

Crusia

Ask a doctor about a prescription for Crusia

How to use Crusia
Leaflet accompanying the packaging: patient information
Crusia, 2000 IU (20 mg)/0.2 ml, solution for injection in a pre-filled syringe
Crusia, 4000 IU (40 mg)/0.4 ml, solution for injection in a pre-filled syringe
Crusia, 6000 IU (60 mg)/0.6 ml, solution for injection in a pre-filled syringe
Crusia, 8000 IU (80 mg)/0.8 ml, solution for injection in a pre-filled syringe
Crusia, 10,000 IU (100 mg)/1 ml, solution for injection in a pre-filled syringe
This medicinal product is subject to additional monitoring. This will allow for quick identification of new safety information. You can help by reporting any side effects you may get. To find out how to report side effects, see section 4.
Enoxaparin sodium
You should carefully read the contents of this leaflet before using the medicine, as it contains important information for the patient.
- You should keep this leaflet, so you can read it again if you need to.
- If you have any further questions, you should ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed specifically for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours.
- If you experience any side effects, including those not listed in this leaflet, you should tell your doctor or pharmacist. See section 4.
Table of contents of the leaflet
- 1. What is Crusia and what is it used for
- 2. Important information before using Crusia
- 3. How to use Crusia
- 4. Possible side effects
- 5. How to store Crusia
- 6. Contents of the packaging and other information
1. What is Crusia and what is it used for
Crusia contains the active substance enoxaparin sodium, which is a low molecular weight heparin (LMWH).
Crusia works in two ways.
- 1) It prevents the growth of existing blood clots. This helps the body to dissolve existing blood clots, making them no longer harmful.
- 2) It prevents the formation of new blood clots in the patient's blood.
Crusia can be used for:
- Treating blood clots that are already present in the patient's blood.
- Preventing the formation of blood clots in the patient's blood in the following situations: before and after surgery, during acute illness when the patient has limited mobility, if the patient has had blood clots caused by cancer to prevent further clots, in unstable angina (a condition where the heart does not receive enough blood), after a heart attack
- Preventing the formation of clots in the dialyzer tubes (used in people with severe kidney function disorders)
in patients with severe kidney function disorders.
2. Important information before using Crusia
When not to use Crusia
- If the patient is allergic to enoxaparin sodium or any of the other ingredients of this medicine (listed in section 6). Symptoms of an allergic reaction may include: rash, difficulty swallowing or breathing, swelling of the lips, face, throat, or tongue.
- If the patient has been diagnosed with an allergy to heparin or other low molecular weight heparins, such as nadroparin, tinzaparin, or dalteparin.
- If the patient has been diagnosed with a reaction to heparin that caused a significant decrease in the number of blood cells responsible for blood clotting (platelets) - a reaction known as heparin-induced thrombocytopenia - within the last 100 days or if the patient has antibodies against enoxaparin in their blood.
- If the patient has severe bleeding or a medical condition associated with an increased risk of bleeding (e.g., stomach ulcers, recent brain or eye surgery), including recent hemorrhagic stroke.
- If the patient is using Crusia to treat blood clots and spinal or epidural anesthesia is planned.
Warnings and precautions
Crusia should not be used interchangeably with other low molecular weight heparins. This is because they are not exactly the same, differ in activity, and have different instructions for use.
Before starting to use Crusia, you should discuss this with your doctor or pharmacist if:
- the patient has ever had a reaction to heparin that caused a significant decrease in the number of platelets
- the patient is scheduled for spinal or epidural anesthesia (see "Surgical procedures and anesthetics")
- the patient has a heart valve replacement
- the patient has endocarditis (infection of the membrane lining the heart)
- the patient has had stomach ulcers
- the patient has recently had a stroke
- the patient has high blood pressure
- the patient has diabetes or has problems with blood vessels in the eyes caused by diabetes (diabetic retinopathy)
- the patient has recently had eye or brain surgery
- the patient is elderly (over 65 years), especially if they are over 75 years old
- the patient has kidney disease
- the patient has liver disease
- the patient is underweight or overweight
- the patient has an increased level of potassium in the blood (which can be checked with a blood test)
- the patient is currently taking medications that may cause bleeding (see below "Crusia and other medicines")
Before starting and periodically during the use of this medicine, the patient may undergo a blood test to check the number of platelets and potassium levels in the blood.
Children and adolescents:
The safety and efficacy of enoxaparin have not been evaluated in children and adolescents.
