
MEPIVACAINA B. BRAUN 20 MG/ML SOLUCIÓN INYECTABLE

Cómo usar MEPIVACAINA B. BRAUN 20 MG/ML SOLUCIÓN INYECTABLE
Traducción generada por IA
Este contenido ha sido traducido automáticamente y se ofrece solo con fines informativos. No sustituye la consulta con un profesional sanitario.
Ver originalContenido del prospecto
- Introducción
- Qué es Mepivacaína B. Braun 20 mg/ml y para qué se utiliza
- Qué necesita saber antes de usar Mepivacaína B. Braun 20 mg/ml
- Consulte a su médico o enfermero antes de que le administren Mepivacaina B. Braun 20 mg/ml:
- Cómo usar Mepivacaína B. Braun 20mg/ml
- Posibles efectos adversos
- Conservación de Mepivacaína B. Braun 20 mg/ml
- Contenido del envase e información adicional
Introducción
Prospecto: información para el paciente
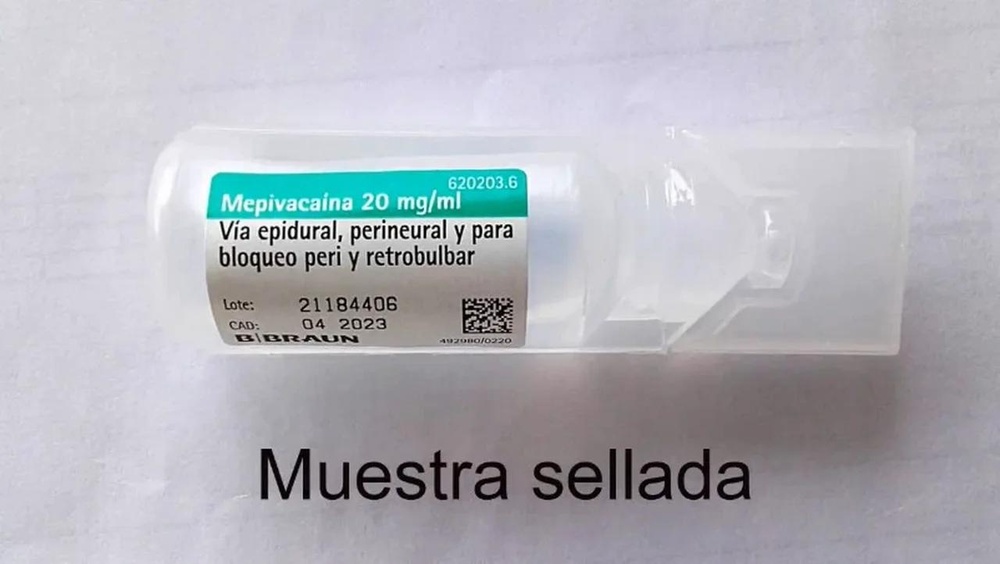
Mepivacaína B. Braun 20 mg/ml solución inyectable
Mepivacaina hidrocloruro
Lea todo el prospecto detenidamente antes de empezar a usar el medicamento porque contiene información importante para usted
- Conserve este prospecto ya que puede tener que volver a leerlo.
- Si tiene alguna duda, consulte a su médico, farmacéutico o enfermero.
- Si experimenta efectos adversos consulte a su médico, farmacéutico o enfermero, incluso si se trata de efectos adversos que no aparecen en este prospecto. Ver sección 4.
Contenido del prospecto:
- Qué es Mepivacaína B. Braun 20 mg/ml y para qué se utiliza
- Qué necesita saber antes de usar Mepivacaína B. Braun 20 mg/ml
- Cómo usar Mepivacaína B. Braun 20mg/ml
- Posibles efectos adversos
- Conservación de Mepivacaína B. Braun 20 mg/ml
- Contenido del envase e información adicional
1. Qué es Mepivacaína B. Braun 20 mg/ml y para qué se utiliza
La mepivacaína es un medicamento que pertenece al grupo de los anestésicos locales de tipo amida y está indicado en anestesia epidural y caudal, bloqueo de nervios periféricos, bloqueo de plexos nerviosos y anestesia para cirugía oftalmológica.
Dependiendo de la cantidad utilizada, detendrá totalmente el dolor o provocará una pérdida parcial de la sensibilidad.
Se utiliza antes de la cirugía o de varios exámenes médicos para prevenir o aliviar el dolor en el área de su cuerpo donde se llevará a cabo el procedimiento.
