LEVOSERT 0,02 MG CADA 24 HORAS SISTEMA DE LIBERACION INTRAUTERINO

Cómo usar LEVOSERT 0,02 MG CADA 24 HORAS SISTEMA DE LIBERACION INTRAUTERINO
Traducción generada por IA
Este contenido ha sido traducido automáticamente y se ofrece solo con fines informativos. No sustituye la consulta con un profesional sanitario.
Ver originalContenido del prospecto
Introducción
Prospecto: información para la usuaria
Levosert 0,02mg cada 24horas sistema de liberación intrauterino
levonorgestrel
Lea todo el prospecto detenidamente antes de empezar a usar este medicamento, porque contiene información importante para usted.
- Conserve este prospecto, ya que puede tener que volver a leerlo.
- Si tiene alguna duda, consulte a su médico o farmacéutico.
- Si experimenta efectos adversos, consulte con su médico o farmacéutico, incluso si se trata de efectos adversos que no aparecen en este prospecto. Ver sección 4.
Contenido del prospecto
- Qué es Levosert y para qué se utiliza
- Qué necesita saber antes de empezar a usar Levosert
- Cómo usar Levosert
- Posibles efectos adversos
- Conservación de Levosert
- Contenido del envase e información adicional
1. Qué es Levosert y para qué se utiliza
Levosert es un sistema de liberación intrauterino (SLI) para su inserción en el útero, donde libera lentamente la hormona levonorgestrel.
Se usa para:
Anticoncepción
Este medicamento es un método anticonceptivo eficaz a largo plazo, no permanente (reversible).
Este medicamento evita el embarazo al adelgazar el revestimiento de la matriz (útero), haciendo más espeso el moco normal de la abertura del útero (canal cervical), de modo que los espermatozoides no pueden atravesarlo para fecundar el óvulo, y evitando la liberación de los óvulos (ovulación) en algunas mujeres. Además, la presencia del cuerpo en forma de T provoca efectos locales en el revestimiento del útero.
El sistema debe retirarse después de 8 años de uso cuando se utiliza como anticonceptivo.
Tratamiento del sangrado menstrual abundante
Este medicamento también es útil para reducir el flujo sanguíneo menstrual, de modo que lo puede usar si sufre sangrado menstrual (periodos) abundante. Esto se denomina menorragia. La hormona en este medicamento actúa adelgazando el revestimiento de su útero para que haya menos sangrado cada mes.
El sistema deberá retirarse o sustituirse trascurridos 8 años de uso, o antes si reaparece el sangrado menstrual abundante o molesto.
Niños y adolescentes
Este medicamento no está indicado para su uso antes del primer sangrado menstrual (menarquia).
2. Qué necesita saber antes de empezar a usar Levosert
No use Levosert:
- si está embarazada o sospecha que puede estar embarazada;
- si tiene o ha tenido una enfermedad inflamatoria pélvica;
- si tiene un flujo vaginal inusual o desagradable, o picor vaginal, ya que esto puede indicar una infección;
- si tiene o ha tenido inflamación del revestimiento del útero tras un parto;
- si tiene o ha tenido infección en el útero tras un parto o tras un aborto en los últimos 3 meses;
- si tiene o ha tenido inflamación del cérvix ( el cuello del útero);
- si tiene o ha tenido un test de Papanicolau anómalo (cambios en el cervix);
- si tiene o ha tenido problemas en el hígado;
- si tiene un tumor en el hígado;
- si tiene una anomalía uterina, incluyendo fibromas uterinos, especialmente aquellos que distorsionan la cavidad uterina.- tiene un patrón de sangrado vaginal anómalo;
- si tiene una afección que le hace susceptible de infecciones. Un médico le habrá dicho si tiene este tipo de condición;
- si tiene o ha tenido cáncer dependiente de hormonas, como el cáncer de mama;
- si tiene o ha tenido o sospecha de la existencia de cualquier tipo de cáncer, incluido cancer de la sangre (leucemia), uterino y cervical, a menos que esté en remisión;
- si tiene o ha tenido enfermedad trofoblástica. Un médico le habrá dicho si tiene este tipo de enfermedad;
- si es alérgica a levonorgestrel o a cualquiera de los demás componentes de este medicamento (incluidos en la sección 6).
Advertencias y precauciones
Antes de que se le coloque este medicamento, su médico o enfermero le harán algunas pruebas para asegurarse de que este medicamento es adecuado para usted. Esto incluirá un examen pélvico y también puede incluir otros exámenes, como un examen de los senos, si su médico o enfermero lo consideran apropiado.
Las infecciones genitales tendrán que ser tratadas con éxito antes de que se le pueda colocar este medicamento.
Si tiene epilepsia, comuníqueselo al médico o al enfermero antes de que le coloque este medicamento porque, aunque es poco frecuente, puede producirse un ataque durante la inserción. Algunas mujeres pueden sentir que se desmayan después del procedimiento. Esto es normal y su médico o enfermero le dirá que descanse un rato.
Este medicamento puede no ser adecuado para todas las mujeres.
Levosert, como otros anticonceptivos hormonales, no protege contra la infección del VIH (SIDA) o de cualquier otra enfermedad de transmisión sexual (p. ej., clamidia, herpes genital, verrugas genitales, gonorrea, hepatitis B y sífilis). Necesitará preservativos para protegerse de estas enfermedades.
