
LENALIDOMIDA SUN 5 MG CAPSULAS DURAS EFG


Cómo usar LENALIDOMIDA SUN 5 MG CAPSULAS DURAS EFG
Traducción generada por IA
Este contenido ha sido traducido automáticamente y se ofrece solo con fines informativos. No sustituye la consulta con un profesional sanitario.
Ver originalContenido del prospecto
Introducción
Prospecto: información para el usuario
Lenalidomida Sun 2,5 mg cápsulas duras EFG
Lenalidomida Sun 5 mg cápsulas duras EFG
Lenalidomida Sun 7,5 mg cápsulas duras EFG
Lenalidomida Sun 10 mg cápsulas duras EFG
Lenalidomida Sun 15 mg cápsulas duras EFG
Lenalidomida Sun 20 mg cápsulas duras EFG
Lenalidomida Sun 25 mg cápsulas duras EFG
lenalidomida
Lea todo el prospecto detenidamente antes de empezar a tomar este medicamento, porque contiene información importante para usted.
- Conserve este prospecto, ya que puede tener que volver a leerlo.
- Si tiene alguna duda, consulte a su médico o farmacéutico.
- Este medicamento se le ha recetado solamente a usted, y no debe dárselo a otras personas aunque tengan los mismos síntomas que usted, ya que puede perjudicarles.
- Si experimenta efectos adversos, consulte a su médico, o farmacéutico, incluso si se trata de efectos adversos que no aparecen en este prospecto. Ver sección 4.
Contenido del prospecto:
- Qué es Lenalidomida Sun y para qué se utiliza
- Qué necesita saber antes de empezar a tomar Lenalidomida Sun
- Cómo tomar Lenalidomida Sun
- Posibles efectos adversos
- Conservación de Lenalidomida Sun
- Contenido del envase e información adicional
1. Qué es Lenalidomida Sun y para qué se utiliza
Qué esLenalidomida Sun
Lenalidomida Sun contiene el principio activo “lenalidomida”. Este medicamento pertenece a un grupo de medicamentos que afectan a cómo funciona el sistema inmunitario.
Para qué se utilizaLenalidomida Sun
Lenalidomida se usa en adultos para:
- Mieloma múltiple
- Síndromes mielodisplásicos (SMD)
- Linfoma de células del manto (LCM)
- Linfoma folicular
Mieloma múltiple
El mieloma múltiple es un tipo de cáncer que afecta a un tipo concreto de glóbulos blancos de la sangre, que se llaman células plasmáticas. Estas células se acumulan en la médula ósea y se multiplican, pasando a estar fuera de control. Esto puede dañar los huesos y los riñones.
El mieloma múltiple por lo general no tiene cura. Sin embargo, se pueden reducir mucho los signos y síntomas o pueden desaparecer durante un periodo de tiempo. A esto se le llama “remisión”.
Mieloma de nuevo diagnóstico: en pacientes que se han sometido a un trasplante de médula ósea
Lenalidomida se utiliza como tratamiento de mantenimiento después de recuperarse de manera adecuada tras un trasplante de médula ósea.
Mieloma múltiple de nuevo diagnóstico: en pacientes que no se puedan tratar con un trasplante de médula ósea
Lenalidomida se toma con otros medicamentos, entre ellos:
- un medicamento de quimioterapia llamado “bortezomib”;
- un medicamento antiinflamatorio llamado “dexametasona”
- un medicamento de quimioterapia llamado “melfalán” y
- un inmunosupresor llamado “prednisona”.
Tomará estos medicamentos al comenzar el tratamiento y luego continuará tomando lenalidomida solo.
Si tiene 75 años o más o tiene problemas de riñón de moderados a graves, su médico le controlará cuidadosamente antes de iniciar el tratamiento.
Mieloma múltiple: en pacientes tratados anteriormente
Lenalidomida se toma junto con un antiinflamatorio llamado “dexametasona”.
Lenalidomida puede frenar el empeoramiento de los signos y síntomas del mieloma múltiple. También ha demostrado retrasar la reaparición del mieloma múltiple tras el tratamiento.
Síndromes mielodisplásicos (SMD)
Los SMD son un grupo de muchas enfermedades diferentes de la sangre y de la médula ósea. Las células de la sangre se vuelven anormales y no funcionan correctamente. Los pacientes pueden experimentar una variedad de signos y síntomas entre los que están un recuento bajo de glóbulos rojos (anemia), la necesidad de transfusión de sangre y el riesgo de infección.