2. Qué necesita saber antes de usar Mepivacaína B. Braun 20 mg/ml
No le deben administrar Mepivacaína B. Braun 20 mg/ml:
- si es alérgico a la mepivacaina hidrocloruro, o a alguno de los demás componentes de este medicamento (incluidos en la sección 6).
- si es alérgico a otros anestésicos locales, p. ej.: Bupivacaina, Lidocaina.
- si sufre defectos graves en la coagulación de la sangre.
- si sufre de enfermedad nerviosa degenerativa.
- si tiene problemas graves con la conducción del impulso del corazón, u otros problemas cardíacos.
- si tiene epilepsia no controlada.
- Si tiene incrementada la presión cerebral.
Advertencias y precauciones
Consulte a su médico o enfermero antes de que le administren Mepivacaina B. Braun 20 mg/ml:
?
- si padece enfermedad nerviosa degenerativa.
?
?
?
?
?
?
?
?
?
- La dosis que va a recibir se controlará cuidadosamente para evitar que la mepivacaína cause reacciones tóxicas en su corazón o sus nervios y cerebro.
- Será observado cuidadosamente mientras se le administra la mepivacaína para detectar tan pronto como sea posible cualquier complicación que pueden afectar la función cardíaca, la circulación sanguínea o las funciones nerviosas y cerebrales, y darle cualquier tratamiento necesario en caso de que ocurran tales complicaciones.
Otros medicamentos y Mepivacaina B. Braun 20 mg/ml
Informe a su médico si está utilizando, ha utilizado recientemente o pudiera tener que utilizar cualquier otro medicamento.
La administración de Mepivacaína B. Braun 20 mg/ml junto con los siguientes medicamentos puede hacer necesario modificar la dosis de alguno de ellos o la interrupción del tratamiento:
- analgésicos fuertes;
- otros anestésicos locales;
- algunos medicamentos que se utilizan para tratar las alteraciones del ritmo del corazón;
- anestésicos generales como el éter;
- medicamento que producen vasoconstricción (reducción del diámetro de los vasos sanguíneos);
- heparina, medicamentos anticoagulantes (que impiden la coagulación de la sangre), antiinflamatorios no esteroideos y substitutivos del plasma (productos que se utilizan ante una pérdida de sangre). Su función de coagulación sanguínea se controlará cuidadosamente si está recibiendo alguno de estos medicamentos;
- inhibidores del citocromo PYP 1A2 (como ciprofloxacina, enoxacina o fluvoxamina);
- medicamentos utilizados para tratar el ardor y úlceras de estómago e intestinos (como la cimetidina);
- Propranolol.
La Mepivacaína generalmente no se combina con otros anestésicos locales.
Uso en niños y ancianos
Los ancianos requieren dosis menores que los adultos jóvenes o de mediana edad.
No debe usarse en en niños y adolescentes menores de 15 años.
Embarazo, lactancia y fertilidad
Si está embarazada o en periodo de lactancia, cree que podría estar embarazada o tiene intención de quedarse embarazada, consulte a su médico o farmacéutico antes de utilizar este medicamento.
Durante el embarazo sólo se le administrará Mepivacaina B. Braun 20 mg/ml tras una estricta consideración de las indicaciones y si su médico lo considera absolutamente necesario. Su médico tomará cualquier posible precaución para evitar daños a usted o su hijo no nato.
La mepivacaína no es un fármaco de preferencia en la anestesia epidural en obstetricia.
Se le administrará este medicamento durante la lactancia solo si su médico lo considera necesario. Si fuera necesaria dicha administración, la lactancia se debe interrumpir hasta 24 horas después de la finalización del tratamiento.
Conducción y uso de máquinas:
Mepivacaina B. Braun 20 mg/ml puede alterar temporalmente su capacidad de movimiento, atención y coordinación. Su médico le indicará si puede conducir o utilizar máquinas.
Mepivacaína B.Braun 20 mg/ ml contiene sodio
Ampollas de 5 ml:
Este medicamento contiene menos de 23 mg de sodio (1 mmol) por cada ampolla de 5 ml, esto es, esencialmente “exento de sodio”.
Ampollas de 10 ml:
Este medicamento contiene menos de 23 mg de sodio (1 mmol) por cada ampolla de 10 ml, esto es, esencialmente “exento de sodio”.
Ampollas de 20 ml:
Este medicamento contiene 40 mg de sodio (componente principal de la sal de mesa/para cocinar) en cada ampolla de 20 ml. Esto equivale al 2% de la ingesta diaria máxima de sodio recomendada para un adulto.
