

Crusia

Ask a doctor about a prescription for Crusia

How to use Crusia
Leaflet accompanying the packaging: patient information
Crusia, 2000 IU (20 mg)/0.2 ml, solution for injection in a pre-filled syringe
Crusia, 4000 IU (40 mg)/0.4 ml, solution for injection in a pre-filled syringe
Crusia, 6000 IU (60 mg)/0.6 ml, solution for injection in a pre-filled syringe
Crusia, 8000 IU (80 mg)/0.8 ml, solution for injection in a pre-filled syringe
Crusia, 10,000 IU (100 mg)/1 ml, solution for injection in a pre-filled syringe
This medicinal product is subject to additional monitoring. This will allow for quick identification of new safety information. You can help by reporting any side effects you may get. To learn how to report side effects, see section 4.
Enoxaparin sodium
You should carefully read the contents of this leaflet before using the medicine, as it contains important information for the patient.
- You should keep this leaflet, so you can read it again if you need to.
- If you have any further questions, you should ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed specifically for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If you experience any side effects, including those not listed in this leaflet, you should tell your doctor or pharmacist. See section 4.
Table of contents of the leaflet
- 1. What is Crusia and what is it used for
- 2. Important information before using Crusia
- 3. How to use Crusia
- 4. Possible side effects
- 5. How to store Crusia
- 6. Contents of the packaging and other information
1. What is Crusia and what is it used for
Crusia contains the active substance enoxaparin sodium, which is a low molecular weight heparin (LMWH).
Crusia works in two ways.
- 1) It prevents the growth of existing blood clots. This helps the body to dissolve existing blood clots, so they are no longer harmful.
- 2) It prevents the formation of new blood clots in the patient's blood.
Crusia can be used for:
- Treating blood clots that are already present in the patient's blood.
- Preventing the formation of blood clots in the patient's blood in the following situations: before and after surgery, during acute illness when the patient has limited mobility, if the patient has had blood clots caused by cancer, to prevent further blood clots, in unstable angina (a condition where the heart does not receive enough blood), after a heart attack
- Preventing the formation of clots in the dialyzer tubes (used in people with severe kidney problems)
in patients with severe kidney problems.
2. Important information before using Crusia
When not to use Crusia
- If you are allergic to enoxaparin sodium or any of the other ingredients of this medicine (listed in section 6). Symptoms of an allergic reaction may include: rash, difficulty swallowing or breathing, swelling of the face, lips, throat, or tongue.
- If you have been diagnosed with an allergy to heparin or other low molecular weight heparins, such as nadroparin, tinzaparin, or dalteparin.
- If you have been diagnosed with a reaction to heparin that has caused a significant decrease in the number of blood cells responsible for blood clotting (platelets) - a reaction known as heparin-induced thrombocytopenia - in the last 100 days or if you have antibodies against enoxaparin in your blood.
- If you have active bleeding or a medical condition that increases the risk of bleeding (such as stomach ulcers, recent brain or eye surgery), including recent hemorrhagic stroke.
- If you are using Crusia to treat blood clots and spinal or epidural anesthesia is planned.
Warnings and precautions
Crusia should not be used interchangeably with other low molecular weight heparins. This is because they are not identical and differ in activity and instructions for use.
Before starting treatment with Crusia, you should discuss this with your doctor or pharmacist if:
- you have ever had a reaction to heparin that has caused a significant decrease in the number of platelets in your blood
- you are scheduled to have spinal or epidural anesthesia (see "Surgical procedures and anesthetics")
- you have a heart valve replacement
- you have endocarditis (an infection of the membrane that lines the heart)
- you have had stomach ulcers
- you have recently had a stroke
- you have high blood pressure
- you have diabetes or have problems with the blood vessels in your eyes caused by diabetes (diabetic retinopathy)
- you have recently had eye or brain surgery
- you are elderly (over 65 years old), especially if you are over 75 years old
- you have kidney problems
- you have liver problems
- you are underweight or overweight
- you have high levels of potassium in your blood (which can be checked with a blood test)
- you are currently taking medications that may cause bleeding (see "Crusia and other medicines")
Before and periodically during treatment with this medicine, you may have blood tests to check the number of platelets in your blood and the level of potassium in your blood.
Children and adolescents:
The safety and efficacy of enoxaparin have not been evaluated in children and adolescents.
Crusia and other medicines
You should tell your doctor or pharmacist about all the medicines you are taking, have recently taken, or plan to take.
