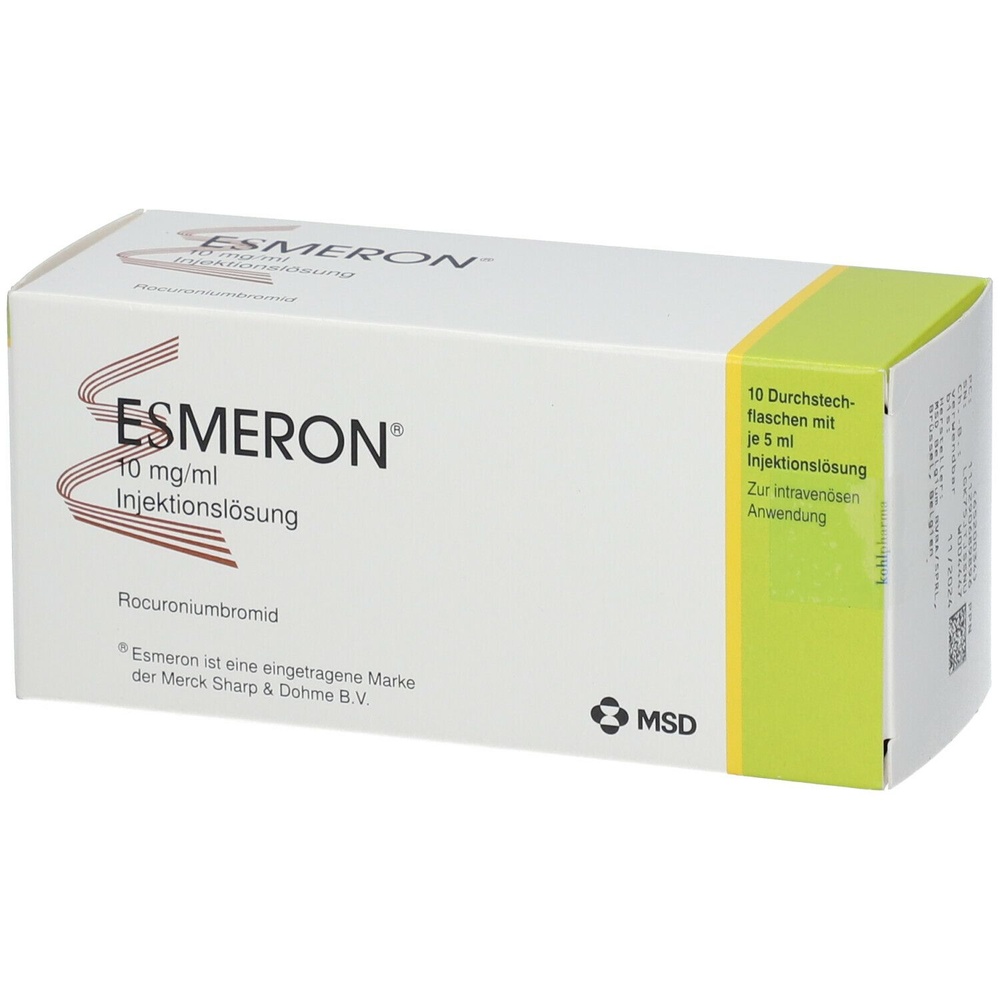
Esmeron
Ask a doctor about a prescription for Esmeron

How to use Esmeron
Package Leaflet: Information for the User
Esmeron, 50 mg/5 ml, solution for injection
Esmeron, 100 mg/10 ml, solution for injection
Rocuronium bromide
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- You should keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack and other information
- 1. What Esmeron is and what it is used for
- 2. Before you use Esmeron
- 3. How to use Esmeron
- 4. Possible side effects
- 5. How to store Esmeron
- 6. Contents of the pack and other information
1. What Esmeron is and what it is used for
Esmeron is one of a group of medicines called muscle relaxants. Muscle relaxants are used during surgery, as part of the general anaesthetic.
Esmeron is used in adult patients as an adjunct to general anaesthesia to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery. Esmeron is also indicated for use in intensive care medicine to facilitate intubation and mechanical ventilation.
Children and adolescents: Esmeron is used as an adjunct to general anaesthesia to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery in full-term newborns, infants and children (from birth to 17 years).
2. Before you use Esmeron
When not to use Esmeron
If you are allergic to rocuronium or any of the other ingredients of this medicine.