3. Cómo usar Mepivacaína B. Braun 20mg/ml
Mepivacaína B. Braun 20 mg/ml se administra por vía epidural y perineural para el bloqueo de la conducción nerviosa y vías de administración para bloqueos peri y retrobulbar en cirugía oftalmológica.
Será administrada por personal sanitario únicamente y su médico determinará cual es la dosis más adecuada para usted. Se debe utilizar siempre la dosis más pequeña requerida para producir la anestesia deseada. La dosificación debe ajustarse individualmente de acuerdo con la edad y peso del paciente así como a las particularidades de cada caso.
En pacientes con enfermedades del hígado, riñón, corazón, mal estado general y en ancianos, es necesario una precaución especial y un ajuste cuidadoso de la dosis.
Su médico le pedirá que hable con el / ella mientras le administra el medicamento para asegurarse de que está consciente.
Su presión arterial puede ser medida de vez en cuando.
Si se le administra más Mepivacaína B. Braun 20 mg/ml de la que debiera:
La sobredosis puede provocar signos y síntomas de intoxicación. La gravedad de los signos y síntomas depende de la dosis administrada. Se puede observar lo siguiente:
- Síntomas en el nervioso central:
Intoxicación leve:
Hormigueo y entumecimiento en el área de la boca, sabor metálico, alteraciones de la audición y la visión, bostezos, ansiedad, inquietud, escalofríos, espasmos musculares, náuseas, vómitos, desorientación.
Intoxicación moderada:
Trastornos del habla, somnolencia, náuseas, vómitos, mareos, somnolencia, confusión, temblor, movimientos coreiformes, convulsiones, midriasis, taquipnea.
Intoxicación grave:
Vómitos (riesgo de asfixia), parálisis del esfínter, pérdida de tono muscular y reactividad, estupor, respiración irregular, parálisis respiratoria, coma, muerte.
- Sintomas en el sistema cardiovascular
Intoxicación leve:
Palpitaciones, hipertensión, taquicardia, taquipnea.
Intoxicación moderada:
Taquicardia, arritmias cardíacas, hipoxia, palidez.
Intoxicación grave:
Hipoxia y cianosis severas, insuficiencia cardíaca primaria, hipotensión, arritmias cardíacas (bradicardia, fibrilación auricular, asistolia).
En tales casos, recibirá el tratamiento necesario primero para normalizar y estabilizar las funciones de su corazón, circulación y respiración y seguidamente para controlar las convulsiones y otros síntomas nerviosos graves. Esto incluye administrar oxígeno y medicación adicional, principalmente para normalizar la función y circulación del corazón.
En caso de sobredosis o ingestión accidental, consulte inmediatamente a su médico, enfermero o farmacéutico o llame al Servicio de Información Toxicológica, teléfono: 91 652 04 20, indicando el medicamento y la cantidad ingerida.
4. Posibles efectos adversos
Al igual que todos los medicamentos, este medicamento puede producir efectos adversos, aunque no todas las personas los sufran.
Frecuentes(pueden afectar hasta a 1 de cada 10 personas):
- Sensación de quemazón, pinchazos y hormigueo en la piel (parestesia) y vértigo.
- Ritmo cardiaco lento y anormal (bradicardia).
- Hipotensión.
- Hipertensión.
- Náuseas.
- Vómitos.
Poco frecuentes (puede afectar hasta a 1 de cada 100 personas):
- Mareo (ligero aturdimiento).
- Temblor.
- Depresión del Sistema Nervioso Central.
- Pérdida de consciencia.
- Convulsiones (incluidas las crisis epilépticas).
- Trastornos del habla como dificultad para articular sonidos y palabras ( disartria) y charlatanería excesiva (logorrea).
- Afectación visual
- Zumbido de oídos (acufenos).
Raros (pueden afectar hasta a 1 de cada 1.000 personas):
- Reacciones anafilácticas /anafilactoides.
- Reacciones alérgicas.
- Dolor debido a la lesión en el nervio (neuropatía).
- Daño neural periférico
- Aracnoiditis.
- Diplopía (parálisis de los músculos oculares).
- Paro cardíaco.
- Angina de pecho.
- Problemas de coordinación del latido cardíaco (bloqueo auriculoventricular).
- Arritmia cardiaca.
- Dificultad para respirar.
Frecuencia no conocida (la frecuencia no puede estimarse a partir de los datos disponibles):
- Euforia.