Hable con su médico antes de usar Levosert:
- si tiene o desarrolla migraña, mareos, visión borrosa, dolores de cabeza peores de lo normal, o si tiene dolor de cabeza con más frecuencia que antes;
- si tiene una coloración amarilla en la piel o en el blanco de los ojos (ictericia);
- si es diabética (nivel demasiado alto de azúcar en sangre), tiene tensión arterial alta o niveles anómalos de lípidos sanguíneos;
- si ha tenido cancer que afecta a la sangre (incluida leucemia) que está ahora en remisión
- si está bajo tratamiento con esteriodes a largo plazo;
- si ha tenido alguna vez un embarazo ectópico (desarrollo del feto fuera del útero) o antecedentes de quistes ováricos;
- si ha tenido o tiene una enfermedad arterial grave, como ataque al corazón o accidente cerebrovascular, o si tiene algún problema cardíaco;
- si tiene antecedentes de coágulos sanguíneos (trombosis);
- si está tomando otros medicamentos, ya que ciertos medicamentos pueden evitar que Levosert funcione correctamente;
- si tiene sangrados irregulares;
- si tiene ataques (epilepsia).
Si tiene o ha tenido alguna de las afecciones indicadas anteriormente, su médico decidirá si puede usar Levosert.
También debe informar a su médico si alguna de estas afecciones se presenta por primera vez mientras tiene colocado Levosert.
Debe ver a un médico o enfermera lo antes posible si presenta una hinchazón dolorosa en la pierna, dolor repentino en el pecho, o dificultad para respirar, puesto que estos pueden ser signos de un coágulo sanguíneo. Es importante que todo coágulo sanguíneo se trate de inmediato.
Expulsión
Las contracciones musculares del útero durante la menstruación pueden a veces empujar el SLI fuera de su sitio o expulsarlo. Es más probable que esto ocurra si tiene sobrepeso en el momento de la inserción del SLI o si tiene antecedentes de menstruaciones abundantes. Si el SLI se sale de su sitio, es posible que no funcione como es debido y, por tanto, el riesgo de embarazo aumenta. Si el SLI se expulsa, ya no está protegida frente al embarazo.
Los síntomas posibles de una expulsión son dolor y sangrado anormal, pero Levosert también puede ser expulsado sin darse cuenta. Debido a que Levosert reduce el flujo menstrual, un aumento del mismo puede ser indicativo de una expulsión.
Es recomendable que verifique los hilos con su dedo, por ejemplo, mientras se ducha. Vea también la sección 3 “Cómo usar Levosert - ¿Cómo puedo saber si Levosert está bien colocado?”. Si presentase signos que indiquen la expulsión o no fuera capaz de palpar los hilos, debería usar un método anticonceptivo adicional (como preservativos), y consultar con su profesional sanitario.
Trastornos psiquiátricos
Algunas mujeres que utilizan anticonceptivos hormonales como Levosert han notificado depresión o un estado de ánimo deprimido. La depresión puede ser grave y a veces puede inducir pensamientos suicidas. Si experimenta alteraciones del estado de ánimo y síntomas depresivos, póngase en contacto con su médico para obtener asesoramiento médico adicional lo antes posible.
Levosert y el hábito tabáquico
Se aconseja a las mujeres que dejen de fumar. Fumar incrementa el riesgo de desarrollar infarto, accidente cerebrovascular, o coágulos sanguíneos.
Uso de tampones o copas menstruales
Se recomienda el uso de compresas. Si se usan tampones o copas menstruales, debe cambiarlos con cuidado para no tirar de los hilos de Levosert.
Uso de Levosert con otros medicamentos
El efecto de los anticonceptivos hormonales como Levosert puede verse reducido por medicamentos que aumentan la cantidad de enzimas producidas por el hígado. Informe a su médico si está tomando:
- fenobarbital, fenitoína o carbamazepina (para tratar la epilepsia);
- griseofulvina (un antifúngico);
- rifampicina o rifabutina (antibióticos);
- nevirapina o efavirenz (para el VIH).
Informe a su médico si está tomando, ha tomado recientemente o podría tener que tomar cualquier otro medicamento. Levosert no debe usarse simultáneamente con otro anticonceptivo hormonal.
Embarazo, lactancia y fertilidad
No debe usar Levosert durante el embarazo o si sospecha que puede estar embarazada.
¿Me puedo quedar embarazada mientras uso Levosert?
Es muy raro que una mujer se quede embarazada teniendo colocado Levosert.
No tener un periodo no necesariamente significa que está embarazada. Algunas mujeres pueden no tener reglas mientras usan el sistema.
Si no ha tenido un periodo durante 6 semanas, considere hacerse una prueba de embarazo. Si es negativa, no hay necesidad de realizarse más pruebas, a menos que tenga otros síntomas de embarazo, como por ejemplo náuseas, cansancio o sensibilidad en los pechos.