Crusia and other medicines
You should tell your doctor or pharmacist about all the medicines you are taking, have recently taken, or plan to take.
- Warfarin - a medicine used to thin the blood
- Aspirin (also known as acetylsalicylic acid or ASA), clopidogrel, or other medicines used to prevent blood clots (see also section 3 "Change of anticoagulant medicine")
- Dextran injections - used as a blood substitute
- Ibuprofen, diclofenac, ketorolac, or other non-steroidal anti-inflammatory medicines used to treat pain and swelling in arthritis and other conditions
- Prednisolone, dexamethasone, or other medicines used to treat asthma, rheumatoid arthritis, and other conditions
- Medicines that increase potassium levels in the blood, such as potassium salts, diuretics, and certain heart medicines.
Surgical procedures and anesthetics
If the patient is scheduled for a lumbar puncture or surgery under spinal or epidural anesthesia, they should inform their doctor that they are using Crusia. See "When not to use Crusia". Additionally, the patient should inform their doctor if they have any spinal problems or if they have had spinal surgery.
Pregnancy and breastfeeding
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a baby, they should ask their doctor or pharmacist for advice before using this medicine.
Women with pregnancy and mechanical heart valve may have an increased risk of blood clots. The doctor should discuss this with the patient.
Women who are breastfeeding or plan to breastfeed should consult their doctor before using this medicine.
Driving and using machines
Crusia does not affect the ability to drive or use machines.
The doctor should document the trade name and batch number of the product used.
Crusia contains sodium
This medicine contains less than 1 mmol (23 mg) of sodium per dose, which means it is essentially "sodium-free".
3. How to use Crusia
This medicine should always be used exactly as prescribed by your doctor or pharmacist. If you are unsure, you should ask your doctor or pharmacist.
Administration of the medicine
- Crusia is usually administered to the patient by a doctor or nurse. This is because it requires injection.
- After returning home, the patient may need to continue using Crusia and self-administer it (see the administration instructions below).
- Crusia is usually administered subcutaneously.
- Crusia may be administered intravenously after certain types of heart attack or after surgery.
- Crusia may be introduced into the dialyzer tube returning blood from the body (into the so-called arterial line) at the start of the dialysis session. Crusia should not be administered intramuscularly.
Dose
- The doctor will decide what dose of Crusia the patient should take. This depends on the reason for using the medicine.
- In patients with kidney disease, the patient may receive a lower dose of Crusia.
- 1. Treatment of blood clots in the patient's blood
- The usual dose is 150 IU (1.5 mg) per kilogram of body weight once daily or 100 IU (1 mg) per kilogram of body weight twice daily.
- The doctor will decide how long the patient should receive Crusia.
- 2. Prevention of blood clot formation in the patient's blood in the following situations:
- Surgical procedure or period of limited mobility due to illness
- The dose depends on the patient's risk of clotting. The patient will receive Crusia at a dose of 2000 IU (20 mg) or 4000 IU (40 mg) per day.
- In the case of planned surgery, the first injection is usually given 2 hours or 12 hours before the procedure.
- If the patient has limited mobility due to illness, they usually receive Crusia at a dose of 4000 IU (40 mg) per day.
- The doctor will decide how long the patient should receive Crusia.
- After a heart attackCrusia can be used in two different types of heart attack: ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI). The dose of Crusia will depend on the patient's age and the type of heart attack they had.
NSTEMI:
- The usual dose is 100 IU (1 mg) per kilogram of body weight every 12 hours.
- The doctor will usually recommend that the patient also take aspirin (acetylsalicylic acid).
- The doctor will decide how long the patient should receive Crusia.
STEMI in patients under 75 years of age:
- The initial dose of Crusia is 3000 IU (30 mg) given intravenously.
- Crusia is also given subcutaneously. The usual dose is 100 IU (1 mg) per kilogram of body weight every 12 hours.
- The doctor will usually recommend that the patient also take aspirin (acetylsalicylic acid).
- The doctor will decide how long the patient should receive Crusia.
STEMI in patients 75 years of age or older:
- The usual dose is 75 IU (0.75 mg) per kilogram of body weight every 12 hours.
The maximum amount of Crusia in the first two doses is 7500 IU (75 mg).
- The doctor will decide how long the patient should receive Crusia.
Patient undergoing percutaneous coronary intervention (PCI):
Depending on when the last dose of Crusia was given, the doctor may decide to give an additional dose of Crusia before the PCI procedure.
Crusia will be given intravenously.