- Ansiedad/nerviosismo.
- Incapacidad del corazón para contraerse de forma efectiva (depresión miocárdica)
Efectos adversos debidos a errores de uso
Se puede producir una anestesia espinal extensa (total) mediante la inyección intratecal inadvertida durante la anestesia epidural planificada, como resultado del uso de un volumen demasiado grande o la colocación incorrecta del paciente (cuando se usan soluciones no isobáricas).
Los primeros signos son inquietud y somnolencia que pueden llevar a la pérdida del conocimiento y al paro respiratorio.
Comunicación de efectos adversos
Si experimenta cualquier tipo de efecto adverso, consulte a su médico o farmacéutico, incluso si se trata de posibles efectos adversos que no aparecen en este prospecto. También puede comunicarlos directamente a través del Sistema Español de Farmacovigilancia de Medicamentos de Uso Humano: www.notificaRAM.es. Mediante la comunicación de efectos adversos usted puede contribuir a proporcionar más información sobre la seguridad de este medicamento.
5. Conservación de Mepivacaína B. Braun 20 mg/ml
Mantener fuera de la vista y del alcance de los niños.
No requiere condiciones especiales de conservación.
No utilice Mepivacaína B. Braun 20 mg/ml después de la fecha de caducidad que aparece en el envase (después de CAD). La fecha de caducidad es el último día del mes que se indica.
El contenido de la ampolla debe ser utilizado inmediatamente tras su apertura. Una vez abierto, desechar la porción no utilizada de la solución. Para un solo uso. No utilice este medicamento si observa partículas.
Los medicamentos no se deben tirar por los desagües ni a la basura. Pregunte a su farmacéutico cómo deshacerse de los envases y de los medicamentos que no necesita. De esta forma ayudará a proteger el medio ambiente.
6. Contenido del envase e información adicional
Composición de Mepivacaína B. Braun 20 mg/ml
Principio Activo | Por 1 ml | Por 5 ml | Por 10 ml | Por 20 ml |
Mepivacaina hidrocloruro | 20 mg | 100 mg | 200 mg | 400 mg |
Los demás excipientes son: cloruro sódico, hidróxido sódico (para ajuste de pH) y agua para preparaciones inyectables en cantidad suficiente.
Aspecto del producto y contenido del envase
Mepivacaína B. Braun 20 mg/ml es una solución inyectable que se presenta en ampollas de polietileno (Mini-Plasco) de 5, 10 y 20 ml. Se presenta en envases de 1 ampolla y 100 ampollas.
Puede que no se comercializen todos los formatos.
Titular de la autorización de comercialización y responsable de la fabricación
- Braun Medical, S.A.
Ctra. de Terrassa, 121
08191-Rubí (Barcelona)
España
Fecha de la última revisión de esteprospecto: agosto 2020
La información detalladay actualizadade este medicamento está disponible en la página Web de la Agencia Española de Medicamentos y Productos Sanitarios(AEMPS):http://www.aemps.gob.es/.
--------------------------------------------------------------------------------------------
Esta información está destinada únicamente a médicos o profesionales del sector sanitario:
Mepivacaína B. Braun 20 mg/ml solo debe ser utilizada por médicos con experiencia en anestesia regional y en técnicas de reanimación o bajo su supervisión. Debe haber disponibles equipos de reanimación cuando se administren anestésicos locales. Debe administrarse la dosis más baja posible que produzca el efecto deseado. La dosis debe ajustarse individualmente a las particularidades de cada caso.
Posología
Se debe utilizar siempre la dosis más pequeña requerida para producir la anestesia deseada. La dosificación debe ajustarse individualmente de acuerdo con la edad y peso del paciente así como a las particularidades de cada caso.
.
Anestesia caudal y epidural, bloqueos nerviosos periféricos:
La dosis no debe de exceder de los 400 mg.
La dosis máxima diaria es de 1g.
Mepivacaína B. Braun 20 mg/ml solución inyectable puede administrarse de forma continua.
Para diferentes tipos de usos, se recomiendan las siguientes dosis:
Bloqueo del nervio ciático | 15 – 20 ml |
Bloqueo del plexo braquial | 3 - 5 ml |
Cirugía oftalmológica | |
| 3 ml |
| 5 -7,5 ml |
Anestesia epidural para cirugía | 5 – 15ml |
Anestesia caudal | 10 – 20 ml |
Para obtener más detalles sobre las dosis que se aplicarán para anestesiar nervios específicos o para técnicas anestésicas específicas, consulte los libros de texto estándar.