Si se queda embarazada con el dispositivo colocado, contacte con su médico lo antes posible para descartar un embarazo ectópico (desarrollo del feto fuera del útero) y se le pueda extraer Levosert para reducir el riesgo de un aborto espontáneo. Sin embargo, si Levosert se deja colocado durante el embarazo, no sólo aumenta el riesgo de sufrir un aborto espontáneo, sino también el riesgo de parto prematuro. Si Levosert no se puede extraer, hable con su profesional sanitario sobre los beneficios y riesgos de continuar el embarazo. Si el embarazo continúa, será monitorizada de cerca durante su embarazo y debe contactar con su médico de inmediato si experimenta calambres estomacales, dolor de estómago o fiebre.
Levosert contiene una hormona denominada levonorgestrel, y ha habido casos aislados de efectos genitales en los bebés si se exponen a dispositivos intrauterinos de levonorgestrel mientras están en el útero.
¿Y si quiero tener un bebé?
Si desea tener un bebé, pídale a su médico que le extraiga Levosert. Su nivel normal de fertilidad volverá muy rápidamente una vez el sistema se haya extraído.
¿Puedo dar el pecho mientras uso Levosert?
En la leche materna se encuentran cantidades muy pequeñas de la hormona de Levosert. No se espera que haya riesgo alguno para el recién nacido. Puede continuar la lactancia durante el uso de este medicamento.
Conducción y uso de máquinas
No hay efectos conocidos sobre la capacidad de conducir y utilizar máquinas.
Levosert contiene sulfato de bario.
El cuerpo en forma de T de Levosert contiene sulfato de bario por lo que puede verse en las radiografías.
3. Cómo usar Levosert
Solamente un médico o enfermera con formación específica puede colocar el sistema (ver las instrucciones especiales para la inserción en el envase).
El profesional le explicará el procedimiento de colocación y cualquier riesgo asociado a su uso. Después será examinada por su médico o enfermera antes de la inserción de Levosert. Si tiene cualquier duda sobre su uso puede consultarlo con ellos.
Empezar a usar Levosert
- Antes de insertar Levosert, es necesario asegurarse de que no está embarazada.
- Debería tener Levosert insertado en un plazo de 7 días a partir del inicio de la menstruación. Cuando Levosert se inserta en estos días, Levosert actúa de inmediato y evitará que quedes embarazada.
- Si no puede tener Levosert insertado en un plazo de 7 días a partir del inicio de la menstruación o si su periodo menstrual llega en momentos impredecibles, Levosert puede ser insertado en cualquier otro día. En este caso, no debe haber tenido relaciones sexuales sin anticoncepción desde su último periodo menstrual, y debe tener una prueba de embarazo negativa antes de la inserción. Además, Levosert puede no prevenir el embarazo de manera confiable de inmediato. Por lo tanto, debe usar un método de barrera anticonceptiva (como preservativos) o abstenerse de relaciones sexuales vaginales durante los primeros 7 días después de la inserción de Levosert.
- Levosert no es adecuado para uso como anticonceptivo de emergencia (anticonceptivo postcoital).
Empezar a usar Levosert después del parto
- Levosert puede ser insertado después del parto una vez que el útero haya vuelto a su tamaño normal, pero no antes de las 6 semanas posteriores al parto (ver sección 4 “Posibles efectos adversos – Perforación”).
- Ver también “Empezar a usar Levosert” más arriba para conocer qué más necesita saber sobre el momento de la inserción.
Empezar a usar Levosert después de un aborto
Levosert puede ser insertado inmediatamente después de un aborto, si el embarazo fue de menos de 3 meses de duración siempre que no haya infecciones genitales. En este caso, Levosert funcionará de inmediato.
Sustitución de Levosert
Levosert se puede sustituir por un nuevo Levosert en cualquier momento de su ciclo menstrual. En este caso, Levosert funcionará de inmediato.
Cambio de otro método anticonceptivo (como anticonceptivos hormonales combinados, implante)
- Levosert puede ser insertado inmediatamente si hay una certeza razonable de que no está embarazada.
- Si han pasado más de 7 días desde el inicio de su sangrado menstrual, debe abstenerse de mantener relaciones sexuales vaginales o usar protección anticonceptiva adicional durante los próximos 7 días.
Colocación de Levosert
El examen realizado por su profesional sanitario antes de la colocación puede incluir:
- una prueba de citología cervical (frotis de Papanicolaou);
- un examen de las mamas;
- otras pruebas, por ejemplo para infecciones, incluidas enfermedades de transmisión sexual, prueba de embarazo, según sea necesario. Su profesional sanitario también hará un examen ginecológico para determinar la posición y el tamaño del útero.
Después del examen ginecológico
- Un instrumento denominado espéculo se introduce en la vagina, y el cérvix puede ser limpiado con una solución antiséptica. Entonces, Levosert es colocado en el útero utilizando un tubo fino y flexible de plástico (el tubo de colocación). Se puede aplicar anestesia local en el cérvix antes de la colocación.
- Algunas mujeres se sienten mareadas o se desmayan durante la colocación o después de que Levosert sea colocado o retirado.
- Puede experimentar algo de dolor y sangrado durante o justo después de la colocación.
Después de la colocación de Levosert debería recibir una tarjeta de recordatorio para la paciente de su médico para exámenes de seguimiento. Lleve esta tarjeta con usted a cada cita programada.