Warnings and precautions
Your health status may be important for the choice of the way Esmeron is given to you. You should tell your anaesthetist if you have ever had:
- allergic reactions to muscle relaxants
- kidney problems or kidney disease
- heart problems
- swelling (e.g. swelling of the ankles)
- liver or bile duct problems or liver function disorders
- nerve or muscle disease
- a history of malignant hyperthermia (a sudden rise in body temperature, rapid heart rate, rapid breathing and stiffness, pain and/or muscle weakness)
Certain medical conditions may affect the way Esmeron works, such as:
- low potassium levels in the blood
- high magnesium levels in the blood
- low calcium levels in the blood
- low protein levels in the blood
- dehydration
- acidosis
- high carbon dioxide levels in the blood (hypercapnia)
- poor general health
- obesity
- burns
If any of these conditions apply to you, your doctor will decide on the dose of Esmeron individually for you.
Children and elderly people
Esmeron can be used in the paediatric population (both full-term newborns, infants and children and adolescents) and elderly people, but the doctor should first assess your health status.
Esmeron and other medicines
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
The following medicines may affect the way Esmeron works:
- certain anaesthetics used during surgery
- corticosteroids (anti-inflammatory medicines) used for a long time and Esmeron in intensive care medicine
- certain antibiotics used for bacterial infections
- certain medicines used for bipolar disorder (e.g. lithium salts)
- certain medicines used for cardiovascular disease (quinidine, calcium channel blockers) or medicines that increase blood pressure
- certain medicines used for malaria (e.g. quinine)
- diuretics
- magnesium salts
- local anaesthetics (e.g. lidocaine, bupivacaine)
- antiepileptic medicines used during surgery (e.g. phenytoin)
Esmeron may affect the way other medicines work:
- increases the effect of local anaesthetics (e.g. lidocaine)
Children and adolescents
No formal drug interaction studies have been performed. In children and adolescents, the interactions described above should be taken into account.
Pregnancy and breast-feeding
Before taking any medicine, you should consult your doctor or pharmacist.
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
You should not breast-feed for 6 hours after taking this medicine.
Driving and using machines
This medicine may affect your ability to drive or use machines.
Your doctor will tell you whether it is safe for you to drive or use machines after taking Esmeron.
Esmeron contains sodium
This medicine contains less than 1 mmol (23 mg) of sodium per vial, which is essentially sodium-free.
3. How to use Esmeron
Dose
Your doctor will decide on the dose of Esmeron. Esmeron will be given to you before and/or during surgery.
The usual dose is 0.6 mg/kg body weight of rocuronium bromide, which lasts for 30 to 40 minutes.
During surgery, the effect of Esmeron will be monitored.
If necessary, a further dose of Esmeron may be given.
Method and route of administration
Esmeron is not intended for self-administration by the patient.
Esmeron is given as an intravenous injection or continuous infusion.
Only a doctor or nurse is allowed to give you Esmeron.
Overdose
It is unlikely that you will be given too much Esmeron, as it will be given to you by a doctor or nurse who will be monitoring your treatment.
If you are given too much Esmeron, artificial respiration will be continued until you can breathe on your own again.
The effect of Esmeron can be shortened by giving a medicine that reverses its effect.
Missed dose
This is not relevant for Esmeron.
4. Possible side effects
Like all medicines, Esmeron can cause side effects, although not everybody gets them.
Uncommon or rare side effects (affecting 0.01% to 1% of people) include:
- increased heart rate (tachycardia)
- decreased blood pressure (hypotension)
- weakening or strengthening of the effect of Esmeron
- pain at the injection site
- prolonged muscle relaxation
Very rare side effects (affecting less than 0.01% of people) include:
- allergic reactions, such as changes in blood pressure or heart rate and shock due to low blood volume
- chest tightness caused by bronchospasm (constriction of the airways)
- skin disorders (e.g. angioedema, redness, rash or blisters)
- muscle weakness or paralysis
- prolonged muscle disorders, usually seen in critically ill patients (steroid myopathy), when Esmeron and corticosteroids are used together in intensive care medicine
Frequency not known (frequency cannot be estimated from the available data):
- severe allergic coronary artery spasm (Kounis syndrome) causing chest pain (angina pectoris) or heart attack (myocardial infarction)
- pupil dilation (mydriasis) or fixed pupils that do not change size in response to light or other stimuli
Children and adolescents
Clinical studies in children and adolescents with rocuronium bromide (up to 1 mg/kg body weight) showed an increased heart rate in 1.4% of patients.
