

Fem 7 Combi

Ask a doctor about a prescription for Fem 7 Combi

How to use Fem 7 Combi
Package Leaflet: Information for the Patient
Fem 7 Combi
Phase I: 50µg/24 h (1.5 mg)
Phase II: 50µg/24 h (1.5 mg) + 10 µg/24 h (1.5 mg)
Transdermal system
(Estradiolum + Levonorgestrelum)
Read the package leaflet carefully before using the medicine, as it contains important information for the patient.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If you experience any side effects, including any not listed in this leaflet, please tell your doctor or pharmacist. See section 4.
Table of Contents of the Leaflet:
- 1. What is Fem 7 Combi and what is it used for
- 2. Important information before using Fem 7 Combi
- 3. How to use Fem 7 Combi
- 4. Possible side effects
- 5. How to store Fem 7 Combi
- 6. Contents of the pack and other information
1. What is Fem 7 Combi and what is it used for
Fem 7 Combiis a transdermal system containing estradiol and levonorgestrel as active substances.
Estradiol in Fem 7 Combi is 17β (beta) estradiol, a hormone identical to natural estradiol, produced mainly in the granulosa cells of the ovarian follicle. In smaller amounts, estrogens are also produced in the corpus luteum, placenta, and adrenal glands. After menopause (when menstruation completely stops), ovarian function decreases, and the body produces only a small amount of estradiol.
The deficiency of estrogens is the cause of various disorders in many women: hot flashes, sleep disturbances, atrophy of the mucous membrane of the uterus and other tissues of the urogenital system, and osteoporosis.
Levonorgestrel belongs to the group of sex hormones, progestogens, which affect the mucous membrane of the uterus in women with an intact uterus. Levonorgestrel reduces the risk of excessive growth of the uterine mucosa and uterine cancer.
Fem 7 Combi is available as a transdermal therapeutic system. This means that the estrogen and levonorgestrel that the body needs to supplement are slowly delivered to the body through the skin using a self-adhesive patch (hormone replacement therapy) to treat unpleasant menopausal symptoms.
Experience with the use of Fem 7 Combi in women over 65 years of age is limited.
Fem 7 Combi is not a contraceptive.
2. Important information before using Fem 7 Combi
When not to use Fem 7 Combi
The use of Fem 7 Combi in children is contraindicated.
Warnings and precautions
Before starting Fem 7 Combi, discuss it with your doctor or pharmacist.
Before starting or restarting hormone replacement therapy, the doctor will perform a thorough medical examination, including a family history. The physical examination (including examination of the pelvic organs and breasts) should take into account the data from the medical history and contraindications and warnings regarding the use of HRT. During treatment, the doctor will perform periodic check-ups, the frequency and type of which should be adapted to the individual needs of the patient. HRT should be used for as long as the benefits of its use outweigh the risks.
If the patient notices changes in the breasts corresponding to breast tumors (see the section "Breast cancer" below), she should inform her doctor, who may refer her for a mammogram.
Situations requiring observation
If any of the following disorders occur, have occurred before, or have worsened during pregnancy or previous hormone therapy, the patient's health must be closely monitored by a doctor.
It should be considered that the mentioned disorders may recur or worsen during treatment with Fem 7 Combi. This applies in particular to such diseases as:
- benign uterine tumors (uterine fibroids) or endometriosis (the presence of fragments of the uterine mucosa in various locations within the pelvis) ;
- previous thromboembolic disorders or risk factors for them (see below);
- risk factors for estrogen-dependent tumors, e.g. breast cancer in first-degree relatives;
- hypertension;
- liver disease (e.g. liver tumor);
- diabetes with vascular changes or without vascular changes;
- gallstones;
- migraine or (severe) headaches;
- systemic lupus erythematosus (an autoimmune disease);
- endometrial hyperplasia in the past (see below);
- epilepsy;
- asthma;
- otosclerosis (a disease affecting the bony labyrinth leading to hearing impairment)
- hereditary and acquired angioedema.