¿Con qué rapidez funciona Levosert?
Anticoncepción
Si Levosert es insertado en su útero ya sea durante su periodo menstrual o dentro de los 7 días posteriores al inicio de su periodo o tiene un dispositivo y es momento de reemplazarlo por uno nuevo o si acaba de tener un aborto, usted está protegida contra el embarazo desde el momento en que le colocan el sistema.
Sangrado menstrual abundante
Levosert normalmente logra una reducción significativa de la pérdida de sangre menstrual en el plazo de 3 a 6 meses de tratamiento.
¿Cómo afectará Levosert a mis periodos?
Muchas mujeres tienen manchados (una pequeña pérdida de sangre) en los primeros 3-6 meses tras la colocación del sistema. Otras tendrán sangrados prolongados o abundantes. Sin embargo, puede presentar un aumento de sangrado, normalmente en los primeros 2 a 3 meses, antes de que se logre una reducción de la pérdida de sangre. En general, tiene más posibilidades de tener menos días de sangrado cada mes y puede que incluso deje de tener el periodo. Esto se debe al efecto de la hormona (levonorgestrel) en el revestimiento del útero. Si no se consigue una reducción notable de la pérdida de sangre al cabo de 3 a 6 meses, deben considerarse otros tratamientos.
Si ha tenido colocado Levosert durante un periodo prolongado de tiempo y luego empieza a tener problemas de sangrado, contacte con su médico o profesional sanitario para que le aconseje.
¿Con qué frecuencia debería hacerme un control del sistema?
Debe comprobar su Levosert al cabo de 4 a 6 semanas después de la colocación, y a partir de entonces regularmente, al menos una vez al año hasta su retirada. Su médico podrá determinar con qué frecuencia y qué tipos de controles son requeridos en su caso particular. Lleve la tarjeta de recordatorio para la paciente que recibió de su médico a cada cita programada. Además, debe ponerse en contacto con su médico si presenta alguno de los síntomas descritos en la sección 2 “Advertencias y precauciones”.
¿Cómo puedo saber si el sistema está en su lugar?
Tras cada periodo menstrual, puede buscar los dos hilos finos que están unidos al extremo inferior del sistema. Su médico le enseñará cómo hacerlo.
No tirede los hilos, porque podría sacarlo accidentalmente. Si no encuentra los hilos, contacte con su médico o enfermera lo antes posible y evite las relaciones sexuales o use un método anticonceptivo de barrera (como los preservativos) mientras tanto.Puede que los hilos simplemente hayan entrado en el útero o canal cervical. Si su médico o enfermera sigue sin encontrar los hilos, puede que se hayan roto, o Levosert podría haber salido por sí solo, o en raros casos puede haber perforado la pared del útero (perforación uterina, ver sección 4).
También debería ir al médico si puede tocar el extremo inferior del dispositivo mismo, o si usted o su pareja sienten dolor o molestias durante las relaciones sexuales.
¿Qué sucede si el sistema se sale por sí solo?
Si el sistema se sale completamente o en parte, puede que no esté protegida contra el embarazo. Es raro, pero posible, que esto suceda sin que usted se dé cuenta durante el periodo menstrual. Un incremento inusual de la cantidad de sangrado durante el periodo puede ser un signo de que esto ha sucedido. Informe a su médico o profesional sanitario si presenta cambios inesperados en su patrón de sangrado.
Retirada de Levosert
Levosert debe ser retirado o reemplazado después de 8 años de uso, o antes si reaparece el sangrado menstrual abundante o molesto.
Su médico puede retirar el sistema fácilmente en cualquier momento, después de lo cual es posible quedarse embarazada. Algunas mujeres se sienten mareadas o se desmayan durante o después de la retirada de Levosert. Puede experimentar algo de dolor y sangrado durante la retirada de Levosert.
Continuación de la anticoncepción después de la retirada
Si no desea quedarse embarazada, Levosert no debe ser retirado después del séptimo día del ciclo menstrual (periodo mensual) a menos que utilice otros métodos anticonceptivos (por ejemplo, preservativos) durante al menos 7 días antes de la retirada del SLI.
Si tiene periodos (menstruaciones) irregulares o no tiene periodos, debería utilizar un método anticonceptivo de barrera durante 7 días antes de la retirada.
También, un nuevo Levosert puede ser colocado inmediatamente después de la retirada, en cuyo caso no se necesita protección adicional. Si no desea continuar con el mismo método, pregunte a su médico sobre otros métodos anticonceptivos fiables.
Si tiene más preguntas sobre el uso de este medicamento, pregunte a su médico.
4. Posibles efectos adversos
Al igual que todos los medicamentos, este medicamento puede producir efectos adversos, aunque no todas las personas los sufran.
Con Levosert, los efectos adversos son más frecuentes durante los primeros meses tras haber colocado el sistema y van disminuyendo conforme pasa el tiempo.
Si usted experimenta alguno de los siguientes efectos adversos graves, por favor contacte con su médico o enfermero inmediatamente:
- Dolor intenso o fiebre que desarrolla poco tiempo después de la inserciónpuede significar que tiene una infección grave que debería tratarse inmediatamente. En raros casos puede ocurrir una infección muy grave (sepsis).
