
Furosemide Kabi
Ask a doctor about a prescription for Furosemide Kabi

How to use Furosemide Kabi
Leaflet attached to the packaging: Information for the user
Furosemide Kabi, 20 mg/2 mL, solution for injection/infusion
Furosemide
You should carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient.
- You should keep this leaflet, so that you can read it again if you need to.
- If you have any doubts, you should consult a doctor or nurse.
- This medicine has been prescribed specifically for you. Do not pass it on to others. The medicine may harm another person, even if their symptoms are the same.
- If the patient experiences any side effects, including any side effects not listed in the leaflet, they should tell their doctor or nurse. See section 4.
Table of contents of the leaflet
- 1. What is Furosemide Kabi and what is it used for
- 2. Important information before using Furosemide Kabi
- 3. How to use Furosemide Kabi
- 4. Possible side effects
- 5. How to store Furosemide Kabi
- 6. Package contents and other information
1. What is Furosemide Kabi and what is it used for
Furosemide Kabi belongs to a group of diuretic medicines. Furosemide increases the amount of urine produced by the body.
Furosemide is used to relieve symptoms caused by too much fluid in the body (edema). Excess fluid in the body may be caused by:
- heart diseases,
- liver diseases,
- kidney diseases. The doctor recommends using furosemide if:
- rapid and effective removal of excess fluid is required;
- the patient cannot take this type of medicine orally or in emergency situations;
- the patient has too much fluid around the heart, lungs, liver, or kidneys;
- there is very high blood pressure that can lead to life-threatening conditions (hypertensive crisis).
2. Important information before using Furosemide Kabi
When not to use Furosemide Kabi:
- if the patient is allergic to furosemide or any of the other ingredients of this medicine (listed in section 6);
- if the patient is allergic to sulfonamide antibiotics;
- in case of significant dehydration (loss of a significant amount of fluid, e.g. due to severe diarrhea or vomiting);
- in case of kidney failure and no urine excretion, despite the administration of furosemide;
- in case of kidney failure resulting from toxicity to the kidneys or liver;
- if the patient has a very low level of potassium or sodium in the blood;
- if the patient is in a coma due to liver failure;
- during breastfeeding. In case of doubts related to the use of the medicine, you should consult a doctor or pharmacist.
Warnings and precautions
Before starting to use Furosemide Kabi, you should discuss it with your doctor or nurse if:
- there are urinary disorders caused by narrowing of the urinary tract (e.g. related to prostate enlargement);
- the patient has diabetes;
- there is low blood pressure or sudden drops in blood pressure (this is especially important for patients with coronary artery or cerebral artery narrowing);
- there is liver disease (e.g. cirrhosis);
- there are kidney diseases (e.g. nephrotic syndrome);
- the patient is dehydrated (loss of fluids due to severe diarrhea or vomiting), as this condition may cause fainting or thrombosis;
- there is gout (pain or inflammation of the joints), caused by high levels of uric acid (a metabolic product) in the blood;
- there is a disease with an inflammatory background, called systemic lupus erythematosus, an immune system disease that attacks the skin, bones, joints, and internal organs;
- there are hearing disorders;
- the patient is using sorbitol (a sugar substitute for diabetic patients);
- the patient is using medicines that can cause life-threatening, irregular heart rhythm (QT interval prolongation);
- the patient is using lithium;
- there is porphyria (a disease in which oxygen binding by red blood cells is disrupted and a purple discoloration of the urine appears);
- there is increased skin sensitivity to sunlight (photosensitivity);
- the patient is an athlete - the medicine may cause a positive result in doping tests;
- the patient is elderly, uses other medicines that may cause low blood pressure, or has other medical conditions that are associated with a risk of low blood pressure. Administration of furosemide to premature infants may cause kidney stones or kidney calcification. If any of the above conditions apply to the patient, the doctor may change the treatment or provide appropriate advice. During the use of Furosemide Kabi, the doctor may recommend regular blood sugar or uric acid tests. The doctor may also recommend monitoring the levels of basic electrolytes, such as sodium and potassium, which is especially important in case of vomiting or diarrhea.
