
Mivacurium Kalceks
Ask a doctor about a prescription for Mivacurium Kalceks

How to use Mivacurium Kalceks
Package Leaflet: Information for the User
Mivacurium Kalceks, 2 mg/mL, Solution for Injection/Infusion
Mivacurium
Read the package leaflet carefully before using the medicine, as it contains important information for the patient.
- Keep this package leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or nurse.
- If you experience any side effects, talk to your doctor or nurse. See section 4.
Table of Contents of the Package Leaflet
- 1. What is Mivacurium Kalceks and what is it used for
- 2. Important information before using Mivacurium Kalceks
- 3. How to use Mivacurium Kalceks
- 4. Possible side effects
- 5. How to store Mivacurium Kalceks
- 6. Contents of the pack and other information
1. What is Mivacurium Kalceks and what is it used for
Mivacurium Kalceks contains the active substance mivacurium. This medicine belongs to a group of muscle relaxants.
This medicine is used:
- to relax muscles during surgery in adults, adolescents, and children from 2 months of age and older, including heart surgery;
- to facilitate the insertion of a tube into the trachea (tracheal intubation), if the patient needs help with breathing.
For more information about this medicine, consult your doctor.
2. Important information before using Mivacurium Kalceks
When not to use Mivacurium Kalceks
- if the patient is allergic to mivacurium or any of the other ingredients of this medicine (listed in section 6);
- if the patient has been diagnosed with abnormal genetic enzyme activity (cholinesterase);
- if the patient or their family has had a bad reaction to an anesthetic in the past.
If the patient is unsure whether any of the above applies to them, they should talk to their doctor or nurse before using this medicine.
Warnings and precautions
Before starting treatment with this medicine, the patient should discuss the following with their doctor or nurse:
- if the patient has muscle weakness, fatigue, or difficulty coordinating movements (myasthenia gravis) or another neuromuscular disease;
- if the patient has a burn that requires medical treatment;
- if the patient has ever had an allergic reaction to a muscle relaxant given during surgery;
- if the patient is sensitive to drops in blood pressure;
- if the patient has undergone a blood cleansing procedure called plasmapheresis;
- if the patient has received donor plasma (plasma exchange);
- if the patient has undergone heart-lung bypass surgery (a procedure that temporarily takes over the function of the heart and lungs during surgery);
- if the patient has lower than normal blood volume (hypovolemia);
- if the patient has an acid-base imbalance in the body;
- if the patient has abnormal levels of sodium, potassium, or calcium in the body;
- if the patient is pregnant or has given birth in the last 6 weeks;
- if the patient has a genetically abnormal cholinesterase enzyme;
- if the patient is particularly sensitive to histamine or has asthma.
Before using this medicine, the patient should talk to their doctor if they have or have had any of the following:
- tetanus;
- severe or prolonged infections such as tuberculosis;
- any prolonged illness after which the patient is weakened;
- cancer;
- anemia (reduced red blood cell count);
- malnutrition;
- hypothyroidism;
- heart disease;
- stomach ulcers;
- burns;
- liver or kidney disease;
- collagen diseases (collagenosis or connective tissue diseases).
If the patient is unsure whether any of the above applies to them, they should talk to their doctor or nurse before using this medicine.
Children
This medicine must not be given to children under 2 months of age.
Mivacurium Kalceks and other medicines
The patient should tell their doctor or nurse about all medicines they are taking or have recently taken, including those obtained without a prescription, including herbal medicines.
This is because these medicines may affect the effectiveness of Mivacurium Kalceks or cause side effects.
In particular, the patient should tell their doctor or nurse if they are taking any of the following medicines:
- anesthetics such as ketamine, enflurane, isoflurane, sevoflurane, and halothane (used to reduce sensation and pain during surgical procedures);
- muscle relaxants such as succinylcholine chloride and pancuronium;
- antibiotics such as aminoglycosides, polymyxins, spectinomycin, tetracyclines, lincomycin, and clindamycin (used to treat infections);
- medicines for irregular heartbeat, such as propranolol (also used to treat high blood pressure), lidocaine, procainamide, quinidine, and calcium channel blockers (anti-arrhythmic medicines);
- diuretics such as furosemide, thiazides, mannitol, and acetazolamide;
- medicines for arthritis, such as chloroquine or D-penicillamine;
- corticosteroids;
- medicines for seizures (epilepsy), such as phenytoin;
- medicines used for mental illnesses, such as lithium, monoamine oxidase inhibitors (MAOIs), selective serotonin reuptake inhibitors (SSRIs), or chlorpromazine (which may also be used for nausea);
- medicines containing magnesium, such as those used to treat indigestion and heartburn;
- nerve block medicines such as trimethaphan and hexamethonium;
- medicines for chest pain (angina), such as oxprenolol (also used to treat high blood pressure);
- bambuterol (used to treat asthma);
- medicines that may decrease plasma cholinesterase levels, such as anticancer medicines, echothiophate iodide, organophosphorus compounds, cholinesterase inhibitors, and some hormones.