- Dolor intenso y sangrado continuadoya que esto puede ser un signo de daño o desgarro de la pared del útero (perforación). La perforación es poco frecuente, pero ocurre con mayor frecuencia durante la inserción de Levosert, aunque puede no detectarse hasta algún tiempo después. Si Levosert se ha alojado fuera de la cavidad del útero, no es efectivo para prevenir el embarazo y debe ser retirado lo antes posible; en muy raras ocasiones esto puede requerir cirugía. El riesgo de perforación es bajo, pero se incrementa en mujeres en periodo de lactancia o mujeres que han tenido un bebé hasta 36 semanas antes de la inserción y puede que incremente en mujeres con el útero fijo inclinado hacia atrás (útero en retroversión y fijo). Si sospecha que puede haber sufrido una perforación, busque inmediatamente asistencia médica y recuérdele que tiene insertado Levosert, especialmente si no fue la persona que se lo insertó.
Posibles signos y síntomas de la perforación pueden incluir:
- dolor intenso (como calambres menstruales) o más dolor del esperado
- sangrado abundante (tras la inserción)
- dolor o sangrado que continua más de unas pocas semanas
- cambios repentinos en los periodos
- dolor durante relaciones sexuales
- si ya no puede sentir los hilos de Levosert (ver “¿Cómo puedo saber si el sistema está en su lugar?” en la sección 3).
- Dolor en la parte baja del abdomen especialmente si también tiene fiebre o ha tenido una falta o tiene un sangrado inesperado,ya que esto puede ser un signo de embarazo ectópico (desarrollo del feto fuera del útero). El riesgo absoluto de embarazo ectópico en usuarias de Levosert es bajo. Sin embargo, cuando una mujer queda embarazada con Levosert dentro, la probabilidad de embarazo ectópico se incrementa.
- Dolor en la parte baja del abdomen o experimenta relaciones sexuales difíciles o dolorosas ya que puede ser un signo de quistes ováricos o enfermedad inflamatoria pélvica. Esto es importante ya que las infecciones pélvicas pueden reducir sus probabilidades de tener un bebé y pueden aumentar el riesgo de embarazo ectópico.
Otros efectos adversos
Muy frecuentes(pueden afectar a más de 1 de cada 10 mujeres) pueden incluir:
- ausencia de menstruaciones, ligeras o infrecuentes (véase "¿Cómo afectará Levosert One a mis menstruaciones?" en la sección 3.
- sangrado vaginal incluyendo manchado.
- infecciones vaginales o de los genitales externos (vulva) causadas por hongos o bacterias;
- granos (acné);
Frecuentes(pueden afectar hasta 1 de cada 10 mujeres) pueden incluir:
- depresión, nerviosismo u otros cambios de humor;
- apetito sexual reducido;
- cefalea;
- migraña;
- sensación de desmayo (presíncope);
- mareos;
- dolor de espalda;
- malestar abdominal;
- náuseas;
- abdomen hinchado;
- vómitos;
- periodos dolorosos;
- aumento del flujo vaginal;
- pechos sensibles y doloridos;
- relaciones sexuales dolorosas;
- espasmo del útero;
- Levosert se sale de su lugar;
- aumento de peso.
Poco frecuentes(pueden afectar hasta 1 de cada 100 mujeres) pueden incluir:
- desmayo;
- eczema;
- inflamación del cuello del útero (cervicitis);
- hinchazón o inflamación en piernas o tobillos;
- aumento del crecimiento de pelo en la cara y el cuerpo;
- pérdida de cabello;
- picazón en la piel (prurito);
- decoloración de la piel o aumento de pigmentación de la piel, especialmente en la cara (cloasma).
Raros(pueden afectar hasta 1 de cada 1.000 mujeres) pueden incluir:
- erupción cutánea, picores,
Comunicación de efectos adversos
Si experimenta cualquier tipo de efecto adverso, consulte a su médico o farmacéutico, incluso si se trata de posibles efectos adversos que no aparecen en este prospecto. También puede comunicarlos directamente a través del Sistema Español de Farmacovigilancia de Medicamentos de Uso Humano: https://www.notificaram.es. Mediante la comunicación de efectos adversos usted puede contribuir a proporcionar más información sobre la seguridad de este medicamento.
5. Conservación de Levosert
Conservar en el embalaje original. Mantenga la bolsa en la caja externa para protegerla de la luz. Mantener el envase perfectamente cerrado. Solo su médico o profesional sanitario pueden abrirlo.
Mantener este medicamento fuera de la vista y del alcance de los niños.
No utilice este sistema después de la fecha de caducidad que aparece en la etiqueta y en el envase exterior después de “CAD:”. La fecha de caducidad es el último día del mes que se indica.
Los medicamentos no se deben tirar por los desagües ni a la basura. Deposite los envases y los medicamentos que no necesita en el Punto SIGRE de la farmacia. En caso de duda pregunte a su farmacéutico cómo deshacerse de los envases y de los medicamentos que no necesita. De esta forma, ayudará a proteger el medio ambiente.
6. Contenido del envase e información adicional
Composición de Levosert
Levosert contiene 52 mg de levonorgestrel, el principio activo. La hormona viene dentro de una sustancia denominada polidimetilsiloxano. Esta sustancia está rodeada por una membrana que también está hecha de polidimetilsiloxano.