Furosemide Kabi and other medicines
You should tell your doctor or nurse about all the medicines you are taking, have recently taken, or plan to take, including those available without a prescription. This is important because some medicines should not be taken at the same time as Furosemide Kabi.
Particularly, you should inform your doctor if you are taking any of the following medicines:
- Lithium (used in mood disorders) - concurrent use with furosemide may increase the effect and side effects of lithium. The doctor will recommend concurrent use only if absolutely necessary and will monitor lithium levels in the blood. If necessary, the doctor will adjust the lithium dose.
- Risperidone, used in the treatment of certain psychoses.
- Cardiac glycosides, such as digoxin - the doctor may adjust the dose of the medicine.
- Medicines used to treat high blood pressure, including thiazide diuretics (e.g. bendroflumethiazide or hydrochlorothiazide), ACE inhibitors (e.g. lisinopril), angiotensin II antagonists (e.g. losartan), as furosemide may cause too much lowering of blood pressure. The doctor may adjust the dose of furosemide.
- Medicines that lower cholesterol and lipid levels, such as fibrates (e.g. clofibrate, fenofibrate, or bezafibrate), as the effect of furosemide may be increased.
- Medicines used to treat diabetes, such as metformin and insulin, as high blood sugar levels may occur.
- Anti-inflammatory medicines, including NSAIDs (e.g. aspirin or celecoxib), as they may weaken the effect of furosemide. High doses of painkillers (salicylates) may increase the side effects of furosemide.
- Anti-inflammatory and anti-allergic medicines, such as corticosteroids, carbenoxolone (used to treat stomach ulcers), or laxatives, as they may affect sodium and potassium levels in the blood when used concurrently with furosemide. Licorice has the same effect as carbenoxolone. The doctor will recommend monitoring potassium levels in the blood.
- Medicines administered by injection during surgical procedures, including tubocurarine, curare derivatives, and succinylcholine.
- Chloral hydrate (used in sleep disorders), as intravenous administration of furosemide within 24 hours before administration of chloral hydrate may cause sudden flushing of the face, excessive sweating, anxiety, nausea, increased blood pressure, and rapid heartbeat. Therefore, concurrent use of furosemide and chloral hydrate is not recommended.
- Phenytoin or phenobarbital, used in the treatment of epilepsy, as the effect of furosemide may be weakened.
- Theophylline, used in the treatment of asthma, as furosemide may increase its effect.
- Antibiotics, such as cephalosporins, polymyxins, aminoglycosides, or quinolones, and other medicines that impair kidney function, such as immunosuppressants, iodine-based contrast agents, foscarnet, or pentamidine, as furosemide may increase their effect.
- Amphotericin B used for a long time (used to treat fungal infections).
- Probenecid (used to protect the kidneys with other medicines), as it may weaken the effect of furosemide.
- Organic platinum compounds (used to treat certain cancers), as furosemide may increase the side effects of these medicines.
- Methotrexate, used to treat certain cancers and severe arthritis, as it may weaken the effect of furosemide.
- Medicines that increase blood pressure (vasopressors), as concurrent use with furosemide may weaken their effect.
- Aminoglutethimide, used to inhibit the production of corticosteroids (in Cushing's syndrome), as it may increase the side effects of furosemide.
- Carbamazepine, used to treat epilepsy or schizophrenia, as it may increase the side effects of furosemide.
- Cyclosporine, used to prevent rejection of a transplanted organ, as it increases the risk of gouty arthritis (joint pain).
- Medicines that affect heart function, such as amiodarone, sotalol, dofetilide, ibutilide, as furosemide may increase their effect.
- Medicines administered by injection before X-ray examination.
- Levothyroxine, used in thyroid diseases.
Furosemide Kabi with food, drink, and alcohol
Food does not affect the action of this medicine when administered intravenously. During the use of furosemide, the patient can eat and drink as usual. There is no need to change the diet, unless the doctor recommends otherwise.
Pregnancy, breastfeeding, and fertility
Furosemide should not be used during pregnancy, unless it is absolutely necessary.
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a child, they should consult a doctor or pharmacist before using this medicine.
- Furosemide may pass from the mother's body to the child.