Indications for immediate discontinuation of treatment. Treatment should be discontinued immediately if any of the conditions listed in the section "When not to use Fem 7 Combi" occur or if:
- jaundice or worsening of liver function;
- significant increase in blood pressure;
- appearance of migraine headaches;
- pregnancy
- swelling of the face, tongue, and (or) throat and (or) difficulty swallowing or hives, in combination with difficulty breathing, which suggest angioedema.
Safety of HRT
In addition to the benefits, HRT is associated with certain risks, which the patient should consider when deciding on this type of treatment or its continuation.
Endometrial cancer (cancer of the uterine mucosa)
Long-term administration of estrogens alone increases the risk of endometrial cancer (endometrial cancer). The additional administration of progestogen significantly reduces this risk.
- Patients with an intact uterus are usually prescribed progestogen and estrogen therapy. These substances can be prescribed separately or in the form of a combined drug as part of HRT.
- In the case of patients who have had a hysterectomy (after hysterectomy), the doctor will discuss with the patient the safety of using only estrogen without progestogen.
- In the case of patients who have had a hysterectomy due to endometriosis, in whom residual foci of endometriosis remain, the risk may apply to any fragments of the uterine mucosa remaining in the body. Therefore, the doctor may prescribe HRT consisting of progestogen and estrogen.
Comparison:
Comparing women with an intact uterus who do not use HRT- in approximately 5 out of 1,000of them, the doctor will diagnose uterine cancer between the ages of 50 and 65.
In the case of women using HRT with only estrogens, this number will be 2 to 12 times higher, depending on the dose and duration of HRT.
Adding progestogen to HRT with only estrogens significantly reduces the risk of uterine cancer.
If the patient experiences intermenstrual bleeding or spotting, it is usually not a cause for concern, especially during the first few months of HRT.
If, however, the bleeding or spotting
- persists for longer than the first few months
- occurs for the first time some time after starting HRT, you should inform your doctor. This may indicate that the uterine mucosa has thickened.
Breast cancer
Women with current or past breast cancer should not use HRT.
Data confirm that taking hormone replacement therapy (HRT) in the form of a combination of estrogen and progestogen or only estrogen increases the risk of breast cancer. The additional risk depends on how long the patient uses HRT. This additional risk becomes apparent after 3 years of HRT use.
After stopping HRT, the additional risk will decrease over time, but the risk may persist for 10 years or more if HRT lasted more than 5 years.
The risk of breast cancer is also higher:
- in patients whose close relative (mother, sister, or grandmother) had breast cancer
- in patients with significant overweight
Comparison:
In the case of women between the ages of 50 and 54 who do not use HRT, breast cancer will be diagnosed in approximately 13 to 17 out of 1,000women over a period of 5 years.
In the case of women aged 50 who start 5-year estrogen-only HRT, the number of cases will be 16-17 out of 1,000patients (i.e., 0 to 3 additional cases).
In the case of women aged 50 who start 5-year estrogen-progestogen HRT, the number of cases will be 21 out of 1,000patients (i.e., 4 to 8 additional cases).
In the case of women between the ages of 50 and 59 who do not use HRT, breast cancer will be diagnosed in approximately 27 out of 1,000women over a period of 10 years.
In the case of women aged 50 who start 10-year estrogen-only HRT, the number of cases will be 34 out of 1,000patients (i.e., 7 additional cases).
In the case of women aged 50 who start 10-year estrogen-progestogen HRT, the number of cases will be 48 out of 1,000patients (i.e., 21 additional cases).
If the patient notices changes in the breasts, such as:
- dimples in the breast skin
- changes in the nipple
- any visible or palpable lumps should see a doctor as soon as possible.
Thrombosis
HRT is associated with a higher relative risk of venous thrombosis (deep vein thrombosis), especially in the first year of HRT use.
These thrombi are not always a threat to health and life, but if one of them moves to the lungs, it can cause chest pain, shortness of breath, collapse, and even death. This condition is called pulmonary embolism.
Deep vein thrombosis and pulmonary embolism are examples of venous thromboembolic disease(VTE).