- Warfarin - a medicine used to thin the blood
- Aspirin (also known as acetylsalicylic acid or ASA), clopidogrel, or other medicines used to prevent blood clots (see also section 3 "Change of anticoagulant medicine")
- Dextrans - used as a blood substitute
- Ibuprofen, diclofenac, ketorolac, or other non-steroidal anti-inflammatory medicines used to treat pain and swelling in arthritis and other conditions
- Prednisolone, dexamethasone, or other medicines used to treat asthma, rheumatoid arthritis, and other conditions
- Medicines that increase potassium levels in the blood, such as potassium salts, diuretics, and certain heart medicines.
Surgical procedures and anesthetics
If you are scheduled to have a lumbar puncture or surgery under epidural or spinal anesthesia, you should inform your doctor that you are taking Crusia. See "When not to use Crusia". Additionally, you should inform your doctor if you have any spinal problems or if you have had spinal surgery.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant, or plan to have a baby, you should ask your doctor or pharmacist for advice before taking this medicine.
Women with pregnancy and mechanical heart valve may have an increased risk of blood clots. Your doctor should discuss this with you.
Women who are breastfeeding or plan to breastfeed should ask their doctor for advice before taking this medicine.
Driving and using machines
Crusia does not affect the ability to drive or use machines.
It is recommended that your doctor documents the trade name and batch number of the product used.
Crusia contains sodium
This medicine contains less than 1 mmol (23 mg) of sodium per dose, which means it is essentially "sodium-free".
3. How to use Crusia
This medicine should always be used exactly as your doctor or pharmacist has told you. If you are not sure, you should ask your doctor or pharmacist.
Administration of the medicine
- Crusia is usually given to you by a doctor or nurse. This is because it needs to be given by injection.
- After you return home, you may need to continue using Crusia and give it to yourself (see the instructions for administration below).
- Crusia is usually given by subcutaneous injection.
- Crusia may be given by intravenous injection after certain types of heart attack or after surgery.
- Crusia may be introduced into the dialysis tube returning blood from the body (into the arterial line) at the start of the dialysis session. Crusia must not be given by intramuscular injection.
Dose
- Your doctor will decide what dose of Crusia you should have. This will depend on the reason for using the medicine.
- In patients with kidney problems, you may be given a lower dose of Crusia.
- 1. Treatment of blood clots in the patient's blood
- The usual dose is 150 IU (1.5 mg) per kilogram of body weight once daily or 100 IU (1 mg) per kilogram of body weight twice daily.
- Your doctor will decide how long you should receive Crusia.
- 2. Prevention of blood clots in the patient's blood in the following situations:
- Surgery or limited mobility due to illness
- The dose depends on the patient's risk of developing a blood clot. You will receive Crusia at a dose of 2000 IU (20 mg) or 4000 IU (40 mg) per day.
- For planned surgery, the first injection is usually given 2 hours or 12 hours before surgery.
- If you have limited mobility due to illness, you will usually receive Crusia at a dose of 4000 IU (40 mg) per day.
- Your doctor will decide how long you should receive Crusia.
- After a heart attackCrusia can be used in two different types of heart attack: heart attack with ST-segment elevation (STEMI) and heart attack without ST-segment elevation (NSTEMI). The dose of Crusia will depend on your age and the type of heart attack you have had.
Non-ST-segment elevation heart attack (NSTEMI):
- The usual dose is 100 IU (1 mg) per kilogram of body weight every 12 hours.
- Your doctor will usually recommend that you also take aspirin (acetylsalicylic acid).
- Your doctor will decide how long you should receive Crusia.
ST-segment elevation heart attack (STEMI) in patients under 75 years of age:
- The initial dose of Crusia is 3000 IU (30 mg) given as an intravenous injection.
- Crusia is also given by subcutaneous injection. The usual dose is 100 IU (1 mg) per kilogram of body weight every 12 hours.
- Your doctor will usually recommend that you also take aspirin (acetylsalicylic acid).
- Your doctor will decide how long you should receive Crusia.
ST-segment elevation heart attack (STEMI) in patients 75 years of age or older:
- The usual dose is 75 IU (0.75 mg) per kilogram of body weight every 12 hours.
The maximum dose of Crusia in the first two doses is 7500 IU (75 mg).
- Your doctor will decide how long you should receive Crusia.
Patient undergoing percutaneous coronary intervention (PCI):
Depending on when the last dose of Crusia was given, your doctor may decide to give an additional dose of Crusia before the PCI procedure.