- 3. Prevention of blood clot formation in the dialyzer tubes
- The usual dose is 100 IU (1 mg) per kilogram of body weight.
- Crusia is injected into the tube returning blood from the body (into the so-called arterial line) at the start of the dialysis session. This dose usually lasts for a 4-hour dialysis session. However, if necessary, the doctor may give the patient an additional dose of 50 IU to 100 IU (0.5 to 1 mg) per kilogram of body weight.
Instructions for using the pre-filled syringe
Self-administration of Crusia
If the patient is able to self-administer Crusia, the doctor or nurse will show them how to do it. Do not attempt to self-administer the medicine without instruction.
If the patient is unsure what to do, they should talk to their doctor or nurse immediately. Proper administration of the injection under the skin (called "subcutaneous injection") will help reduce pain and bruising at the injection site.
Before self-administering Crusia
- Gather the necessary items: syringe, cotton ball, soap, and water, and a container for sharp objects.
- Check the expiration date on the packaging. Do not use the medicine after the expiration date.
- Check if the syringe is damaged and if the liquid is clear. If not, use another syringe.
- Make sure what dose is to be administered.
- Examine the abdomen to check if the last injection caused redness, discoloration, swelling, drainage, or if it is still painful. If so, consult a doctor or nurse.
Instructions for self-administering Crusia:
(Instructions for pre-filled syringes without a safety device)
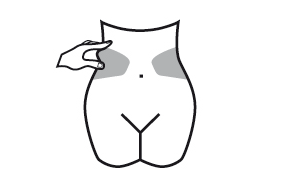
Preparing the injection site
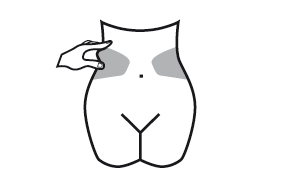
- 1) Choose an injection site on the right or left side of the abdomen. The injection site should be at least 5 cm away from the navel towards the sides.
- Do not inject within 5 cm of the navel or around existing scars or bruises.
- Alternate injection sites between the left and right side of the abdomen, depending on the location of the previous injection.
- 2) Wash your hands. Clean (do not rub) the injection site with an alcohol swab or soap and water.
- 3) Sit or lie down in a comfortable position, so you are relaxed. Make sure the injection site is in view. A chair, couch, or bed with pillows for support will be suitable.
Choosing the dose
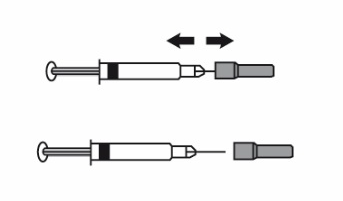
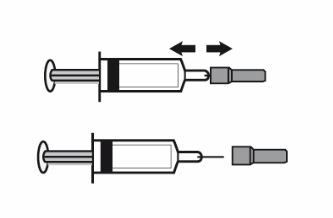
- 1) Carefully remove the needle cap from the syringe. Discard the cap.
- Do not press the plunger before injecting to remove air bubbles. This may reduce the administered dose.
- After removing the cap, do not touch the needle. This will ensure the sterility of the needle.
- 2) If the amount of medicine in the syringe is consistent with the prescribed dose, there is no need to adjust the dose. You can now administer the injection.
- 3) If the dose depends on body weight, it may be necessary to adjust the dose in the syringe according to the prescribed dose. In this case, excess medicine should be discarded, holding the syringe with the needle facing down (to maintain air bubbles in the syringe) and discarding the excess into a container.
- 4) A drop may appear at the tip of the needle. If so, remove the drop before injecting by tapping the syringe with the needle facing down. You can now administer the injection.
Administering the injection
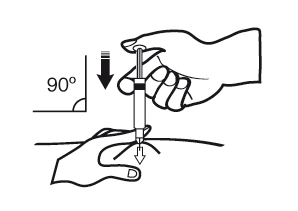
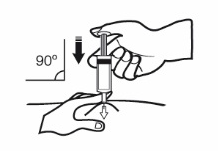
- 1) Hold the syringe in the hand you write with (like a pencil). With the other hand, gently grasp the cleaned skin of the abdomen with your index finger and thumb, creating a fold of skin between your fingers.
- Make sure to maintain the skin fold during the injection.
- 2) Hold the syringe with the needle facing down (perpendicular at a 90-degree angle). Insert the entire length of the needle into the skin fold.
- 3) Press the plunger with your thumb. This will introduce the medicine into the abdominal fat tissue. Administer the entire amount of medicine in the syringe.