Thrombosis is more likely to occur:
- in patients with significant obesity
- in patients with a history of thrombosis
- if there have been thromboses in the patient's close family
- if the patient has had at least one miscarriage
- if the patient has coagulation disorders requiring treatment with anticoagulant drugs
- in patients who are immobilized for a long time due to major surgery, injury, or illness
- in patients with a rare disease called systemic lupus erythematosus.
If any of these conditions occur in the patient, they should consult a doctor to see if they can start HRT.
Comparison:
Comparing women around the age of 50who do not use HRT- in approximately 3 out of 1,000of them, a thrombus will occur over a period of 5 years.
In the case of women around the age of 50 who use HRT, this number will be 7 out of 1,000.
Comparing women around the age of 60who do not use HRT- in approximately 8 out of 1,000of them, a thrombus will occur over a period of 5 years.
In the case of women around the age of 60 who use HRT, this number will be 17 out of 1,000.
If the patient experiences:
- painful swelling of the leg
- sudden chest pain
- difficulty breathing should see a doctor as soon as possible and not use HRT until the doctor agrees. These may be symptoms of thrombosis.
If the patient is scheduled for surgery, they should inform their doctor. It may be necessary to discontinue HRT 4 to 6 weeks before surgery to reduce the risk of thrombosis. The doctor will inform the patient when they can resume HRT.
Ischemic heart disease
HRT is not recommended for women with current or recent heart disease. If the patient has ever had heart disease, they should consult a doctor to see if they can use HRT.
HRT does not support the prevention of heart disease.
Studies with one type of HRT (conjugated equine estrogens and medroxyprogesterone) have shown that the risk of heart disease may be slightly higher during the first year of treatment. In the case of other HRTs, it is likely that the risk will be similar, but this is not certain.
If the patient experiences:
- chest pain radiating to the arm and neck should see a doctor as soon as possible and not use HRT until the doctor agrees. These may be symptoms of heart disease.
Stroke
Recent studies suggest that HRT slightly increases the risk of stroke. Other factors that may increase the risk of stroke include:
- aging
- high blood pressure
- smoking
- excessive alcohol consumption
- irregular heartbeat
If the patient has the above-mentioned risk factors for strokeor if the patient has had a stroke in the past, they should consult a doctor to see if they can use HRT.
Comparison:
Comparing women around the age of 50who do not use HRT- in approximately 3 out of 1,000of them, a stroke will occur over a period of 5 years.
In the case of women around the age of 50 who use HRT, this number will be 4 out of 1,000.
Comparing women around the age of 60who do not use HRT- in approximately 11 out of 1,000of them, a stroke will occur over a period of 5 years.
In the case of women around the age of 60 who use HRT, this number will be 15 out of 1,000.
Ovarian cancer
Ovarian cancer is rare - much rarer than breast cancer.
The use of HRT containing only estrogens or a combination of estrogens and progestogens is associated with a slightly increased risk of ovarian cancer.
The risk of ovarian cancer depends on age. For example, in women between the ages of 50 and 54 who do not use HRT, ovarian cancer will be diagnosed over a period of 5 years in approximately 2 out of 2,000women.
In women who have taken HRT for 5 years, it will occur in approximately 3 out of 2,000users (i.e., 1 additional case).
Other disorders
Estrogens can cause fluid retention, so patients with heart or kidney disorders should be closely monitored. Patients with severe renal impairment should be closely monitored, as it can be expected that the concentration of the active substances of Fem 7 Combi in the bloodstream will increase.
Women with previous hypertriglyceridemia should be closely monitored during estrogen replacement therapy or other hormone replacement therapy, as rare cases have been reported in which significant increases in triglyceride levels in the blood led to pancreatitis after estrogen use.
Estrogens affect the levels of other hormones and proteins.
Fem 7 Combi and other medicines
The metabolism of estrogens and progestogens may be increased during concurrent use of substances that induce the activity of enzymes that metabolize drugs (especially cytochrome P 450 enzymes), such as antiepileptic drugs (e.g., phenobarbital, phenytoin, carbamazepine, primidone) and anti-infective drugs (rifampicin, rifabutin, nevirapine, efavirenz).