- Furosemide is used in pregnant women only if absolutely necessary. Furosemide Kabi should not be used during breastfeeding.
- The medicine passes into breast milk. Before using any medicine, you should consult a doctor or pharmacist.
Driving and using machines
Furosemide Kabi may impair concentration. You should not drive vehicles or operate machines, as furosemide may impair concentration (see section 4, "Possible side effects").
- 4. "Possible side effects").
Furosemide Kabi contains sodium
This medicine contains 3.7 mg of sodium (the main component of table salt) per mL. This corresponds to 0.2% of the maximum recommended daily intake of sodium in the diet for adults.
3. How to use Furosemide Kabi
This medicine should always be used as directed by your doctor or nurse. If you have any doubts, you should consult a doctor or nurse.
Furosemide Kabi is administered by a doctor or nurse:
- by slow injection into a vein (intravenously) or
- in exceptional cases, into a muscle (intramuscularly). The doctor will determine the correct dose, administration time, and duration of treatment. This depends on the patient's age, weight, medical history, other medicines the patient is taking, and the type and severity of the disease.
General recommendations
- Parenteral administration of furosemide is indicated when oral administration is impossible or ineffective (e.g. in case of reduced intestinal absorption) or when rapid action is required.
- In cases where parenteral administration is used, it is recommended to switch to oral administration as soon as possible.
- To achieve optimal efficacy and prevent compensatory reactions, continuous infusion of furosemide is generally preferred over multiple injections, such as bolus injections.
- If continuous infusion of furosemide is not possible during continued treatment after initial administration of one or more injections, it is recommended to administer small doses intravenously at short intervals (about 4 hours) rather than large doses at longer intervals.
- Intravenously, furosemide should be administered by slow injection or infusion. It should not be administered faster than 4 mg per minute, and it should not be mixed with other medicines in the same syringe.
Dosage
Adults
- In the absence of a need to reduce the dose (see below), the recommended initial dose for adults and adolescents over 15 years of age is 20 mg to 40 mg of furosemide administered intravenously (or in exceptional cases, intramuscularly). The maximum dose depends on the individual patient's response to treatment.
- If a higher dose is required, the doctor will administer an additional 20 mg injection. Usually, subsequent doses are administered every 2 hours until the desired fluid loss is achieved.
- In some cases, a higher initial or maintenance dose may be necessary, depending on the patient's condition. The dose is determined by the doctor. If such doses are required, they can be administered by continuous infusion. Children and adolescents (under 18 years of age) Experience with the use of furosemide in children and adolescents is limited. Intravenous administration of furosemide in children and adolescents under 15 years of age is recommended only in exceptional cases. The dosage should be adjusted according to body weight, and the recommended dose is 0.5 to 1 mg/kg body weight per day, up to a maximum total daily dose of 20 mg. Treatment should be switched to oral administration as soon as possible. Elderly patients In elderly patients, the usual initial dose is 20 mg per day. The dose can be gradually increased until the desired fluid loss is achieved. Weight loss due to fluid loss should not exceed 1 kg of body weight per day. If prolonged use of Furosemide Kabi is necessary, the doctor will recommend oral administration (tablets) as soon as possible.
Using a higher dose of Furosemide Kabi than recommended
If the patient is concerned that they have received too much of the medicine, they should immediately inform their doctor.
Symptoms of furosemide overdose include: dryness of the mucous membranes, increased thirst, irregular heartbeat, mood disorders, muscle cramps or pain, nausea or vomiting, extreme fatigue or weakness, slow pulse or loss of appetite.
Missing a dose of Furosemide Kabi
If the patient is concerned that they have missed an injection, they should talk to their doctor or nurse.
In case of any further doubts related to the use of this medicine, you should consult a doctor or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
During treatment with furosemide, the following side effects may occur:
Common (may affect up to 1 in 10 people):
- Hepatic encephalopathy in patients with liver failure (symptoms include memory lapses, seizures, mood changes, coma).
Uncommon (may affect up to 1 in 100 people):
- skin rashes (including itching, redness, peeling), tendency to bruise or increased sensitivity to sunlight;
- blood disorders that can lead to bleeding disorders (with increased risk of bleeding);
- hearing loss (sometimes irreversible).