Aspecto del producto y contenido del envase
Levosert consta de un pequeño cuerpo en forma de T hecho de un plástico denominado polietileno. Esta estructura proporciona un dispositivo para liberar la hormona de forma gradual en el útero.
Hay dos hilos finos, hechos de polipropileno y de azul de ftalocianina de cobre, unidos al extremo inferior del armazón. Estos hilos permitirán una extracción sencilla y le permitirán a usted y a su médico comprobar que el dispositivo está en su lugar.
El SLI Levosert con el dispositivo de inserción se envasa individualmente en una bolsa despegable que está hecha de dos láminas: bolsa termoformada (poliéster) con tapa despegable.
Cada envase contiene uno o cinco Levosert en bolsa o bolsas despegables, que se envasan individualmente en una o cinco cajas individuales con el prospecto y la tarjeta recordatorio para la paciente.
Tamaño de los envases:
1 sistema de liberación intrauterino con dispositivo aplicador.
5 sistemas de liberación intrauterinos con dispositivo aplicador.
Multipack: cinco envases de un sistema de liberación intrauterino con un dispositivo aplicador.
Puede que solamente estén comercializados algunos tamaños de envases.
Titular de la autorización de comercialización
Gedeon Richter Plc.
Gyömroi út 19-21.
1103 Budapest
Hungría
Responsable de la fabricación
Odyssea Pharma SA
Rue du Travail 16
4460 Grâce Hollogne
Bélgica
Gedeon Richter Plc.
Gyömroi út 19-21.
1103 Budapest
Hungría
Pueden solicitar más información respecto a este medicamento dirigiéndose al representante local del titular de la autorización de comercialización:
Gedeon Richter Ibérica S.A.
Sabino Arana, 28 4º 2ª
08028 Barcelona
España
+34 93 2034300
Este medicamento está autorizado en los estados miembros del Espacio Económico Europeo y en el Reino Unido (Irlanda del Norte) con los siguientes nombres:
Alemania, Austria, Chipre, Malta, Noruega, Suecia | Levosert |
Dinamarca | Levosert Two |
Croacia | Levosert 20 mikrograma/24 sata intrauterini sustav |
España | Levosert 0,02 mg cada 24 horas sistema de liberación intrauterino |
Irlanda | Levosert 52 mg Intrauterine Delivery System |
Islandia | Levosert 20 míkrógrömm/24 klst.Leginnlegg |
Italia | Benilexa |
Reino Unido | Benilexa Two Handed |
Eslovenia | Levosert 20 mikrogramov/24 ur intrauterini dostavni sistem |
Fecha de la última revisión de este prospectojulio 2024
La información detallada y actualizada de este medicamento está disponible en la página Web de la Agencia Española de Medicamentos y Productos Sanitarios (AEMPS)http://www.aemps.gob.es/
Esta información está destinada únicamente a profesionales del sector sanitario
Consulte las instrucciones de uso y manipulación incluidas en el envase.
_____________________________________________________________________________
Instrucciones de uso y manipulación
Levosert 0,02mg cada 24horas sistema de liberación intrauterino
levonorgestrel
Esta información está destinada únicamente a profesionales del sector sanitario
Lista de comprobación para el profesional que prescribe
Hágase las siguientes preguntas antes de prescribir/insertar Levosert:
- ¿He comprobado que las necesidades de la paciente cumplen con las indicaciones de anticoncepción o sangrado menstrual abundante y con la duración de uso, de hasta ocho años?
- ¿He cumplimentado la tarjeta de la paciente incluida en el envase y se la he dado a la paciente como recordatorio? (toda inserción de más de ocho años de duración debe comunicarse como uso no autorizado)
Lea las siguientes instrucciones de uso atentamente, puesto que puede haber alguna diferencia en el tipo de dispositivo aplicador en comparación con otros DIU que haya usado anteriormente:
Instrucciones de inserción
Debe ser insertado por un profesional sanitario utilizando una técnica aséptica.
Se recomienda que Levosert solo debería ser insertado por profesionales sanitarios que estén experimentados en la colocación de sistemas de liberación intrauterina (SLI) y/o que hayan recibido formación suficiente sobre el procedimiento de inserción de Levosert y hayan leído atentamente estas instrucciones antes de la inserción de Levosert.
Levosert se suministra en un envase estéril que no debe abrirse hasta que sea necesario para su inserción. No reesterilizar. Para un solo uso. El producto expuesto debe manejarse con precauciones asépticas. Si se rompe el sellado del envase estéril, el producto debe desecharse (ver instrucciones de eliminación en la sección 6.6). No utilizar si el envase interno está dañado o abierto. No insertar después de la fecha de caducidad indicada en la caja y en el blíster después de CAD. La fecha de caducidad es el último día del mes que se indica.
Para conocer el momento de la inserción, consulte la sección 4.2 de la ficha técnica.
Levosert incluye dentro del envase una tarjeta recordatorio para la paciente. Completar la tarjeta recordatorio para la paciente y entregarla a la paciente después de la inserción.
Preparación para la inserción
- Examine a la paciente para descartar contraindicaciones para la inserción de Levosert (ver secciones 4.3 y 4.4 bajo Exploración médica).