Ritonavir and nelfinavir, although known as potent enzyme inhibitors, have enzyme-inducing properties when used concomitantly with steroid hormones.
Herbal products containing St. John's Wort (Hypericum perforatum) may induce the metabolism of estrogens and progestogens.
With transdermal administration, there is no so-called "first-pass" effect in the liver, so substances that induce enzymes have a smaller effect on estrogens and progestogens administered in this way than on hormones taken orally.
Clinically, accelerated metabolism of estrogens and progestogens may lead to a decrease in the effectiveness of these hormones and disturbances in the profile of menstrual bleeding.
Note! This also applies to drugs taken recently.
Hormone replacement therapy may affect the action of other drugs:
- epilepsy medication (lamotrigine), as it may increase the frequency of seizures;
- drugs used to treat viral hepatitis C (HCV) (such as the treatment regimen using ombitasvir/paritaprevir/ritonavir with dasabuvir or without dasabuvir and the treatment regimen using glecaprevir/pibrentasvir) as it may cause an increase in liver function test parameters in the blood (increased activity of the liver enzyme ALT) in women using combined hormonal contraceptives containing ethinyl estradiol. Fem 7 Combi contains estradiol instead of ethinyl estradiol. It is not known whether an increased activity of the liver enzyme ALT may occur during the use of Fem 7 Combi with such a combination treatment regimen for HCV.
Tell your doctor about all the medicines you are taking now or have taken recently, as well as any medicines you plan to take. Your doctor will give you appropriate instructions.
Lab tests
If a blood test is necessary, inform your doctor or laboratory staff that you are taking Fem 7 Combi, as this medicine may affect the results of some tests.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant, or plan to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Pregnancy
Fem 7 Combi is not indicated for use during pregnancy. If you become pregnant during treatment with Fem 7 Combi, you should stop using the medicine immediately.
Clinical studies conducted on a large number of patients do not show adverse effects of levonorgestrel on the fetus.
The results of epidemiological studies on accidental exposure of the fetus to estrogens and levonorgestrel do not show harmful effects on the embryo and fetus.
Breastfeeding
Fem 7 Combi is not indicated for use during breastfeeding.
Driving and using machines
No effect of Fem 7 Combi on the ability to drive and use machines has been observed.
3. How to use Fem 7 Combi
Always use this medicine exactly as your doctor has told you. If you are not sure, ask your doctor or pharmacist.
Dosage for adults
- Fem 7 Combi is used once a week, i.e., the used patch should be replaced immediately with a new one every 7 days (always on the same day of the week). Fem 7 Combi is intended for continuous sequential treatment.
- Each treatment cycle consists of two types of Fem 7 Combi systems: two systems containing only estradiol (phase I) and two systems containing estradiol and levonorgestrel (phase II).
Use in children and adolescents
The use of Fem 7 Combi in children is contraindicated.
How to start using Fem 7 Combi.
- Treatment should be started by applying one patch.
- In postmenopausal women not using hormone replacement therapy, treatment with Fem 7 Combi can be started at any time
- In women using other hormone replacement therapy products continuously, treatment with Fem 7 Combi can also be started at any time.
- In women using other hormone replacement therapy products continuously and sequentially, the change to Fem 7 Combi should be made after completing the current treatment cycle.
Method of administration:
The instructions for handling are illustrated by the following figures.
The transdermal system consists of a thin, transparent film in the shape of an octagon connected to a two-part, rectangular, stronger protective film.
The octagonal part of the system is the actual, active patch. The inner adhesive surface contains hormones that are released into the skin.
Each transdermal system of Fem 7 Combi is packaged in a separate, tightly closed sachet.