Rare (may affect up to 1 in 1,000 people):
- nausea or vomiting, diarrhea, constipation, loss of appetite, discomfort in the mouth and stomach;
- hearing disorders (more common in patients with kidney failure) and tinnitus (ringing in the ears);
- anaphylaxis, severe allergic reaction, which can cause rash, swelling, difficulty breathing, and loss of consciousness; in such a case, you should immediatelycontact a doctor;
- kidney damage (interstitial nephritis);
- very low white blood cell count (which can cause life-threatening infections); in such a case, you should immediatelycontact a doctor;
- muscle disorders, including muscle cramps or weakness;
- pain or discomfort at the injection site (especially after intramuscular injection);
- possibility of exacerbation or activation of systemic lupus erythematosus;
- abnormal blood test results (change in the level of substances similar to fats in the blood);
- feeling of numbness or tingling, feeling of spinning (dizziness);
- high fever;
- blurred vision, confusion, drowsiness;
- dryness of the mucous membranes.
Very rare (may affect up to 1 in 10,000 people):
- severe muscle disorders, including tremors, muscle spasms, and cramps (also known as tetany);
- blood disorders that can lead to anemia and decreased immunity to infections;
- pancreatitis, causing severe abdominal pain.
Frequency not known (cannot be estimated from the available data):
- Stevens-Johnson syndrome (formation of blisters and peeling of the skin around the lips, eyes, mouth, nose, and genitals, flu-like symptoms, fever);
- toxic epidermal necrolysis (peeling of large areas of skin, with exposure of the underlying skin);
- acute generalized exanthematous pustulosis (acute febrile drug eruption, also known as AGEP);
- drug reaction with eosinophilia and systemic symptoms (also known as DRESS syndrome);
- dizziness, fainting, and loss of consciousness (due to symptomatic hypotension or other causes), headache;
- exacerbation or activation of systemic lupus erythematosus (with symptoms such as rash, joint pain, fever);
- reports of muscle damage (rhabdomyolysis), often associated with severe hypokalemia.
The following side effects may also occur:
- Low blood pressure, causing fainting or dizziness, which can also cause a feeling of pressure in the head, joint pain, blood clots, or circulatory shock (shock).
- Low potassium levels in the blood, which can cause muscle weakness, numbness, and tingling, minor difficulties in moving limbs, vomiting, bloating, constipation, increased urine production, increased thirst, slow or irregular heartbeat. These disorders occur more frequently in patients with other diseases, such as liver or heart disorders, in case of a diet with low potassium content, or in case of use of other medicines (see "Furosemide Kabi and other medicines"). Significant potassium loss can lead to transient impairment of intestinal motility or to disorders of consciousness, including loss of consciousness in extreme cases. The doctor may recommend regular blood tests and the use of potassium supplements.
- Low sodium, calcium, and magnesium levels in the blood, caused by their increased excretion in the urine. Low sodium levels can cause concentration disorders, calf cramps, loss of appetite, weakness, drowsiness, vomiting, and confusion. Low calcium levels can cause painful muscle cramps. Painful muscle cramps and heart rhythm disorders can also be caused by low magnesium levels in the blood.
Painful muscle cramps and heart rhythm disorders can also be caused by low magnesium levels in the blood.
- Gout - possibility of occurrence or exacerbation.
- Urinary disorders - possibility of exacerbation of disorders.
- Diabetes - possibility of occurrence or exacerbation.
- Liver function disorders or blood changes, which can cause jaundice (yellowing of the skin, dark urine, fatigue).
- Decreased intravascular volume, especially in the elderly, which can cause blood thickening with a tendency to form blood clots in case of significant fluid loss.
- In premature infants, kidney stones or kidney calcification may occur.
- Possibility of maintaining a patent ductus arteriosus in premature infants (this duct is open in unborn children).
Reporting side effects
If you experience any side effects, including any side effects not listed in this leaflet, you should tell your doctor, pharmacist, or nurse. Side effects can be reported directly to the Department of Monitoring of Adverse Reactions to Medicinal Products of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products
Al. Jerozolimskie 181C
02-222 Warsaw
tel.: + 48 22 49 21 301
fax: + 48 22 49 21 309
website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Furosemide Kabi
- The medicine should be stored out of sight and reach of children.