- Coloque un espéculo, visualice el cuello uterino y, a continuación, haga una limpieza minuciosa del cuello uterino y la vagina con una solución antiséptica adecuada.
- El profesional sanitario puede contar con la colaboracion de personal auxiliar si lo considera necesario.
- Sujete el labio anterior del cuello uterino con unas pinzas tenáculo u otras pinzas para estabilizar el útero. Si el útero está en retroversión, puede ser más apropiado sujetar el labio posterior del cuello uterino. Se puede aplicar una ligera tracción con las pinzas para enderezar el canal cervical. Las pinzas deben permanecer en su posición y se debe mantener una tracción suave sobre el cuello uterino durante todo el procedimiento de inserción.
- Introducir una sonda uterina avanzadas a través del canal cervical hasta el fondo para medir la profundidad. Si la profundidad uterina es < 5,5 cm, interrumpir el procedimiento. Confirme la dirección de la cavidad uterina y excluya cualquier evidencia de anomalías intrauterinas (p. ej., septo, miomas submucosos) o un anticonceptivo intrauterino previamente insertado que no haya sido retirado. Si se encuentra dificultad, considere la dilatación del canal cervical. Si se requiere dilatación cervical, se debe considerar el uso de analgésicos y/o un bloqueo paracervical.
Descripción
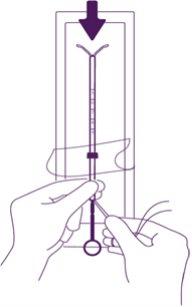
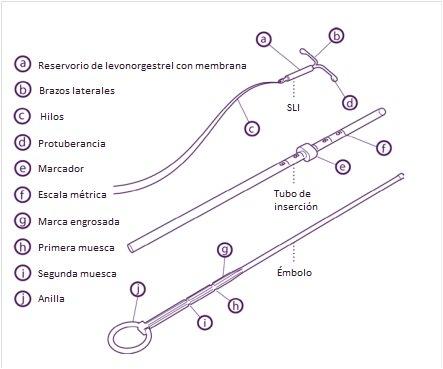
Figura 1 |
Preparación para la inserción
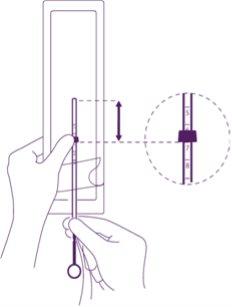
Figura 2 Figura 3
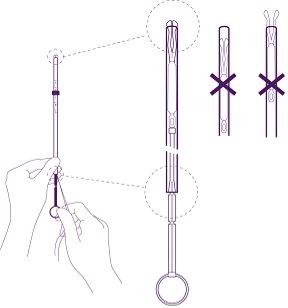
Figura 4 |
| Introduzca el émbolo y el SLI en el tubo de inserción Abra parcialmente el blíster (sobre 1/3 desde la parte inferior) e introduzca el émbolo en el tubo de inserción. Desenganche los hilos del marcador. Tire del hilo para introducir el SLI en el tubo. Los brazos del SLI deben quedar en un plano horizontal, paralelos al lado plano del marcador. |
Figura 5 | Coloque el borde inferior del marcador en el valor de la profundidad medida Coloque el borde inferior del marcador azul en el valor de la medición obtenida por histerometría. Los lados planos del marcador deben quedar siempre paralelos a los brazos. Esto permitirá que los brazos se abran correctamente en la cavidad uterina. | |
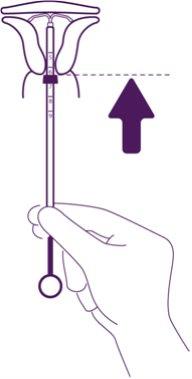
Inserción Figura 6 | Ajuste la posición del SLI en el tubo de inserción Sujete el émbolo con firmeza mientras tira del hilo y mueva el tubo para ajustar la posición del SLI. Las protuberancias de los brazos laterales deben estar contrapuestas, ligeramente por encima del extremo superior del tubo de inserción (ver imagen ampliada 1) y el borde distal del tubo debe estar alineado con la primera muesca del émbolo (ver imagen ampliada 2). Si el tubo no está alineado con la primera muesca del émbolo debe tirar del hilo con más firmeza. | |
Figura 7 | Introduzca el dispositivo en el canal cervical hasta que el marcador azul esté en contacto con el cérvix Saque todo el dispositivo del blíster, sujetando firmemente el émbolo y el tubo juntos en la posición ajustada correctamente. Introduzca el dispositivo en el canal cervical hasta que el marcador azul esté en contacto con el cérvix. | |
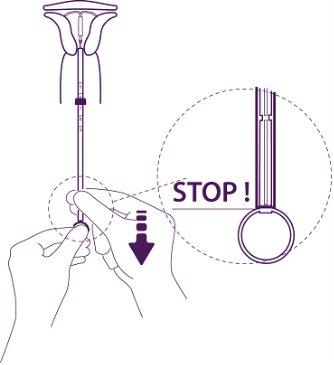
Figura 8 | Deje salir los brazos del sistema intrauterino Sujete el émbolo, suelte el hilo y tire del tubo de inserción hacia abajo hasta que su extremo inferior alcance la segunda muesca del émbolo. | |
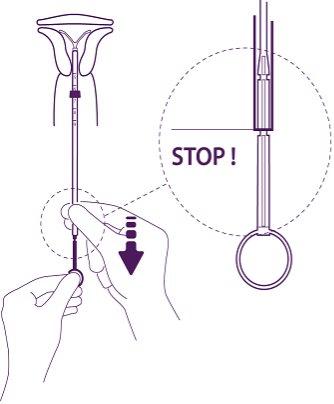
Figura 9 | Empuje el dispositivo contra el fundus uterino Para posicionar del SLI en la cavidad uterina, empuje el tubo de inserción simultáneamente con el émbolo, hasta que el marcador azul esté otra vez en contacto con el cérvix. Levosert estará entonces colocado correctamente en la cavidad uterina. | |