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
Side effects can be reported to the national reporting system listed below.
5. How to store Esmeron
Keep this medicine out of the sight and reach of children.
Esmeron should only be stored in a hospital pharmacy.
Store in a refrigerator (2°C - 8°C).
Esmeron can be stored outside of the refrigerator, at a temperature below 30°C, for a maximum of 3 months.
Esmeron can be taken in and out of the refrigerator at any time during the 3-year shelf-life, but the total time out of the refrigerator should not exceed 3 months.
The storage period should not exceed the expiry date stated on the carton and vial.
Do not use this medicine after the expiry date which is stated on the carton and vial after “EXP”.
Do not use this medicine if you notice any particles or if the solution is not clear.
6. Contents of the pack and other information
What Esmeron contains
- The active substance is rocuronium bromide.
- The other ingredients are sodium acetate, sodium chloride, glacial acetic acid to pH 4 and water for injections. 1 ml solution contains 1.64 mg of sodium. The medicine does not contain any preservatives.
What Esmeron looks like and contents of the pack
Esmeron is a colourless to light brown solution for injection or continuous infusion containing 10 mg/ml of rocuronium bromide.
The following pack sizes are available:
- Vials containing 50 mg of rocuronium bromide in 5 ml solution (10 vials in a pack)
- Vials containing 100 mg of rocuronium bromide in 10 ml solution (10 vials in a pack)
Marketing Authorisation Holder and Manufacturer
Marketing Authorisation Holder
MSD Polska Sp. z o.o.
ul. Chłodna 51
00-867 Warszawa
Tel. (+48) 22 54 95 100
Manufacturer
N.V. Organon, Kloosterstraat 6, 5349 AB, Oss, Netherlands
Merck Sharp & Dohme B.V., Waarderweg 39, 2031 BN Haarlem, Netherlands
Date of last revision of the leaflet: 07/2023
Information intended for healthcare professionals only:
For intravenous use only.
As with other neuromuscular blocking agents, Esmeron should only be administered by, or under the supervision of, experienced clinicians who are familiar with the use of these agents and who are aware of their actions and the signs of their effects.
The dosage of Esmeron should be individualised for each patient.
During the administration of Esmeron, it is recommended that the patient’s vital signs and neuromuscular transmission be continuously monitored.
Inhalational anaesthetics potentiate the neuromuscular blocking effect of rocuronium bromide.
This potentiation becomes clinically significant with longer durations of anaesthesia, when the concentration of the inhalational agent in the tissues is sufficient to produce this effect.
Therefore, during long-term anaesthesia (longer than 1 hour) with inhalational agents, the dosage of Esmeron should be modified, either by administering smaller maintenance doses or by reducing the rate of infusion.
The recommended dose of Esmeron is intended as a guideline and may need to be adjusted according to the patient’s response.
Surgery
Intubation
The standard dose for intubation during routine anaesthesia is 0.6 mg/kg body weight of rocuronium bromide.
Suitable conditions for intubation are usually achieved within 60 seconds in the majority of patients.
During rapid sequence induction of anaesthesia, a dose of 1.0 mg/kg body weight of rocuronium bromide is recommended, which provides suitable conditions for intubation within 60 seconds in nearly all patients.
When using a dose of 0.6 mg/kg body weight of rocuronium bromide during rapid sequence induction of anaesthesia, it is recommended to intubate the patient after 90 seconds.
A reference to the use of rocuronium bromide during rapid sequence induction of anaesthesia in caesarean section is provided in section 4.6.
Higher doses
In the event that higher doses are required in individual patients, initial doses of up to 2 mg/kg body weight of rocuronium bromide have been administered during surgery without causing cardiovascular side effects.
The use of higher doses of rocuronium bromide accelerates the onset of effect and prolongs the clinically effective duration of action (see section 5.1).
Maintenance doses
The recommended maintenance dose is 0.15 mg/kg body weight of rocuronium bromide.
During long-term anaesthesia with inhalational agents, the dose should be reduced to 0.075-0.1 mg/kg body weight of rocuronium bromide.
Maintenance doses should be administered when the twitch response returns to 25% of control value or when one or two responses to a train-of-four stimuli are present.
Continuous infusion
If rocuronium bromide is administered by continuous infusion, it is recommended that an initial dose of 0.6 mg/kg body weight of rocuronium bromide be administered, and when the twitch response returns to 10% of control value or one or two responses to a train-of-four stimuli are present, the infusion should be started.