- Do not use this medicine after the expiry date stated on the packaging after EXP. The expiry date refers to the last day of the month stated.
- Ampoules should be stored in the outer packaging to protect them from light.
- Medicines should not be disposed of via wastewater or household waste. You should ask your pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Package contents and other information
What Furosemide Kabi contains
- The active substance of the medicine is furosemide.
- The other ingredients are: sodium chloride, sodium hydroxide, water for injections.
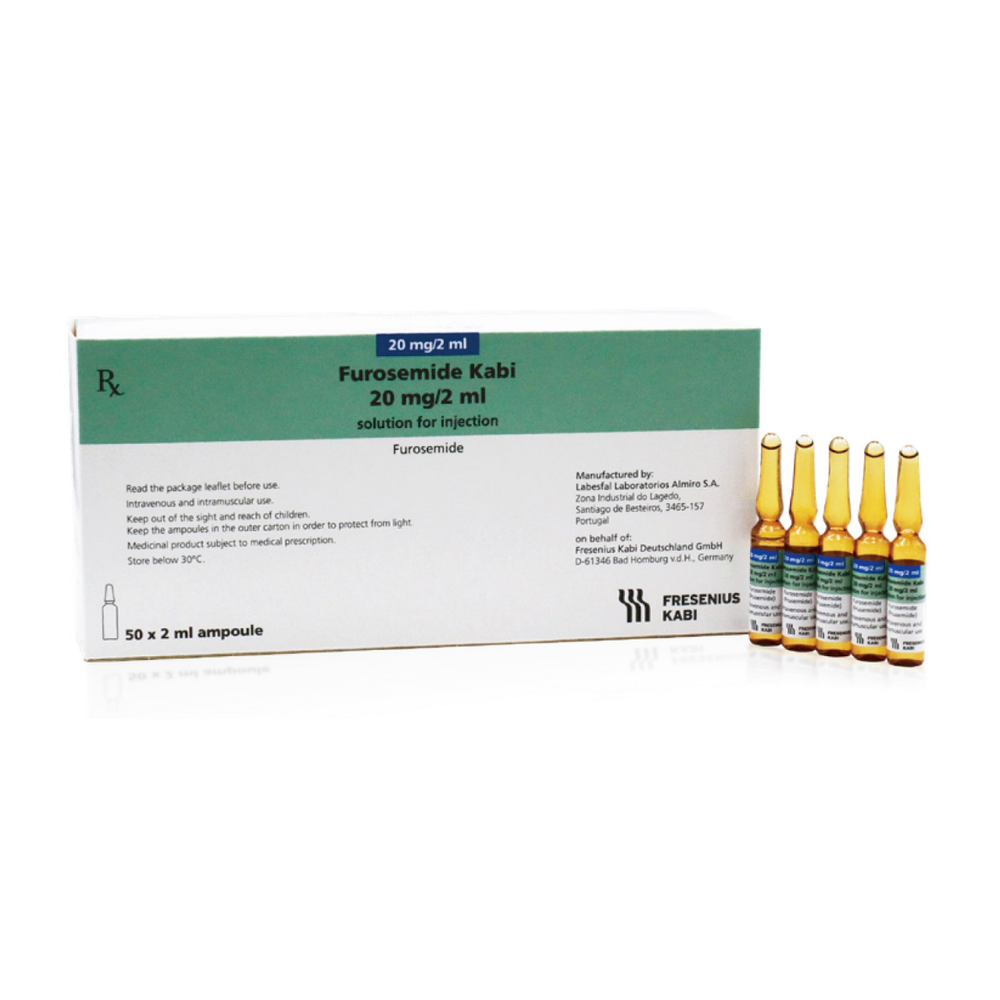
What Furosemide Kabi looks like and what the package contains
Furosemide Kabi is a clear, colorless or almost colorless solution.
The package may contain 5, 50, or 100 ampoules of 2 mL of glass, containing Furosemide Kabi, 20 mg/2 mL, solution for injection/infusion.
Marketing authorization holder
Fresenius Kabi Polska Sp. z o.o.