Pregnancy and breastfeeding
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a baby, they should ask their doctor for advice before using this medicine.
Driving and using machines
Driving or operating machinery too soon after surgery may be dangerous. The doctor will tell the patient how long they need to wait before they can drive and use machines.
3. How to use Mivacurium Kalceks
The patient will never be expected to administer this medicine themselves. They will always receive it from a qualified person.
This medicine can be given:
- as a single injection into a vein (intravenous bolus injection);
- as a continuous intravenous infusion. The medicine is then given slowly over a long period.
The doctor will decide on the route of administration and the dose the patient will receive. It will depend on:
- the patient's body weight;
- the required degree and duration of muscle relaxation;
- the patient's expected response to the medicine.
This medicine must not be used in children under 2 months of age.
Overdose of Mivacurium Kalceks
This medicine should always be given under strictly controlled conditions. However, if the patient thinks they have been given too much medicine, they should tell their doctor or nurse immediately.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Allergic reactions (may occur in less than 1 in 10,000 patients)
If the patient experiences an allergic reaction, they should tell their doctor or nurse immediately. Symptoms may include:
- sudden wheezing, chest pain, or tightness in the chest
- swelling of the eyelids, face, lips, tongue, or throat
- hives or itching on any part of the body
- collapse (sudden failure of blood circulation)
The patient should tell their doctor or nurse if they notice any of the following:
Very common (may occur in more than 1 in 10 patients)
- redness of the skin
Uncommon (may occur in less than 1 in 100 patients)
- increased heart rate
- decreased blood pressure
- wheezing or coughing
- rash or hives (hives or "hives" anywhere on the body)
Reporting side effects
If side effects occur, including any not listed in this package leaflet, the patient should tell their doctor or pharmacist. Side effects can be reported directly to the Department of Adverse Reaction Monitoring of Medicinal Products, Medical Devices, and Biocidal Products
Al. Jerozolimskie 181C
PL-02-222 Warsaw
Phone: +48 22 49 21 301
Fax: +48 22 49 21 309
Website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
Reporting side effects will help to gather more information on the safety of this medicine.
5. How to store Mivacurium Kalceks
The medicine should be stored out of sight and reach of children.
Do not use this medicine after the expiry date stated on the carton after "Expiry Date" and on the ampoule after "EXP". The expiry date refers to the last day of the month stated.
Store in a refrigerator (2°C – 8°C).
Shelf-life after dilution
Chemical and physical stability has been demonstrated for 48 hours at 30°C and 2 to 8°C after dilution with infusion solutions (listed below) at a concentration of 0,5 mg/mL.
From a microbiological point of view, the diluted solution should be used immediately. If not used immediately, the responsibility for the storage time and conditions before use lies with the user. The storage time of the solution should not normally exceed 24 hours at 2 to 8°C, unless the dilution has taken place in controlled and validated aseptic conditions.
Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Contents of the pack and other information
What Mivacurium Kalceks contains
- The active substance is mivacurium. 1 mL of solution contains 2 mg of mivacurium (as mivacurium chloride). Each 5 mL ampoule contains 10 mg of mivacurium (as mivacurium chloride). Each 10 mL ampoule contains 20 mg of mivacurium (as mivacurium chloride).
- The other ingredient is water for injections.
What Mivacurium Kalceks looks like and contents of the pack
Clear, colorless or pale yellow solution, free from visible particles.
5 mL or 10 mL solution in ampoules made of colorless glass type I, with one break point.
Ampoules are packed in a blister. Blisters are packed in a cardboard box.
Pack sizes:
5 or 10 ampoules of 5 mL
5 or 10 ampoules of 10 mL
Not all pack sizes may be marketed.