This will be given as an intravenous injection.
- 3. Prevention of blood clots in the dialyzer tubes
- The usual dose is 100 IU (1 mg) per kilogram of body weight.
- Crusia is injected into the tube returning blood from the body (into the arterial line) at the start of the dialysis session. This dose is usually sufficient for a 4-hour dialysis session. However, your doctor may give you an additional dose of 50 IU to 100 IU (0.5 to 1 mg) per kilogram of body weight if necessary.
Instructions for using the pre-filled syringe
Self-administration of Crusia
If you are able to give yourself Crusia, your doctor or nurse will show you how to do it. Do not attempt to give yourself an injection until you have been instructed.
If you are unsure about what to do, you should talk to your doctor or nurse immediately. Proper injection technique will help to reduce pain and bruising at the injection site.
Before self-administration of Crusia
- Gather the necessary items: syringe, cotton ball or soap and water, and a container for sharp objects.
- Check the expiration date on the packaging. Do not use the medicine after the expiration date.
- Check that the syringe is not damaged and that the liquid is clear. If it is not, use another syringe.
- Make sure you know what dose you are supposed to inject.
- Look at your stomach to check if the last injection has caused redness, discoloration, swelling, discharge, or if it is still painful. If it is, you should talk to your doctor or nurse.
Instructions for self-administration of Crusia:
(Instructions for pre-filled syringes without a safety device)
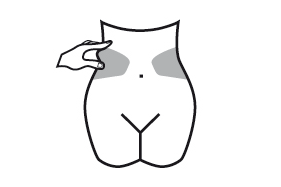
Preparing the injection site
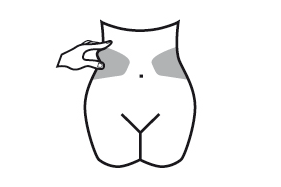
- 1) Choose an injection site on the right or left side of your stomach. The injection site should be at least 5 cm away from your belly button.
- Do not inject within 5 cm of your belly button or around existing scars or bruises.
- Alternate injection sites between the left and right sides of your stomach, depending on the site of the previous injection.
- 2) Wash your hands. Clean (do not rub) the injection site with a cotton ball soaked in alcohol or soap and water.
- 3) Sit or lie down in a comfortable position, so you are relaxed. Make sure the injection site is within your sight. A chair, couch, or bed with pillows for support will be suitable.
Choosing the dose
- 1) Carefully remove the needle cap from the syringe. Discard the cap.
- Do not press the plunger before injecting to remove air bubbles. This may reduce the dose administered.
- After removing the cap, do not touch the needle. This will ensure the sterility of the needle.
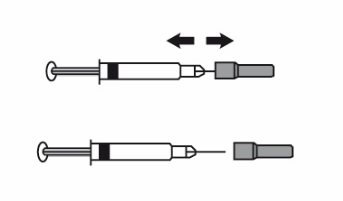
- 2) If the amount of medicine in the syringe is the same as the prescribed dose, there is no need to adjust the dose. You can now give the injection.
- 3) If the dose depends on your body weight, you may need to adjust the dose in the syringe according to the prescribed dose. In this case, you should remove any excess medicine by holding the syringe with the needle facing down (to keep air bubbles in the syringe) and expelling the excess medicine into a container.
- 4) A drop may appear at the tip of the needle. If it does, you should remove the drop before injecting by tapping the syringe with the needle facing down. You can now give the injection.
Injecting the medicine
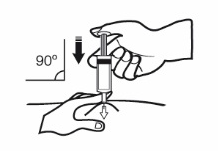
- 1) Hold the syringe in the hand you write with (like a pen). With your other hand, gently grasp the cleaned skin of your stomach between your thumb and index finger, creating a fold in the skin.
- Make sure you maintain the skin fold while giving the injection.
- 2) Hold the syringe with the needle facing down (at a 90-degree angle). Insert the entire length of the needle into the skin fold.
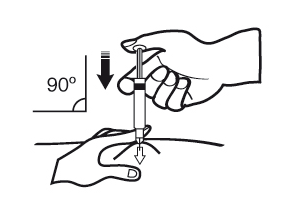
- 3) Press the plunger with your thumb. This will inject the medicine into the fatty tissue of your stomach. You should inject the entire amount of medicine in the syringe.
- 4) Remove the needle from the injection site, pulling it out straight. Hold the needle away from yourself and others. You can now release the skin fold.