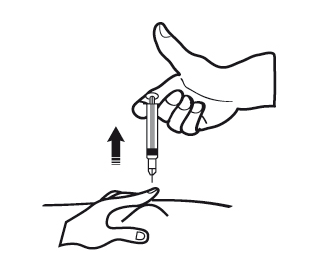
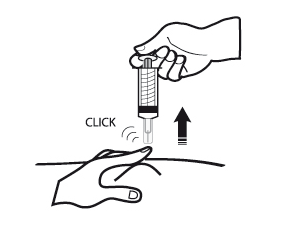
- 4) Remove the needle from the injection site, pulling it straight out. Keep the needle away from yourself and others. You can now release the skin fold.
After administering the injection
- 1) To avoid bruising, do not rub the injection site after administering the injection.
- 2) Dispose of the used syringe in a container for sharp objects. Close the container and store it in a place that is out of sight and reach of children. If the container is full, dispose of it according to the doctor's or pharmacist's instructions.
Any unused medicine or waste should be disposed of in accordance with local regulations.
If you feel that the dose is too strong (e.g., unexpected bleeding occurs) or too weak (e.g., the dose probably does not work), you should consult your doctor or pharmacist.
Keeping a diary helps ensure that you do not miss a dose of medicine.
Instructions for pre-filled syringes with a safety device:
Preparing the injection site
- 1) Choose an injection site on the right or left side of the abdomen. The injection site should be at least 5 cm away from the navel towards the sides.
- Do not inject within 5 cm of the navel or around existing scars or bruises.
- Alternate injection sites between the left and right side of the abdomen, depending on the location of the previous injection.
- 2) Wash your hands. Clean (do not rub) the injection site with an alcohol swab or soap and water.
- 3) Sit or lie down in a comfortable position, so you are relaxed. Make sure the injection site is in view. A chair, couch, or bed with pillows for support will be suitable.
Choosing the dose
- 1) Carefully remove the needle cap from the syringe. Discard the cap.
- Do not press the plunger before injecting to remove air bubbles. This may reduce the administered dose.
- After removing the cap, do not touch the needle. This will ensure the sterility of the needle.
- 2) If the amount of medicine in the syringe is consistent with the prescribed dose, there is no need to adjust the dose. You can now administer the injection.
- 3) If the dose depends on body weight, it may be necessary to adjust the dose in the syringe according to the prescribed dose. In this case, excess medicine should be discarded, holding the syringe with the needle facing down (to maintain air bubbles in the syringe) and discarding the excess into a container.
- 4) A drop may appear at the tip of the needle. If so, remove the drop before injecting by tapping the syringe with the needle facing down. You can now administer the injection.
Administering the injection
- 1) Hold the syringe in the hand you write with (like a pencil). With the other hand, gently grasp the cleaned skin of the abdomen with your index finger and thumb, creating a fold of skin between your fingers.
- Make sure to maintain the skin fold during the injection.
- 2) Hold the syringe with the needle facing down (perpendicular at a 90-degree angle). Insert the entire length of the needle into the skin fold.
- 3) Press the plunger with your thumb. This will introduce the medicine into the abdominal fat tissue. Administer the entire amount of medicine in the syringe.
- 4) Remove the needle from the injection site, pulling it straight out while still holding the plunger. Keep the needle away from yourself and others. The safety device is activated by firmly pressing the plunger. The protective cover will automatically cover the needle, and a clicking sound will be heard, confirming the activation of the protective cover. You can now release the skin fold.
After administering the injection
- 1) To avoid bruising, do not rub the injection site after administering the injection.
- 2) Dispose of the used syringe in a container for sharp objects. Close the container and store it in a place that is out of sight and reach of children. If the container is full, dispose of it according to the doctor's or pharmacist's instructions.
Any unused medicine or waste should be disposed of in accordance with local regulations.
If you feel that the dose is too strong (e.g., unexpected bleeding occurs) or too weak (e.g., the dose probably does not work), you should consult your doctor or pharmacist.
Keeping a diary helps ensure that you do not miss a dose of medicine.
Change of anticoagulant medicine
- Change from Crusia to medicines that thin the blood, called vitamin K antagonists (e.g., warfarin)The doctor will recommend blood tests to determine the INR (International Normalized Ratio) and, based on this, will inform the patient when to stop taking Crusia.