Marketing authorization holder and manufacturer
AS KALCEKS
Krustpils iela 71E
LV-1057 Rīga
Latvia
Phone: +371 67083320
Email: [email protected]
This medicine is authorized in the Member States of the European Economic Area under the following names:
Latvia
Mivacurium Kalceks 2 mg/ml šķīdums injekcijām/infūzijām
Germany
Mivacurium Kalceks 2 mg/ml Injektions-/Infusionslösung
Poland
Mivacurium Kalceks
Date of last revision of the package leaflet:
---------------------------------------------------------------------------------------------------------------------------
Information intended for healthcare professionals only:
Dosing
- Use in injection in adults
Mivacurium Kalceks is given by intravenous injection. The mean dose required to produce 95% suppression of a single twitch response of the adductor pollicis muscle to ulnar nerve stimulation (ED95) is 0.07 mg/kg body weight (range 0.06 to 0.09 mg/kg body weight) in adults anesthetized with narcotic analgesics.
For endotracheal intubation, the following dosing regimens are recommended:
a)
A dose of 0.2 mg/kg body weight administered over 30 seconds provides good or excellent intubating conditions within 2 to 2.5 minutes.
b)
A dose of 0.25 mg/kg body weight administered as a divided dose (0.15 mg/kg body weight, followed by 0.1 mg/kg body weight 30 seconds later) provides good or excellent intubating conditions within 1.5 to 2 minutes of the completion of administration of the first dose.
The recommended dose range for bolus administration in healthy adult patients is from 0.07 to 0.25 mg/kg body weight. The duration of action of the neuromuscular blockade depends on the dose. Doses of 0.07 mg/kg body weight, 0.15 mg/kg body weight, 0.20 mg/kg body weight, and 0.25 mg/kg body weight produce clinically effective neuromuscular blockade for approximately 13, 16, 20, and 23 minutes, respectively.
Doses up to 0.15 mg/kg body weight can be administered over 5 to 15 seconds. Larger doses should be administered over 30 seconds or as divided doses to minimize the risk of cardiovascular side effects.
Full recovery from neuromuscular blockade can be delayed after long or repeated administration of mivacurium. The neuromuscular blockade produced by mivacurium can be reversed by the administration of standard doses of anticholinesterase inhibitors. However, because spontaneous recovery from mivacurium-induced neuromuscular blockade is rapid, reversal of the blockade may not be necessary in routine practice, as it shortens the time to recovery of neuromuscular function by only about 5-6 minutes.
- Use in infusion in adults
To maintain neuromuscular blockade, mivacurium can be administered by continuous infusion. Following the initial dose of mivacurium, a infusion rate of 8 to 10 micrograms/kg body weight/minute (0.5 to 0.6 mg/kg body weight/hour) is recommended. The initial infusion rate should be adjusted based on the patient's response to peripheral nerve stimulation and clinical criteria.
The infusion rate should be adjusted in increments of approximately 1 microgram/kg body weight/minute (0.06 mg/kg body weight/hour). In general, it is recommended to maintain a given infusion rate for at least 3 minutes before making adjustments.
In adult patients anesthetized with narcotic analgesics, an infusion rate of 6 to 7 micrograms/kg body weight/minute (approximately 0.4 mg/kg body weight/hour) maintains 89% to 99% neuromuscular blockade. In patients anesthetized with isoflurane or enflurane, the initial infusion rate of mivacurium should be reduced by approximately 25%. In patients anesthetized with sevoflurane, the infusion rate of mivacurium should be reduced by approximately 50%. In patients anesthetized with halothane, the need to reduce the infusion rate may be less.
Spontaneous recovery from mivacurium-induced neuromuscular blockade after infusion is not dependent on the duration of infusion and is comparable to recovery after bolus administration.
Administration of mivacurium by continuous infusion has not been associated with development of tachyphylaxis or accumulation of neuromuscular blocking effect.
Special patient populations
Pediatric population
Infants and children from 7 months to 12 years
Mivacurium has a higher ED95 (approximately 0.1 mg/kg body weight), a faster onset of action, a shorter duration of clinically effective neuromuscular blockade, and a faster spontaneous recovery from neuromuscular blockade in infants and children from 7 months to 12 years compared to adults.
The recommended dose range for injection in children from 7 months to 12 years is from 0.1 to 0.2 mg/kg body weight, administered over 5 to 15 seconds. A dose of 0.2 mg/kg body weight, administered during stable anesthesia induced by narcotic analgesics or halothane, produces clinically effective neuromuscular blockade for approximately 9 minutes.
For endotracheal intubation in infants and children from 7 months to 12 years, a dose of 0.2 mg/kg body weight of mivacurium is recommended. Maximum neuromuscular blockade usually occurs within 2 minutes of administration of this dose, and intubating conditions are usually suitable within this time.