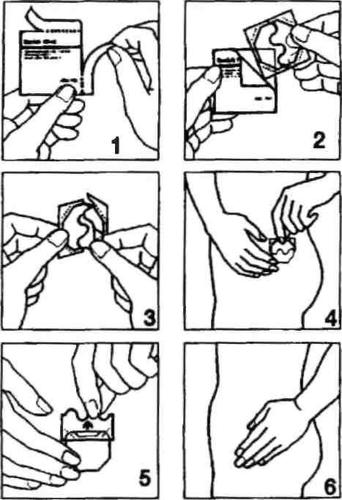
- Open one of the sachets along the side notches (do not use scissors), and then remove the patch. (Fig. 1 and 2).
- The patch should be applied to the skin immediately after removal from the packaging.
- Remove half of the two-part protective film. Do not touch the adhesive part of the patch with your fingers. Apply the adhesive part of the patch to the skin. (Fig. 3 and 4).
- Remove the second half of the protective film. Press the patch with your hand and hold for 30 seconds. The patch will warm up to body temperature, ensuring its optimal adhesion to the skin. (Fig. 5 and 6). Make sure the entire patch adheres to the skin, especially at the edges.
- The patch application site should be changed each time, i.e., a new patch can be applied to the same site after two weeks.
- The skin at the selected site should be healthy, degreased, dry, and undamaged.
- The best places to apply the patch are the hips, upper buttocks, and lower abdomen, as the skin is relatively smooth in these areas. Fem 7 Combi patches should not be applied to the breasts and their immediate vicinity! Do not apply the patch to the waist!
- The patch adheres well to the skin. Bathing in the bathtub, showering, and exercising should not affect the patch's action.
- Avoid rubbing the patch with a sponge or towel, as this may cause the patch to come off.
- Do not wear tight clothing that may cause the patch to come off.
- The patch should be removed slowly to avoid irritating the skin.
- If the patch comes off completely before 7 days, simply apply a new patch.
- Each patch should be used for 7 days. It is recommended to change the patches during treatment always on the same day of the week.
- The next patch should be applied according to the original treatment plan.
- Avoid exposing the patch to direct sunlight.
- If some adhesive remains on the skin after removing the patch, it can be gently wiped off with a cream or cosmetic milk.
How long can Fem 7 Combi be used
Each transdermal system should be used for 7 days.
HRT should be continued for as long as the benefits of relieving menopausal symptoms outweigh the risks associated with HRT use.
Using more than the recommended dose of Fem 7 Combi
Due to the route of administration, overdose of Fem 7 Combi is unlikely.
The symptoms of overdose are breast tenderness, swelling in the abdominal/pelvic area, feeling of anxiety, agitation, nausea, and vomiting. In case of symptoms of overdose, the system should be removed.
Missing a dose of Fem 7 Combi
If a patch change is missed after 7 days, it should be replaced immediately, and the next patch change should be performed on the scheduled day, at the usual time.
Do not use a double dose to make up for a missed patch.
Stopping treatment with Fem 7 Combi
The following symptoms may occur: recurrence of menopausal symptoms.
If the patient wants to stop treatment for some time or permanently, they should first consult their doctor.
4. Possible side effects
Like all medicines, Fem 7 Combi can cause side effects, although not everybody gets them.
The following side effects are possible during hormone replacement therapy in the menopause.
Side effects occur most frequently (> 10%) at the site of application of the transdermal system.
These are: redness of the skin (erythema), irritation, and swelling of the skin, itching. They usually resolve without special treatment within 2-3 days after removing the patch.
Common side effects (which may occur more frequently than in 1 in 100 patients, but less frequently than in 1 in 10 patients):
- increased libido,
- decreased libido,
- headaches,
- nausea,
- vomiting,
- intermenstrual bleeding and spotting.
Uncommon side effects (which may occur more frequently than in 1 in 1,000 patients, but less frequently than in 1 in 100 patients):
- dizziness,
- migraine,
- paresthesia,
- bloating,
- abdominal pain,
- indigestion,
- hypertension,
- painful menstruation,
- endometrial hyperplasia,
- breast cancer,
- fluid retention,
- weight gain,
- weight loss,
- fatigue
Rare side effects (which may occur more frequently than in 1 in 10,000 patients, but less frequently than in 1 in 1,000 patients):
- depression,
- gallstones,
- cholestatic jaundice,
- uterine fibroids.