Pacientes de edad avanzada
Puede ser necesario aplicar dosis más bajas para pacientes de edad avanzada o aquellos en mal estado general.
Población pediátrica
Las dosis para adolescentes a partir de 15 años son las indicadas anteriormente para adultos.
No está indicado para menores de 15 años.
Insuficiencia hepática
En pacientes con insuficiencia hepática no es necesaria una reducción de la dosis para la anestesia quirúrgica.
Cuando se usan bloqueos prolongados, por ejemplo, mediante administración repetida, las dosis repetidas de mepivacaína deben reducirse en un 50% en pacientes con enfermedad hepática de grado C (clasificación de Child-Pugh) y la dosis total en 24 horas no debe de exceder de 750 mg de mepivacaína.
Insuficiencia renal
No es necesaria una reducción de la dosis para la anestesia quirúrgica hasta las 24 h en pacientes con disfunción renal.
Administración
- Vía perineural, epidural para bloqueo de la conducción nerviosa.
- Cirugía oftalmológica: vías de administración para bloqueos peri y retrobulbar.
La anestesia local no debe ser inyectada en zonas infectadas.
Antes de la inyección debe asegurarse que la aguja no está situada intravascularmente.La inyección debe efectuarse de forma lenta y fraccionada.
Normas básicas a seguir:
- Elegir la dosificación más baja posible.
- Utilizar una aguja de la dimensión apropiada.
- Inyectar lentamente con varias aspiraciones en dos planos (rotar la aguja 180º).
Se debe tener mucho cuidado para evitar la inyección intravascular accidental. Es esencial realizar una aspiración cuidadosa.
- Controlar la presión sanguínea.
- Tener en cuenta la premedicación. La premedicación debería incluir la administración profiláctica de atropina y - en función de las cantidades convenientes de anestésico local a inyectar - un barbitúrico de acción corta.
- Si es necesario, suspender la administración de anticoagulantes antes de la administración del anestésico local.
- Observar las contraindicaciones generales y específicas para los diversos métodos de anestesia local o regional.
Para la administración epidural continua deben utilizarse soluciones de mepivacaína más diluidas.
Para la anestesia epidural, se debe administrar una dosis de prueba, que consiste en 3 - 4 ml de un anestésico local con adrenalina añadida (1: 200 000) antes de la dosis completa, debido a que una inyección intravascular de adrenalina es rápidamente reconocida debido al aumento de la frecuencia cardíaca. La frecuencia cardíaca debe medirse repetidamente hasta 5 minutos después de la administración de la dosis de prueba.
Debe mantenerse el contacto verbal con el paciente y el ritmo cardiaco debe ser medido repetidamente hasta 5 minutos después de la administración de la dosis de prueba. Debe repetirse la aspiración antes de administrar la dosis principal. La dosis principal debe inyectarse lentamente y, especialmente al incrementar la dosis, mantener contacto constante con el paciente. La administración debe interrumpirse inmediatamente a los primeros síntomas de toxicidad.
Antes de administrar un anestésico local debe asegurarse que el equipo necesario para la reanimación, p. ej.: fuente de oxígeno, material para mantener libre el tracto respiratorio y medicación de emergencia para el tratamiento de las reacciones tóxicas, está disponible de forma inmediata.
- País de registro
- Principio activo
- Requiere recetaSí
- Fabricante
- Esta información es de carácter general y no sustituye la consulta con un profesional sanitario.
- Alternativas a MEPIVACAINA B. BRAUN 20 MG/ML SOLUCIÓN INYECTABLEForma farmacéutica: INYECTABLE, 54 mgPrincipio activo: mepivacaineFabricante: Laboratorios Clarben S.A.Requiere recetaForma farmacéutica: INYECTABLE, 10 mg/mlPrincipio activo: mepivacaineFabricante: B Braun Medical S.A.Requiere recetaForma farmacéutica: INYECTABLE, 3% mepivacaina hidrocloruroPrincipio activo: mepivacaineFabricante: Farmalider S.A.Requiere receta
Médicos online para MEPIVACAINA B. BRAUN 20 MG/ML SOLUCIÓN INYECTABLE
Comenta la dosis, los posibles efectos secundarios, interacciones, contraindicaciones o la revisión de receta de MEPIVACAINA B. BRAUN 20 MG/ML SOLUCIÓN INYECTABLE, sujeto a valoración médica y a la normativa local.
Preguntas frecuentes