Lenalidomida se utiliza para tratar a pacientes adultos diagnosticados de SMD, cuando todos los siguientes puntos sean aplicables:
- necesita transfusiones de sangre periódicamente para tratar los niveles bajos de glóbulos rojos (“anemia dependiente de transfusiones”);
- tiene una anomalía de las células de la médula ósea llamada “anomalía citogenética de deleción 5q aislada”. Esto significa que su cuerpo no produce un número suficiente de células sanguíneas sanas;
- otros tratamientos que ha utilizado anteriormente no son adecuados o no funcionan lo suficientemente bien.
Lenalidomida puede aumentar el número de glóbulos rojos sanos que produce el organismo al reducir el número de células anormales:
- esto puede reducir el número de transfusiones de sangre necesarias. Es posible que no se necesiten transfusiones.
Linfoma de células del manto (LCM)
El LCM es un cáncer de una parte del sistema inmunológico (el tejido linfático). Afecta a un tipo de glóbulos blancos de la sangre llamados “linfocitos B” o células B. El LCM es una enfermedad en la que las células B crecen sin control y se acumulan en el tejido linfático, la médula ósea o la sangre.
Lenalidomida se utiliza en monoterapia para tratar a pacientes adultos que han recibido tratamiento anteriormente con otros medicamentos.
Linfoma folicular (LF)
El LF es un cáncer de crecimiento lento que afecta a los linfocitos B. Estos son un tipo de glóbulos blancos que ayudan al organismo a combatir las infecciones. Cuando una persona sufre LF puede almacenar demasiados de estos linfocitos B en la sangre, la médula ósea, los nódulos linfáticos y el bazo.
Lenalidomida se utiliza con otro medicamento llamado “rituximab” para el tratamiento de pacientes adultos que han recibido tratamiento previo para el linfoma folicular.
Cómo actúaLenalidomida Sun
Lenalidomida actúa afectando al sistema inmunitario del organismo y atacando directamente al cáncer. Actúa de diversas formas:
- detiene el desarrollo de las células cancerosas;
- detiene el crecimiento de los vasos sanguíneos en el cáncer;
- estimula parte del sistema inmunitario para que ataque a las células cancerosas.
2. Qué necesita saber antes de empezar a tomar Lenalidomida Sun
Debe leer el prospecto de todos los medicamentos que vaya a tomar en combinación con Lenalidomida Sun antes de empezar el tratamiento con este medicamento.
No tomeLenalidomida Sun:
- si está embarazada, cree que podría estar embarazada o tiene intención de quedarse embarazada, ya que se espera que lenalidomida sea perjudicial para el feto(ver sección 2, “Embarazo, lactancia y anticoncepción: información para mujeres y hombres”).
- si puede quedarse embarazada, a menos que siga todas las medidas necesarias para evitarlo (ver sección 2, “Embarazo, lactancia y anticoncepción: información para mujeres y hombres”). Si puede quedarse embarazada, su médico anotará con cada receta que se han tomado todas las medidas necesarias y le proporcionará esta confirmación.
- si es alérgico a lenalidomida o a alguno de los demás componentes de este medicamento (incluidos en la sección 6). Si cree que puede ser alérgico, consulte a su médico.
Si alguna de estas condiciones es aplicable a usted, no tome lenalidomida. En caso de duda, consulte a su médico.
Advertencias y precauciones
Consulte a su médico, farmacéutico o enfermero antes de empezar a tomarLenalidomida Sunsi:
- ha tenido alguna vez coágulos de sangre; durante el tratamiento, tiene un mayor riesgo de presentar coágulos de sangre en las venas y en las arterias;
- tiene algún signo de infección, como tos o fiebre;
- tiene o ha tenido previamente una infección viral, especialmente infección por hepatitis B, varicela zóster o VIH. En caso de duda, consulte a su médico. El tratamiento con lenalidomida puede hacer que el virus se vuelva activo de nuevo, en los pacientes portadores del virus, dando lugar a la reaparición de la infección. Su médico debe comprobar si ha tenido alguna vez una infección por hepatitis B;
- tiene problemas de riñón; su médico puede ajustarle la dosis de lenalidomida;
- ha tenido un ataque al corazón, alguna vez ha tenido un coágulo de sangre, o si fuma, tiene la tensión arterial alta o los niveles de colesterol altos;
- ha tenido una reacción alérgica mientras utilizaba talidomida (otro medicamento que se utiliza para tratar el mieloma múltiple), como por ejemplo erupción cutánea, picor, hinchazón, mareos o problemas respiratorios;
- ha experimentado en el pasado una combinación de cualquiera de los síntomas siguientes: erupción generalizada, enrojecimiento de la piel, temperatura corporal alta, síntomas de tipo gripal, aumento de las enzimas hepáticas, anomalías en la sangre (eosinofilia) nódulos linfáticos engrosados (son síntomas de una reacción cutánea grave llamada reacción a fármaco con eosinofilia y síntomas sistémicos, que también se conoce como DRESS por sus siglas en inglés o síndrome de hipersensibilidad al fármaco) (ver también la sección 4 “Posibles efectos adversos”).