Figura 10 | Pase el SLI del tubo a la cavidad uterina Sin mover el émbolo, tire del tubo de inserción hacia abajo hasta la anilla del émbolo. Una ligera resistencia marca el paso por el engrosamiento del émbolo. No obstante, tire del tubo hacia abajo hasta la anilla del émbolo. El SLI estará entonces completamente liberado del tubo de inserción. | |
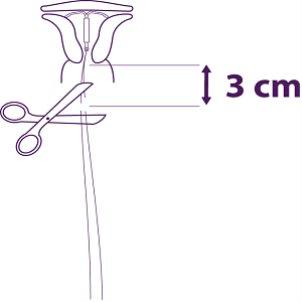
| Saque de forma secuencial los componentes del aplicador y corte los hilos Saque de forma secuencial primero el émbolo y luego el tubo de inserción. Corte los hilos a unos 3 cm del cérvix. |
La inserción de Levosert se ha completado.
Información importante a tener en cuenta durante o después de la inserción:
- Si sospecha que el SLI no está en la posición correcta:
- Compruebe la inserción con una ecografía u otra prueba radiológica adecuada.
- Si se sospecha que la inserción es incorrecta, retire el SLI. No vuelva a insertar el mismo SLI después de retirarlo.
¡IMPORTANTE!
En caso de una inserción difícil y/o de dolor o sangrado excepcionales durante o tras la inserción, se debe realizar una exploración física y una ecografía inmediatamente para descartar la perforación del cuerpo o cuello uterino. La exploración física por sí sola (incluida la comprobación de los hilos) puede no ser suficiente para excluir una perforación parcial. Si es necesario, extraiga el sistema e inserte un nuevo sistema estéril.
Después de la inserción, las mujeres deben ser reexaminadas al cabo de 4 a 6 semanas para comprobar los hilos y asegurar que el dispositivo está en la posición correcta. Informe sobre cualquier caso de perforación uterina o dificultades de inserción a través del Sistema Español de Farmacovigilancia de Medicamentos de Uso Humano: https://www.notificaram.es.
Retirada/sustitución
El SLI se extrae tirando con suavidad de los hilos con un fórceps. El uso de fuerza excesiva o instrumentos afilados durante la extracción puede provocar la rotura del sistema.
Si los hilos no son visibles y se descubre que el sistema está en la cavidad uterina en el examen de ultrasonido, se puede extraer usando unos fórceps estrechos. Esto puede requerir dilatación del canal cervical o intervención quirúrgica.
Después de la extracción del SLI, se debe examinar el sistema para comprobar que está intacto y que se ha retirado por completo. Durante las extracciones difíciles, se han notificado casos aislados en los que el cilindro de la hormona se ha deslizado sobre los brazos horizontales, escondiéndolos totalmente dentro del cilindro. Esta situación no requiere ninguna otra intervención una vez se haya comprobado que el SLI está completo. Las protuberancias de los brazos horizontales normalmente evitan la completa separación del cilindro del cuerpo en forma de T.
- País de registro
- Principio activo
- Requiere recetaSí
- Fabricante
- Esta información es de carácter general y no sustituye la consulta con un profesional sanitario.
- Alternativas a LEVOSERT 0,02 MG CADA 24 HORAS SISTEMA DE LIBERACION INTRAUTERINOForma farmacéutica: DISPOSITIVO INTRAUTERINO, 13,5 mg levonorgestrelPrincipio activo: plastic IUD with progestogenFabricante: Bayer Hispania S.L.Requiere recetaForma farmacéutica: DISPOSITIVO INTRAUTERINO, 19,5 mgPrincipio activo: plastic IUD with progestogenFabricante: Bayer Hispania S.L.Requiere recetaForma farmacéutica: DISPOSITIVO INTRAUTERINO, 0,02 mg/24 hPrincipio activo: plastic IUD with progestogenFabricante: Gedeon Richter Plc.Requiere receta
Médicos online para LEVOSERT 0,02 MG CADA 24 HORAS SISTEMA DE LIBERACION INTRAUTERINO
Comenta la dosis, los posibles efectos secundarios, interacciones, contraindicaciones o la revisión de receta de LEVOSERT 0,02 MG CADA 24 HORAS SISTEMA DE LIBERACION INTRAUTERINO, sujeto a valoración médica y a la normativa local.
Preguntas frecuentes