube and place the applicator on the tube (1).
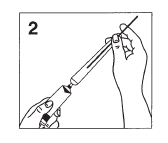
Pressing the tube will fill the applicator with cream (2).
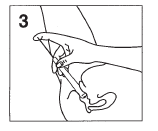
Then, remove the applicator from the tube and carefully insert it as far as possible into the vagina, remaining in a supine position with legs slightly apart. By gently pressing the green plunger, the cream will be released into the vagina (3).
After use, the applicator should be washed in warm water for about 30 seconds. The green plunger can also be removed. To do this, press the plunger into the applicator with the rounded end until a slight resistance is overcome, and then pull it out completely from the other end (the wide end of the applicator).
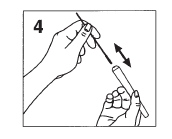
After cleaning and drying, the green plunger should be reinserted into the wide end of the applicator and pushed in completely until a slight resistance is felt again. The applicator is then ready for reuse.
When applying to the external genitalia, a thin layer of the appropriate amount (1/2 of the applicator's volume) of cream should be applied.
Before each reuse, the applicator should be inspected for visible damage. An applicator with visible damage should not be reused and should be discarded with household waste.
The doctor will try to prescribe the lowest possible dose, which should be taken for the shortest duration necessary to alleviate symptoms.
If the patient feels that the effect of Oekolp is too strong or too weak, they should consult a doctor.
Using more than the recommended dose of Oekolp
In case of using a higher dose than recommended, a doctor or pharmacist should be consulted immediately.
In case of swallowing the cream, it does not pose a risk to health and life. However, a doctor should be informed. Symptoms of overdose are usually nausea and vomiting; in women, bleeding from the genital tract may also occur after a few days.
Missing a dose of Oekolp
A double dose should not be used to make up for a missed dose.
If a dose is missed, it should be taken as soon as possible, unless it is the day of the next application. If the missed dose is noticed on the day of the next application, the missed dose should be skipped and the next doses taken according to the previously established schedule.
Stopping Oekolp treatment
If treatment is stopped, the doctor should be consulted to discuss how to resume taking the medicine.
Need for surgery
Patients who are to undergo surgery should inform the surgeon that they are using Oekolp. It may be necessary to stop using Oekolp about 4 to 6 weeks before surgery to reduce the risk of blood clots (see section 2 "Blood clots in veins (venous thrombosis)"). The doctor should be asked when it is possible to resume Oekolp treatment.
In case of any further doubts about using this medicine, a doctor or pharmacist should be consulted.
4. Possible side effects
Like all medicines, Oekolp can cause side effects, although not everybody gets them.
The following diseases are reported more frequently in women using HRT medications that circulate in the blood than in those not using HRT. This risk is lower for vaginally administered medicines like Oekolp:
- ovarian cancer
- presence of blood clots in veins of the legs or lungs (venous thromboembolic disease)
- stroke
- possible memory loss in case of starting HRT at an age over 65.
More information on side effects can be found in section 2.
Depending on the doses used and the patient's sensitivity, the following side effects may occur:
- breast swelling and tenderness
- mild vaginal bleeding
- increased vaginal discharge
- nausea
- fluid retention in the body, usually manifesting as swelling of the ankles or feet
- local irritation or itching
- flu-like symptoms. In most patients, these symptoms will disappear after the first few weeks of treatment.
The following side effects have been reported during the use of other HRT medications:
- gallbladder inflammation
- various skin disorders:
- skin discoloration, especially on the face or neck (chloasma)
- painful red lumps on the skin (erythema nodosum)
- rash with plate-like, red lesions or ulcers (erythema multiforme).
Reporting side effects
If any side effects occur, including those not listed in this leaflet, a doctor or pharmacist should be informed.
Side effects can be reported directly to the Department of Drug Safety, Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, tel.: 22 49-21-301, fax: 22 49-21-309, website: https://smz.ezdrowie.gov.pl.
Side effects can also be reported to the marketing authorization holder.
Reporting side effects will help to gather more information on the safety of the medicine.
5. How to store Oekolp
The medicine should be stored out of sight and reach of children.
Do not use this medicine after the expiry date stated on the tube and carton after "Expiry date". The expiry date refers to the last day of the month.
The medicine should be stored at a temperature below 25°C.
Medicines should not be disposed of via wastewater or household waste. A pharmacist should be asked how to dispose of unused medicines. This will help protect the environment.
6. Contents of the pack and other information
What Oekolp contains
- The active substance of the medicine is estriol, 1 milligram per gram.
- The other ingredients are: decylamine hydrochloride, sodium docuzate, propylene glycol, dimethicone 350, self-emulsifying glyceryl monostearate, medium-chain triglycerides, Softisan 601 consisting of 80-90% mono-, di-, triglycerides of saturated fatty acids (C8-C18) and 10-20% cetostearyl ether of macrogol, purified water.
What Oekolp looks like and contents of the pack
Homogeneous, white cream. Aluminum tube with a plastic applicator in a cardboard box.
The pack contains 25 g of cream.
Marketing authorization holder and manufacturer
DR. KADE Pharmazeutische Fabrik GmbH
Rigistrasse 2
12277 Berlin
Germany
For more detailed information, please contact the representative of the marketing authorization holder:
Kadefarm Sp. z o.o.
Sierosław, ul. Gipsowa 18
62-080 Tarnowo Podgórne, Poland
Phone: +48 61 862 99 43
e-mail: [email protected]
Date of last revision of the leaflet:
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterDr. Kade Pharmazeutische Fabrik GmbH
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to OekolpDosage form: Gel, 50 mcg/gActive substance: estriolManufacturer: Italfarmaco S.A.Prescription requiredDosage form: Suppositories, 0.5 mgActive substance: estriolManufacturer: Dr. Kade Pharmazeutische Fabrik GmbHPrescription requiredDosage form: Suppositories, 0.5 mgActive substance: estriolPrescription required
Alternatives to Oekolp in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Oekolp in Ukraine
Alternative to Oekolp in Spain
Online doctors for Oekolp
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Oekolp – subject to medical assessment and local rules.