Si alguna de las alteraciones anteriores es aplicable a usted, informe a su médico, farmacéutico o enfermero antes de empezar el tratamiento.
En cualquier momento, durante o después del tratamiento, informe a su médico o enfermero inmediatamente si presenta:
- visión borrosa, pérdida de la visión o visión doble, dificultad para hablar, debilidad en un brazo o una pierna, un cambio en la forma de caminar o problemas de equilibrio, entumecimiento persistente, disminución de la sensibilidad o pérdida de sensibilidad, pérdida de memoria o confusión. Todos ellos pueden ser síntomas de una enfermedad cerebral grave y potencialmente mortal conocida como leucoencefalopatía multifocal progresiva (LMP). Si tiene alguno de estos síntomas antes de empezar el tratamiento con lenalidomida, informe a su médico si observa algún cambio en estos síntomas.
- falta de aire, cansancio, mareo, dolor en el pecho, latido cardíaco más rápido o hinchazón en las piernas o los tobillos. Estos pueden ser síntomas de una afección grave conocida como hipertensión pulmonar (ver sección 4).
Análisis y pruebas
Antes de iniciar el tratamiento con lenalidomida y durante el mismo, le harán análisis de sangre con regularidad, esto se debe a que lenalidomida puede causar una disminución de las células de la sangre que ayudan a luchar contra las infecciones (glóbulos blancos) y de las que participan en la coagulación (plaquetas).
Su médico le solicitará que le hagan un análisis de sangre:
- antes del tratamiento;
- cada semana, durante las 8 primeras semanas de tratamiento;
- posteriormente, por lo menos cada mes.
Puede que se le evalúe para detectar signos de problemas cardiopulmonares antes y durante el tratamiento con lenalidomida.
Para pacientes con SMD que tomen Lenalidomida Sun
Si tiene un SMD, puede ser más propenso a padecer una enfermedad más avanzada llamada leucemia mieloide aguda (LMA). Además, se desconoce cómo afecta lenalidomida a las posibilidades de que desarrolle LMA. Su médico, por tanto, le podrá hacer analíticas para detectar signos que puedan predecir mejor la posibilidad de que desarrolle LMA durante el tratamiento con lenalidomida.
Para pacientes con MCL que tomen Lenalidomida Sun
Su médico le solicitará que le hagan un análisis de sangre:
- antes del tratamiento;
- cada semana durante las primeras 8 semanas (2 ciclos) de tratamiento;
- a continuación, cada 2 semanas en los ciclos 3 y 4 (ver sección 3 “Ciclo de tratamiento” para obtener más información);
- después de esto se hará al comienzo de cada ciclo y
- al menos una vez al mes.
Para pacientes con LF que tomen Lenalidomida Sun
Su médico le solicitará que le hagan un análisis de sangre:
- antes del tratamiento;
- cada semana durante las primeras 3 semanas (1 ciclo) de tratamiento;
- a continuación, cada 2 semanas en los ciclos 2 a 4 (ver sección 3 “Ciclo de tratamiento” para obtener más información);
- después de esto se hará al comienzo de cada ciclo y
- al menos cada mes.
Su médico puede comprobar si tiene una cantidad total de tumor alta en el cuerpo, incluida la médula ósea. Esto podría dar lugar a una enfermedad en la que los tumores se descomponen y producen niveles inusuales de sustancias químicas en la sangre que, a su vez, pueden originar insuficiencia renal (esta enfermedad se llama “síndrome de lisis tumoral”).