The infusion rate should always be adjusted to the individual needs of the patient.
In adults, during intravenous anaesthesia, the infusion rate required to maintain a twitch response of 10% of control value or one or two responses to a train-of-four stimuli is 0.3-0.6 mg/kg body weight/hour.
In patients anaesthetised with inhalational agents, the infusion rate is 0.3-0.4 mg/kg body weight/hour.
It is recommended that neuromuscular transmission be continuously monitored because of the wide interindividual variability and the influence of the anaesthetic technique.
Children and adolescents
In full-term newborns, infants, children and adolescents (from birth to 17 years), the recommended intubating dose and the recommended maintenance dose are similar to those in adults.
However, the duration of action of a single intubating dose is longer in newborns and infants than in children (see section 5.1).
The infusion rate in adolescents is similar to that in adults, while in children (2-11 years), higher infusion rates may be required.
In children (2-11 years), it is recommended to start with the same infusion rate as in adults and adjust according to the individual response of the patient during surgery to maintain a twitch response of 10% of control value or one or two responses to a train-of-four stimuli.
Experience with the use of rocuronium bromide in rapid sequence induction of anaesthesia in children and adolescents is limited.
Therefore, the use of rocuronium bromide for facilitating endotracheal intubation during rapid sequence induction of anaesthesia in children and adolescents is not recommended.
Dosage in elderly patients, patients with hepatic or biliary disorders and/or renal impairment
The standard dose for intubation in elderly patients and patients with hepatic or biliary disorders and/or renal impairment is 0.6 mg/kg body weight of rocuronium bromide.
During rapid sequence induction of anaesthesia in patients who may be expected to have a prolonged effect of the medicine, a dose of 0.6 mg/kg body weight of rocuronium bromide should be considered.
Regardless of the anaesthetic technique used, the recommended maintenance dose in these patients is 0.075-0.1 mg/kg body weight of rocuronium bromide, and the recommended infusion rate is 0.3-0.4 mg/kg body weight/hour (see “Continuous infusion”) (see also section 4.4).
Dosage in obese patients
In obese patients (defined as a body weight 30% or more above ideal body weight), the dose of Esmeron should be reduced, taking into account the ideal body weight.
Intensive Care Unit (ICU) procedures
Intubation
The same doses as described above for surgery should be used for intubation.
Dosage for mechanical ventilation
A dose of 0.6 mg/kg body weight of rocuronium bromide is recommended.
When the twitch response returns to 10% of control value or one or two responses to a train-of-four stimuli are present, the infusion should be started.
The dosage should always be adjusted to the individual needs of the patient.
The recommended initial infusion rate to maintain a twitch response of 80-90% (one or two responses to a train-of-four stimuli) in adult patients is 0.3-0.6 mg/kg body weight/hour in the first hour of administration.
During the next 6-12 hours, the infusion rate should be reduced according to the individual needs of the patient.
Later, the individual needs remain relatively constant.
In controlled clinical studies, a significant interindividual variability in infusion rates was observed, with average hourly infusion rates ranging from 0.2 to 0.5 mg/kg body weight/hour, depending on the type and degree of organ system impairment, concomitant medications and individual patient characteristics.
To achieve optimal control of the patient, it is recommended that neuromuscular transmission be monitored.
Administration of the medicine for up to 7 days has been studied.
Special patient populations
The use of Esmeron for facilitating mechanical ventilation in ICU is not recommended in children and adolescents and elderly patients with renal impairment due to lack of data on efficacy and safety.
Method of administration
Esmeron should be administered intravenously as a rapid injection or continuous infusion (see section 6.6).
- Country of registration
- Active substance
- Prescription requiredNo
- Manufacturer
- ImporterMerck Sharp & Dohme B.V. N.V. Organon Organon (Ireland) Ltd.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to EsmeronDosage form: Solution, 100 mg/10 mlActive substance: rocuronium bromideManufacturer: Merck Sharp & Dohme B.V. N.V. OrganonPrescription not requiredDosage form: Solution, 10 mg/mlActive substance: rocuronium bromidePrescription not requiredDosage form: Solution, 10 mg/mlActive substance: rocuronium bromideManufacturer: B. Braun Melsungen AGPrescription required
Alternatives to Esmeron in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Esmeron in Spain
Alternative to Esmeron in Ukraine
Online doctors for Esmeron
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Esmeron – subject to medical assessment and local rules.