- Change from vitamin K antagonists (e.g., warfarin) to CrusiaThe patient should stop taking the vitamin K antagonist. The doctor will recommend blood tests to determine the INR and, based on this, will inform the patient when to start taking Crusia.
- Change from Crusia to direct oral anticoagulantsThe patient should stop taking Crusia. Then, they should start taking the direct oral anticoagulant 0-2 hours before the scheduled time of the next injection; and then continue taking the medicine as usual.
- Change from direct oral anticoagulant to CrusiaThe patient should stop taking the direct oral anticoagulant. Treatment with Crusia can be started 12 hours after the last dose of the direct oral anticoagulant.
Use of a higher than recommended dose of Crusia
If the patient thinks they have used too much or too little Crusia, they should immediately inform their doctor, nurse, or pharmacist, even if they do not notice any problems. If a child accidentally injects or swallows Crusia, they should go to the hospital emergency department immediately.
Missing a dose of Crusia
If a dose of medicine is missed, it should be taken as soon as possible. Do not take a double dose to make up for a missed dose. Keeping a diary helps ensure that you do not miss a dose of medicine.
Stopping the use of Crusia
If you have any further questions about the use of this medicine, you should ask your doctor, pharmacist, or nurse.
It is important to continue administering Crusia injections until the doctor recommends stopping them. If treatment is stopped, a blood clot may form, which can be very dangerous.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
As with other similar medicines (used to reduce blood clotting), Crusia may cause bleeding, which can be life-threatening. In some cases, bleeding may not be immediately visible.
If you experience any bleeding that does not stop on its own, as well as signs of excessive bleeding (severe weakness, fatigue, pallor, dizziness, headaches, or unexplained sweating), you should immediately consult your doctor. The doctor may decide to monitor the patient more closely or change the medicine.
If you experience any of the following symptoms, you should stop using enoxaparin and seek medical help immediately:
- Any symptoms of a severe allergic reaction (such as difficulty breathing, swelling of the lips, mouth, throat, or eyes).
- A red, scaly, widespread rash with thickening of the skin and blisters, accompanied by fever.
You should immediately consult your doctor:
- If the patient experiences any signs of a blood clot blocking a blood vessel, such as:
- cramping pain, redness, increased warmth, or swelling in one leg - these are symptoms of deep vein thrombosis
- shortness of breath, chest pain, fainting, or coughing up blood - these are symptoms of pulmonary embolism
- If the patient experiences a painful rash or dark red spots under the skin that do not fade when pressed. The doctor may order blood tests to check the platelet count.
Summary of possible side effects:
Very common (may affect more than 1 in 10 people)
- Bleeding.
- Increased liver enzyme activity.
Common (may affect up to 1 in 10 people)
- Increased tendency to bruise. This may be due to a decrease in platelet count.
- Pink spots on the skin. These changes are more likely at the injection sites of Crusia.
- Hives (urticaria).
- Itching, redness of the skin.
- Bruising or pain at the injection site.
- Decreased red blood cell count.
- Increased platelet count.
- Headache.
Uncommon (may affect up to 1 in 100 people)
- Sudden severe headache. This may be a sign of bleeding in the brain.
- Tenderness and swelling of the abdomen. This may be a sign of bleeding in the stomach.
- Large, red, irregularly-shaped skin changes with blisters or without blisters.
- Skin irritation (local irritation).
- The patient may notice yellowing of the skin or eyes and darker urine. This may indicate liver disease.
Rare (may affect up to 1 in 1,000 people)
- Severe allergic reaction. Symptoms of such a reaction may include: rash, difficulty swallowing or breathing, swelling of the lips, face, throat, or tongue.
- High potassium levels in the blood. This is more likely in people with kidney disease or diabetes. The doctor may check this with a blood test.
- Increased eosinophil count in the blood. The doctor may check this with a blood test.
- Hair loss.
- Osteoporosis (a condition where bones are more prone to fractures) after long-term use of the medicine.
- Numbness, tingling, and muscle weakness (especially in the lower part of the body) after a lumbar puncture or spinal anesthesia.
- Loss of control over the bladder or bowels (a condition where the patient cannot control when they need to go to the toilet).
- Hardening or a lump at the injection site.
Reporting side effects
If you experience any side effects, including those not listed in this leaflet, you should tell your doctor, pharmacist, or nurse. Side effects can be reported directly to the Department of Drug Safety Monitoring of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, tel.: +48 22 49 21 301, fax: +48 22 49 21 309, website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
Reporting side effects will help to gather more information on the safety of this medicine.