Other side effects
- estrogen-dependent benign and malignant tumors, e.g., endometrial cancer;
- venous thromboembolic disease, e.g., deep vein thrombosis of the legs or pelvic thrombosis and pulmonary embolism. These occur more frequently in women using HRT than in those not using HRT (see the section "When not to use Fem 7 Combi" and "When to exercise caution when using Fem 7 Combi");
- myocardial infarction and stroke;
- gallbladder disease (e.g., gallstones);
- skin and subcutaneous tissue disorders: chloasma (brown spots on the face), erythema multiforme, nodular erythema, Schönlein-Henoch purpura (hemorrhagic purpura);
- possible dementia (dementia).
Reporting side effects
If you experience any side effects, including any not listed in this leaflet, please tell your doctor or pharmacist. Side effects can be reported directly to the
Department for Monitoring of Adverse Reactions to Medicinal Products, Medical Devices, and Biocidal Products
Al. Jerozolimskie 181C
02-222 Warsaw
Phone: +48 22 49 21 301
Fax: +48 22 49 21 309
Website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Fem 7 Combi
- Keep out of the sight and reach of children.
- Store in a temperature below 30°C.
- Do not use this medicine after the expiry date which is stated on the carton after “Expiry date”. The expiry date refers to the last day of that month.
- Used systems should be folded with the adhesive surface inward and then discarded.
- Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help protect the environment.
6. Contents of the pack and other information
What Fem 7 Combi contains
Active substances:
Transdermal system of phase I:
estradiol (Estradiolum) hemihydrate 1.5 mg
After application to the skin, 50 micrograms of estradiol are released from the transdermal system per day for 7 days. The active surface area of the transdermal system is 15 cm².
Transdermal system of phase II:
estradiol (Estradiolum) hemihydrate 1.5 mg
levonorgestrel (Levonorgestrelum) 1.5 mg
After application to the skin, 50 micrograms of estradiol and 10 micrograms of levonorgestrel are released from the transdermal system per day for 7 days. The active surface area of the transdermal system is 15 cm².
Other ingredients of the medicine are:
Adhesive layer: styrene-isoprene copolymer, glycerin esters of hydrogenated rosin acids
Outer protective layer: polyethylene terephthalate (PET)
Protective layer (to be removed): polyethylene terephthalate (PET) coated with silicone
What Fem 7 Combi looks like and contents of the pack
Fem 7 Combi is an octagonal, transparent, elastic patch with rounded edges.
Its inner (adhesive) layer is covered with a two-part, rectangular, stronger protective film.
4 transdermal systems - 2 phase I transdermal systems + 2 phase II transdermal systems
12 transdermal systems - 6 phase I transdermal systems + 6 phase II transdermal systems
Marketing authorization holder
Theramex Ireland Limited
3rd Floor, Kilmore House,
Park Lane, Spencer Dock,
Dublin 1
D01 YE64
Ireland
Manufacturer:
LTS Lohmann Therapie-Systeme AG
Lohmannstraße 2
56626 Andernach
Germany
To obtain more detailed information, please contact the local representative of the marketing authorization holder at phone number: 22 307 71 66.
Date of last revision of the leaflet:
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterLTS Lohmann Terapie-Systeme AG
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Fem 7 CombiDosage form: Gel, 0.5 mgActive substance: estradiolManufacturer: Orion CorporationPrescription requiredDosage form: Gel, 1 mgActive substance: estradiolManufacturer: Orion CorporationPrescription requiredDosage form: Gel, 1 mg/gActive substance: estradiolPrescription required
Alternatives to Fem 7 Combi in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Fem 7 Combi in Spain
Alternative to Fem 7 Combi in Ukraine
Online doctors for Fem 7 Combi
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Fem 7 Combi – subject to medical assessment and local rules.