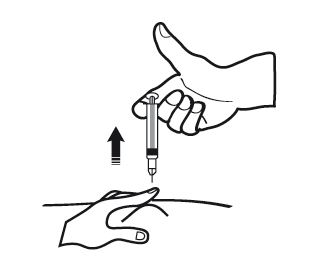
After the injection
- 1) To avoid bruising, do not rub the injection site after the injection.
- 2) Dispose of the used syringe in a container for sharp objects. Close the container and keep it out of sight and reach of children. If the container is full, dispose of it according to the instructions of your doctor or pharmacist.
Any unused medicine or waste materials should be disposed of in accordance with local regulations.
If you feel that the dose is too strong (for example, you experience unexpected bleeding) or too weak (for example, the dose probably does not work), you should consult your doctor or pharmacist.
Instructions for pre-filled syringes with a safety device:
Preparing the injection site
- 1) Choose an injection site on the right or left side of your stomach. The injection site should be at least 5 cm away from your belly button.
- Do not inject within 5 cm of your belly button or around existing scars or bruises.
- Alternate injection sites between the left and right sides of your stomach, depending on the site of the previous injection.
- 2) Wash your hands. Clean (do not rub) the injection site with a cotton ball soaked in alcohol or soap and water.
- 3) Sit or lie down in a comfortable position, so you are relaxed. Make sure the injection site is within your sight. A chair, couch, or bed with pillows for support will be suitable.
Choosing the dose
- 1) Carefully remove the needle cap from the syringe. Discard the cap.
- Do not press the plunger before injecting to remove air bubbles. This may reduce the dose administered.
- After removing the cap, do not touch the needle. This will ensure the sterility of the needle.
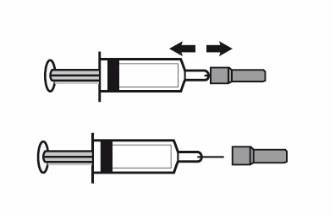
- 2) If the amount of medicine in the syringe is the same as the prescribed dose, there is no need to adjust the dose. You can now give the injection.
- 3) If the dose depends on your body weight, you may need to adjust the dose in the syringe according to the prescribed dose. In this case, you should remove any excess medicine by holding the syringe with the needle facing down (to keep air bubbles in the syringe) and expelling the excess medicine into a container.
- 4) A drop may appear at the tip of the needle. If it does, you should remove the drop before injecting by tapping the syringe with the needle facing down. You can now give the injection.
Injecting the medicine
- 1) Hold the syringe in the hand you write with (like a pen). With your other hand, gently grasp the cleaned skin of your stomach between your thumb and index finger, creating a fold in the skin.
- Make sure you maintain the skin fold while giving the injection.
- 2) Hold the syringe with the needle facing down (at a 90-degree angle). Insert the entire length of the needle into the skin fold.
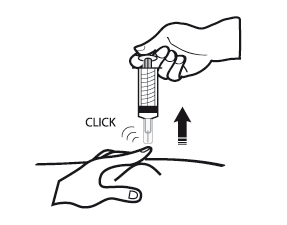
- 3) Press the plunger with your thumb. This will inject the medicine into the fatty tissue of your stomach. You should inject the entire amount of medicine in the syringe.
- 4) Remove the needle from the injection site, pulling it out straight, while still holding the plunger. Hold the needle away from yourself and others. The safety device is activated by firmly pressing the plunger. The protective shield will automatically cover the needle and a clicking sound will be heard, confirming the activation of the protective shield. You can now release the skin fold.
After the injection
- 1) To avoid bruising, do not rub the injection site after the injection.
- 2) Dispose of the used syringe in a container for sharp objects. Close the container and keep it out of sight and reach of children. If the container is full, dispose of it according to the instructions of your doctor or pharmacist.
Any unused medicine or waste materials should be disposed of in accordance with local regulations.
If you feel that the dose is too strong (for example, you experience unexpected bleeding) or too weak (for example, the dose probably does not work), you should consult your doctor or pharmacist.
Change of anticoagulant medicine
- Change from Crusia to medicines that thin the blood, known as vitamin K antagonists (e.g. warfarin)Your doctor will advise you to have blood tests to measure your INR (International Normalized Ratio) and will tell you when to stop taking Crusia based on the results.
- Change from vitamin K antagonists (e.g. warfarin) to CrusiaYou should stop taking the vitamin K antagonist. Your doctor will advise you to have blood tests to measure your INR and will tell you when to start taking Crusia based on the results.