Infants and children usually require more frequent maintenance doses than adults. Available data suggest that a maintenance dose of 0.1 mg/kg body weight prolongs clinically effective neuromuscular blockade by approximately 6 to 9 minutes during anesthesia induced by narcotic analgesics or halothane.
Infants and children usually require higher infusion rates than adults. During halothane anesthesia, the mean infusion rate required to maintain 89% to 99% neuromuscular blockade in patients from 7 to 23 months of age is approximately 11 micrograms/kg body weight/minute (approximately 0.7 mg/kg body weight/hour) [range: 3 to 26 micrograms/kg body weight/minute (approximately 0.2 to 1.6 mg/kg body weight/hour)].
In children from 2 to 12 years of age, the equivalent mean infusion rate is approximately 13 to 14 micrograms/kg body weight/minute (approximately 0.8 mg/kg body weight/hour) [range: 5 to 31 micrograms/kg body weight/minute (approximately 0.3 to 1.9 mg/kg body weight/hour)], during halothane or narcotic analgesic anesthesia.
Neuromuscular blockade produced by mivacurium is potentiated by concurrent administration of inhalational anesthetics. Clinical studies have demonstrated that in children from 2 to 12 years of age, the infusion rate of mivacurium should be reduced by approximately 70% during sevoflurane anesthesia.
Spontaneous recovery from neuromuscular blockade occurs within approximately 10 minutes of the start of recovery.
Infants from 2 to 6 months
Mivacurium has a similar ED95 compared to adults (approximately 0.07 mg/kg body weight), but a faster onset of action, a shorter duration of clinically effective neuromuscular blockade, and a faster spontaneous recovery from neuromuscular blockade in infants from 2 to 6 months.
The recommended dose range for injection in infants from 2 to 6 months is from 0.1 to 0.15 mg/kg body weight, administered over 5 to 15 seconds. A dose of 0.15 mg/kg body weight, administered during stable anesthesia induced by halothane, produces clinically effective neuromuscular blockade for approximately 9 minutes.
A dose of 0.15 mg/kg body weight of mivacurium is recommended for endotracheal intubation in infants from 2 to 6 months. Maximum neuromuscular blockade usually occurs within approximately 1.4 minutes of administration of this dose, and intubating conditions are usually suitable within this time.
Infants from 2 to 6 months usually require more frequent maintenance doses than adults. Available data suggest that a maintenance dose of 0.1 mg/kg body weight prolongs clinically effective neuromuscular blockade by approximately 7 minutes during halothane anesthesia.
Infants from 2 to 6 months usually require higher infusion rates than adults. The mean infusion rate required to maintain 89% to 99% neuromuscular blockade during halothane anesthesia is approximately 11 micrograms/kg body weight/minute (approximately 0.7 mg/kg body weight/hour) [range: 4 to 24 micrograms/kg body weight/minute (approximately 0.2 to 1.5 mg/kg body weight/hour)].
Spontaneous recovery from neuromuscular blockade occurs within approximately 10 minutes of the start of recovery.
Newborns and infants below 2 months
The safety and efficacy of mivacurium chloride in newborns and infants below 2 months of age have not been established. No dosage recommendations can be made.
Elderly patients
In elderly patients receiving a single dose of mivacurium by rapid intravenous injection, the time to onset of action and the duration and rate of recovery of neuromuscular blockade may be prolonged by approximately 20 to 30% compared to younger patients. Elderly patients may require slower infusion rates or less frequent maintenance doses when administered by rapid intravenous injection.
Patients with cardiovascular disease
Patients with clinically significant cardiovascular disease should receive the initial dose of mivacurium over at least 60 seconds. When administered in this manner, mivacurium has been shown to produce minimal hemodynamic changes in patients undergoing cardiac surgery.
Patients with renal impairment
In patients with end-stage renal failure, the clinically effective neuromuscular blockade produced by 0.15 mg/kg body weight of mivacurium is prolonged by approximately 1.5 times compared to patients with normal renal function. Therefore, the dose of mivacurium should be adjusted according to the individual patient's clinical response.
Prolonged and enhanced neuromuscular blockade may also occur in patients with acute or chronic renal failure due to decreased plasma cholinesterase activity.
Patients with hepatic impairment
In patients with end-stage liver disease, the clinically effective neuromuscular blockade produced by 0.15 mg/kg body weight of mivacurium is prolonged by approximately 3 times compared to patients with normal liver function. This prolongation of action is associated with decreased plasma cholinesterase activity in these patients. Therefore, the dose of mivacurium should be adjusted according to the individual patient's clinical response.