Al. Jerozolimskie 134
02-305 Warsaw
Manufacturer
LABESFAL - Laboratórios Almiro S.A. (Fresenius Kabi Group)
Lagedo, 3465-157 Santiago de Besteiros
Portugal
To obtain more detailed information, you should contact the marketing authorization holder:
Fresenius Kabi Polska Sp. z o.o.
Al. Jerozolimskie 134
02-305 Warsaw
tel. + 48 22 345 67 89
This medicine is authorized in the Member States of the European Economic Area and in the United Kingdom (Northern Ireland) under the following names:
Belgium
Furosemide Fresenius Kabi 20 mg/2 ml oplossing voor injectie /
infusie
Furosemide Fresenius Kabi 20 mg/2 ml solution injectable /pour
perfusion
Furosemide Fresenius Kabi 20 mg/2 ml Injektionslösung/
Infusionslösung
Czech Republic
Furosemid Kabi
Finland
Furosemide Fresenius Kabi 10 mg/ml injektio-/infuusioneste
Spain
Furosemida Fresenius Kabi 20 mg/2 ml solución inyectable inyectable
y para perfusión EFG
Netherlands
Furosemide Fresenius Kabi 20 mg/2 ml oplossing voor injectie/infusie
Ireland
Furosemide 20mg/2ml solution for injection/infusion
Poland
Furosemide Kabi
Portugal
Furosemida Fresenius Kabi 20mg/2ml solução injectável ou para
perfusão
Slovakia
Furosemid Kabi 20 mg/2 ml, injekcný /infúzny roztok
United Kingdom
(Northern Ireland)
Furosemide 20mg/2ml solution for injection/infusion
Date of last revision of the leaflet:29.05.2023
Information intended for healthcare professionals only:
Method of administration:
Furosemide should be administered intravenously slowly, not faster than 4 mg per minute. Other medicines should not be administered in the same syringe.
Intramuscular administration of furosemide should be limited to exceptional cases when oral or intravenous administration is impossible. Note that intramuscular administration is not suitable for emergency situations, such as pulmonary edema.
The recommended initial dose for adults and adolescents over 15 years of age is 20 mg to 40 mg (1 or 2 ampoules), administered intravenously (or in exceptional cases, intramuscularly). The maximum dose depends on the individual patient's response to treatment. If a higher dose is required, it should be increased by 20 mg and not administered more frequently than every 2 hours.
In adult patients, the maximum recommended daily dose is 1500 mg of furosemide.
Incompatibilities:
Furosemide Kabi can be mixed with neutral or slightly alkaline solutions, with a pH of 7-10, such as 0.9% sodium chloride solution and Ringer's solution with lactate.
Due to the risk of precipitation, furosemide should not be mixed with strongly acidic solutions (pH less than 5.5), such as solutions containing ascorbic acid, noradrenaline, and adrenaline.
A solution with visible particles should not be used.
The medicine is intended for single use, and any unused solution should be discarded.
Shelf life:
3 years
Shelf life after opening:
The medicine should be used immediately after opening.
Shelf life after dilution:
The chemical and physical stability of the medicine is maintained for 24 hours at 25°C, protected from light.
For microbiological reasons, the medicine should be used immediately. If the medicine is not used immediately, the user is responsible for the storage time and conditions before administration. The medicine should not be stored for more than 24 hours at a temperature of 2 to 8°C, unless it has been diluted in controlled and validated aseptic conditions.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterLabesfal - Laboratorios Almiro S.A. (Fresenius Kabi Group)
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Furosemide KabiDosage form: Solution, 10 mg/mlActive substance: furosemidePrescription not requiredDosage form: Solution, 10 mg/mlActive substance: furosemidePrescription requiredDosage form: Solution, 10 mg/mlActive substance: furosemideManufacturer: Laboratórios Basi - Indústria Farmacêutica, S.A.Prescription required
Alternatives to Furosemide Kabi in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Furosemide Kabi in Hiszpania
Alternative to Furosemide Kabi in Ukraina
Online doctors for Furosemide Kabi
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Furosemide Kabi – subject to medical assessment and local rules.