- Change from Crusia to direct oral anticoagulantsYou should stop taking Crusia. Then, you should start taking the direct oral anticoagulant 0-2 hours before the planned time of the next Crusia injection; and then you should continue taking the medicine as usual.
- Change from direct oral anticoagulant to CrusiaYou should stop taking the direct oral anticoagulant. Treatment with Crusia can be started 12 hours after the last dose of the direct oral anticoagulant.
Use of a higher than recommended dose of Crusia
If you think you have used too much or too little Crusia, you should immediately inform your doctor, nurse, or pharmacist, even if you do not notice any problems. If a child accidentally injects or swallows Crusia, you should immediately go to the hospital emergency department.
Missing a dose of Crusia
If you miss a dose, you should take it as soon as possible. Do not take a double dose to make up for a missed dose. Keeping a diary can help you make sure you do not miss a dose.
Stopping treatment with Crusia
If you have any further questions about using this medicine, you should ask your doctor, pharmacist, or nurse.
It is important to continue giving yourself injections of Crusia until your doctor tells you to stop. If you stop treatment, you may develop a blood clot, which can be very dangerous.
4. Possible side effects
Like all medicines, Crusia can cause side effects, although not everybody gets them.
As with other similar medicines (used to reduce blood clotting), Crusia can cause bleeding, which can be life-threatening. In some cases, bleeding may not be immediately visible.
If you experience any bleeding that does not stop by itself, as well as signs of excessive bleeding (severe weakness, tiredness, paleness, dizziness, headaches, or unexplained sweating), you should immediately consult your doctor. Your doctor may decide to monitor you more closely or change your medicine.
If you experience any of the following symptoms, you should stop using enoxaparin and seek medical help immediately:
- Any symptoms of a severe allergic reaction (such as difficulty breathing, swelling of the lips, mouth, throat, or eyes).
- A red, scaly, widespread rash with thickening of the skin and blisters, accompanied by fever.
You should immediately consult your doctor:
- If you experience any signs of a blood clot blocking a blood vessel, such as:
- cramping pain, redness, increased warmth or swelling in one of your legs - these are symptoms of deep vein thrombosis
- shortness of breath, chest pain, fainting, or coughing up blood - these are symptoms of pulmonary embolism
- If you experience painful bruising or purple spots under the skin that do not fade when pressed. Your doctor may order blood tests to check your platelet count.
List of possible side effects:
Very common (may affect more than 1 in 10 people)
- Bleeding.
- Increased liver enzyme activity.
Common (may affect up to 1 in 10 people)
- Increased tendency to bruise. This may be due to a decrease in the number of platelets in your blood.
- Purple spots on the skin. These changes are more likely to occur at the injection sites of Crusia.
- Hives (itchy rash).
- Itchy, red skin.
- Bruising or pain at the injection site.
- Decreased red blood cell count.
- Increased platelet count.
- Headache.
Uncommon (may affect up to 1 in 100 people)
- Sudden severe headache. This may be a sign of bleeding in the brain.
- Tenderness and swelling of the stomach. This may be a sign of bleeding in the stomach.
- Large, red, irregularly-shaped skin changes with blisters, which may be accompanied by fever.
- Skin irritation (local irritation).
- You may notice yellowing of the skin or eyes and darker urine. This may indicate liver problems.
Rare (may affect up to 1 in 1,000 people)
- Severe allergic reaction. Symptoms of such a reaction may include: rash, difficulty swallowing or breathing, swelling of the lips, face, throat, or tongue.
- High levels of potassium in the blood. This is more likely to occur in people with kidney problems or diabetes. Your doctor may check this with a blood test.
- Increased eosinophil count in the blood. Your doctor may check this with a blood test.
- Hair loss.
- Osteoporosis (a condition where bones are more likely to break) after long-term use of the medicine.
- Numbness, tingling, and muscle weakness (especially in the lower part of the body) after a lumbar puncture or spinal anesthesia.
- Loss of control over urination or bowel movements (a condition where you are unable to control when you go to the toilet).
- Hardening or a lump at the injection site.
Reporting side effects
If you experience any side effects, including those not listed in this leaflet, you should tell your doctor, pharmacist, or nurse. Side effects can be reported directly to the Department of Medicinal Product Monitoring, Urząd Rejestracji Produktów Leczniczych, Wyrobów Medycznych i Produktów Biobójczych, Al. Jerozolimskie 181C, 02-222 Warszawa, tel.: +48 22 49 21 301, fax: +48 22 49 21 309, website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Crusia
Store in a temperature not exceeding 25°C. Do not freeze.