Patients with decreased plasma cholinesterase activity
Mivacurium is metabolized by plasma cholinesterase. Plasma cholinesterase activity may be decreased in patients with genetic abnormalities of plasma cholinesterase (e.g., patients who are heterozygous or homozygous for the atypical gene for plasma cholinesterase) and in various disease states or after the administration of certain drugs. In patients with decreased plasma cholinesterase activity, there may be an increased risk of prolonged neuromuscular blockade after administration of mivacurium. A small decrease in plasma cholinesterase activity (i.e., to 20% of the lower limit of normal) does not have a clinically significant effect on the duration of action.
Patients with obesity
In obese patients (greater than 30% above ideal body weight), the initial dose of mivacurium should be calculated based on ideal body weight, rather than actual body weight.
Monitoring of patients
As with all neuromuscular blocking agents, it is recommended that neuromuscular function be monitored when using mivacurium in order to individualize dosage requirements.
With mivacurium, there is no significant decrease in the response to train-of-four stimulation. Intubating conditions are usually suitable before complete abolition of the response to train-of-four stimulation of the adductor pollicis muscle.
Route of administration
For intravenous use.
This product does not contain antimicrobial preservatives and is intended for single use only.
Overdose
Symptoms and signs
Prolonged muscle paralysis and its consequences are the main symptoms of overdose of neuromuscular blocking agents. However, there is an increased risk of hemodynamic side effects, particularly hypotension.
Treatment
Until spontaneous recovery of adequate respiratory function, it is essential to maintain a patent airway and to provide ventilation with positive pressure.
Administration of anticholinesterase inhibitors, together with atropine or glycopyrrolate, when signs of spontaneous recovery from neuromuscular blockade first appear, may accelerate recovery.
Appropriate positioning of the patient and administration of fluids or vasoactive agents as needed may support cardiovascular function.
Incompatibilities
Mivacurium solution has an acidic pH (approximately 4.5) and should not be mixed with strongly alkaline solutions, e.g., barbiturates.
This medicinal product must not be mixed with other medicinal products except those mentioned below.
Instructions for use and disposal
For single use only.
The ampoule should be inspected visually before use. Only clear and particle-free solutions should be used.
After opening, the medicinal product should be used immediately.
Because the product does not contain antimicrobial preservatives, the mivacurium solution should be used in completely aseptic conditions, and any dilution should be made just prior to use. Any unused solution in opened ampoules should be discarded.
It has been demonstrated that mivacurium can be combined with certain commonly used anaesthetic drugs in solution, which are acidic in nature. When mivacurium and other anaesthetic drugs are administered through the same intravenous line or cannula, and compatibility has not been established, the line should be flushed with isotonic sodium chloride solution between administration of each drug.
Mivacurium Kalceks is compatible with the following infusion solutions:
- 9 mg/mL (0.9%) sodium chloride solution
- 50 mg/mL (5%) glucose solution for infusion
- 1.8 mg/mL (0.18%) sodium chloride and 40 mg/mL (4%) glucose solution
- Ringer's solution with lactate
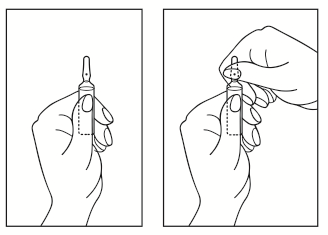
Instructions for opening the ampoule
- 1) Turn the ampoule so that the colored dot is facing upwards. If there is solution in the upper part of the ampoule, gently tap with a finger to move all the solution to the lower part of the ampoule.
- 2) Use both hands to open the ampoule; holding the lower part of the ampoule in one hand, use the other hand to break off the upper part of the ampoule in the direction of the colored dot (see picture below).
- Country of registration
- Active substance
- Prescription requiredNo
- ImporterAS Kalceks
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Mivacurium KalceksDosage form: Solution, 2 mg/mlActive substance: mivacurium chloridePrescription not requiredDosage form: Powder, 4 mgActive substance: pipecuronium bromideManufacturer: Gedeon Richter Plc.Prescription not requiredDosage form: Solution, 10 mg/mlActive substance: atracuriumManufacturer: Akciju sabiedriba "Kalceks"Prescription not required
Alternatives to Mivacurium Kalceks in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Mivacurium Kalceks in Spain
Online doctors for Mivacurium Kalceks
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Mivacurium Kalceks – subject to medical assessment and local rules.