5. How to store Crusia
Store in a temperature below 25°C. Do not freeze.
Crusia pre-filled syringes are single-dose containers - any unused product should be discarded.
The medicine should be stored in a place that is out of sight and reach of children.
Do not use this medicine after the expiration date stated on the packaging. The expiration date refers to the last day of the month.
Do not use the medicine if the pre-filled syringe is damaged or if the product is not clear.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Contents of the packaging and other information
What Crusia contains
- The active substance of Crusia is enoxaparin sodium.
Each pre-filled syringe contains enoxaparin sodium equivalent to 2000 IU of anti-Xa activity (which is equivalent to 20 mg) in 0.2 ml of water for injection.
Each pre-filled syringe contains enoxaparin sodium equivalent to 4000 IU of anti-Xa activity (which is equivalent to 40 mg) in 0.4 ml of water for injection.
Each pre-filled syringe contains enoxaparin sodium equivalent to 6000 IU of anti-Xa activity (which is equivalent to 60 mg) in 0.6 ml of water for injection.
Each pre-filled syringe contains enoxaparin sodium equivalent to 8000 IU of anti-Xa activity (which is equivalent to 80 mg) in 0.8 ml of water for injection.
Each pre-filled syringe contains enoxaparin sodium equivalent to 10,000 IU of anti-Xa activity (which is equivalent to 100 mg) in 1.0 ml of water for injection.
- The other ingredient is water for injection.
What Crusia looks like and contents of the pack
Crusia is a clear, colorless to pale yellow solution for injection in a pre-filled syringe made of glass type I with a rubber stopper, plunger, and needle in a protective cover, with or without an automatic safety device. It is available in the following strengths:
Crusia 2000 IU (20 mg)/0.2 ml solution for injection in a 0.5 ml pre-filled syringe without graduation.
Pack sizes: 2, 6, 10, 20, and 50 pre-filled syringes.
Crusia 4000 IU (40 mg)/0.4 ml solution for injection in a 0.5 ml pre-filled syringe without graduation.
Pack sizes: 2, 6, 10, 20, 30, and 50 pre-filled syringes.
Crusia 6000 IU (60 mg)/0.6 ml solution for injection in a 1 ml pre-filled syringe.
Pack sizes: 2, 6, 10, 12, 24, 30, and 50 pre-filled syringes.
Crusia 8000 IU (80 mg)/0.8 ml solution for injection in a 1 ml pre-filled syringe.
Pack sizes: 2, 6, 10, 12, 24, 30, and 50 pre-filled syringes.
Crusia 10,000 IU (100 mg)/1 ml solution for injection in a 1 ml pre-filled syringe.
Pack sizes: 2, 6, 10, 12, 24, 30, and 50 pre-filled syringes.
Not all pack sizes may be marketed.
In some pack sizes, the pre-filled syringes may be connected to a safety device.
Marketing authorization holder and manufacturer:
Marketing authorization holder:
Laboratorios Farmacéuticos Rovi, S.A.
Julián Camarillo, 35
28037 Madrid
Spain
tel.: (+48) 699 711 147
Manufacturer:
ROVI Pharma Industrial Services S.A.
Julián Camarillo, 35
28037 Madrid
Spain
This medicine is authorized in the Member States of the European Economic Area and in the United Kingdom (Northern Ireland) under the following names:
Austria, Denmark, Finland, Netherlands, Germany, Norway, Sweden, United Kingdom (Northern Ireland), Spain, Portugal, Greece, Bulgaria, Czech Republic, Estonia, Croatia, Hungary, Latvia, Poland, Romania, Slovakia: Crusia
France: Enoxaparine Crusia
Italy: Rovinadil
Belgium, Ireland, Slovenia, Luxembourg: Teuro
Date of last revision of the leaflet: 01/2023
Other sources of information
Detailed information on this medicine is available on the website of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products: http://www.urpl.gov.pl/
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterRovi Pharma industrial Services, S.A.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to CrusiaDosage form: Solution, 12,000 IU (120 mg)/0.8 mlActive substance: enoxaparinPrescription requiredDosage form: Solution, 15,000 IU (150 mg)/mlActive substance: enoxaparinPrescription requiredDosage form: Solution, 2000 IU (20 mg)/0.2 mlActive substance: enoxaparin
Alternatives to Crusia in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Crusia in Hiszpania
Alternative to Crusia in Ukraina
Online doctors for Crusia
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Crusia – subject to medical assessment and local rules.