Crusia pre-filled syringes are single-dose containers - any unused medicine should be discarded.
The medicine should be kept out of sight and reach of children.
Do not use this medicine after the expiration date stated on the packaging. The expiration date refers to the last day of the month stated.
Do not use the medicine if the pre-filled syringe is damaged or if the product is not clear.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Contents of the packaging and other information
What Crusia contains
- The active substance is enoxaparin sodium.
Each pre-filled syringe contains enoxaparin sodium equivalent to 2000 IU of anti-Xa activity (which is equivalent to 20 mg) in 0.2 ml of water for injection.
Each pre-filled syringe contains enoxaparin sodium equivalent to 4000 IU of anti-Xa activity (which is equivalent to 40 mg) in 0.4 ml of water for injection.
Each pre-filled syringe contains enoxaparin sodium equivalent to 6000 IU of anti-Xa activity (which is equivalent to 60 mg) in 0.6 ml of water for injection.
Each pre-filled syringe contains enoxaparin sodium equivalent to 8000 IU of anti-Xa activity (which is equivalent to 80 mg) in 0.8 ml of water for injection.
Each pre-filled syringe contains enoxaparin sodium equivalent to 10,000 IU of anti-Xa activity (which is equivalent to 100 mg) in 1.0 ml of water for injection.
- The other ingredient is water for injection.
What Crusia looks like and contents of the pack
Crusia is a clear, colorless to pale yellow solution for injection in a pre-filled syringe made of glass type I, with a rubber stopper, plunger, and needle in a protective shield, with or without an automatic safety device. It is available in the following strengths:
Crusia 2000 IU (20 mg)/0.2 ml solution for injection in a 0.5 ml pre-filled syringe without graduation.
Pack sizes: 2, 6, 10, 20, and 50 pre-filled syringes.
Crusia 4000 IU (40 mg)/0.4 ml solution for injection in a 0.5 ml pre-filled syringe without graduation.
Pack sizes: 2, 6, 10, 20, 30, and 50 pre-filled syringes.
Crusia 6000 IU (60 mg)/0.6 ml solution for injection in a 1 ml pre-filled syringe.
Pack sizes: 2, 6, 10, 12, 24, 30, and 50 pre-filled syringes.
Crusia 8000 IU (80 mg)/0.8 ml solution for injection in a 1 ml pre-filled syringe.
Pack sizes: 2, 6, 10, 12, 24, 30, and 50 pre-filled syringes.
Crusia 10,000 IU (100 mg)/1 ml solution for injection in a 1 ml pre-filled syringe.
Pack sizes: 2, 6, 10, 12, 24, 30, and 50 pre-filled syringes.
Not all pack sizes may be marketed.
Marketing authorization holder and manufacturer:
Marketing authorization holder:
Laboratorios Farmacéuticos Rovi, S.A.
Julián Camarillo, 35
28037 Madrid
Spain
tel.: (+48) 699 711 147
Manufacturer:
ROVI Pharma Industrial Services S.A.
Julián Camarillo, 35
28037 Madrid
Spain
This medicine is authorized in the Member States of the European Economic Area and in the United Kingdom (Northern Ireland) under the following names:
Austria, Denmark, Finland, Netherlands, Germany, Norway, Sweden, United Kingdom (Northern Ireland), Spain, Portugal, Greece, Bulgaria, Czech Republic, Estonia, Croatia, Hungary, Latvia, Poland, Romania, Slovakia: Crusia
France: Enoxaparine Crusia
Italy: Rovinadil
Belgium, Ireland, Slovenia, Luxembourg: Teuro
Date of last revision of the leaflet: 01/2023
Other sources of information
Detailed information on this medicine is available on the website of the Urząd Rejestracji Produktów Leczniczych, Wyrobów Medycznych i Produktów Biobójczych: http://www.urpl.gov.pl/
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterRovi Pharma industrial Services, S.A.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to CrusiaDosage form: Solution, 12,000 IU (120 mg)/0.8 mlActive substance: enoxaparinPrescription requiredDosage form: Solution, 15,000 IU (150 mg)/mlActive substance: enoxaparinPrescription requiredDosage form: Solution, 2000 IU (20 mg)/0.2 mlActive substance: enoxaparin
Alternatives to Crusia in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Crusia in Spain
Alternative to Crusia in Ukraine
Online doctors for Crusia
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Crusia – subject to medical assessment and local rules.