Su médico puede examinarle para comprobar si se han producido cambios en su piel, tales como manchas rojas o erupciones cutáneas.
Su médico puede ajustar la dosis de lenalidomida o interrumpir su tratamiento, dependiendo de los resultados de sus análisis de sangre y de su estado general. Si es un paciente de nuevo diagnóstico, su médico puede evaluar también su tratamiento en función de su edad y de otras afecciones que ya tenga.
Donación de sangre
No debe donar sangre durante el tratamiento ni durante al menos 7 días después del final del tratamiento.
Niños y adolescentes
No está recomendado el uso de lenalidomida en niños y adolescentes menores de 18 años.
Personas de edad avanzada y personas con problemas renales
Si tiene 75 años o más o tiene problemas renales de moderados a graves, su médico le examinará detenidamente antes de iniciar el tratamiento.
Otros medicamentos y Lenalidomida Sun
Informe a su médico o enfermero si está tomando, ha tomado recientemente o pudiera tener que tomar cualquier otro medicamento. Esto se debe a que lenalidomida puede afectar a la forma en que funcionan otros medicamentos. Además, algunos medicamentos pueden afectar a la forma en que funciona lenalidomida.
En concreto, informe a su médico o enfermero si está tomando alguno de los siguientes medicamentos:
- algunos medicamentos que se utilizan para prevenir el embarazo, tales como los anticonceptivos orales, ya que pueden dejar de funcionar;
- algunos medicamentos que se utilizan para problemas de corazón, tales como la digoxina;
- algunos medicamentos que se utilizan para adelgazar la sangre, tales como la warfarina.
Embarazo, lactancia y anticoncepción: información para mujeres y hombres
Embarazo
Mujeres que toman Lenalidomida Sun
- No debe tomar lenalidomida si está embarazada, ya que se espera que sea perjudicial para el feto.
- No se debe quedar embarazada mientras toma lenalidomida. Por lo tanto, tiene que usar métodos anticonceptivos eficaces si existe la posibilidad de que pueda quedarse embarazada (ver “Anticoncepción”).
- Si se queda embarazada durante el tratamiento con lenalidomida, debe interrumpir el tratamiento e informar inmediatamente a su médico.
Hombres que toman Lenalidomida Sun
- Si su pareja se queda embarazada mientras usted toma lenalidomida, debe informar inmediatamente a su médico. Es recomendable que su pareja solicite consejo médico.
- Usted también debe utilizar métodos anticonceptivos efectivos (ver “Anticoncepción”).
Lactancia
No debe dar el pecho mientras tome lenalidomida, ya que se desconoce si lenalidomida pasa a la leche materna.
Anticoncepción
Para las mujeres que toman Lenalidomida Sun
Antes de comenzar el tratamiento, pregunte a su médico si tiene la capacidad de quedarse embarazada, aunque crea que esto es poco probable.
Si puede quedarse embarazada
- le harán pruebas de embarazo bajo supervisión médica (antes de cada tratamiento, al menos cada 4 semanas durante el tratamiento y durante al menos 4 semanas después de finalizar el tratamiento) excepto que se haya confirmado el cierre de las trompas de Falopio para que los óvulos no lleguen al útero (ligadura de trompas)
Y
- debe usar métodos anticonceptivos efectivos desde al menos 4 semanas antes de iniciar el tratamiento, durante el tratamiento y hasta al menos 4 semanas después de finalizar el tratamiento. Su médico le aconsejará sobre los métodos anticonceptivos más adecuados.
Para los hombres que toman Lenalidomida Sun
Lenalidomida pasa al semen humano. Si su pareja está embarazada o puede quedarse embarazada y no utiliza ningún método anticonceptivo eficaz, usted debe utilizar preservativos durante el tratamiento y hasta al menos 7 días después de finalizar el tratamiento, incluso si se ha sometido a una vasectomía. No debe donar semen ni esperma durante el tratamiento y durante al menos 7 días después de finalizar el tratamiento.
Conducción y uso de máquinas
No conduzca ni utilice máquinas si se siente mareado, cansado, adormilado, tiene vértigo o visión borrosa después de tomar lenalidomida.
Lenalidomida Sun contiene lactosa
Este medicamento contiene lactosa. Si su médico le ha dicho que tiene intolerancia a ciertos azúcares, consulte con él antes de tomar este medicamento.
3. Cómo tomar Lenalidomida Sun
Lenalidomida se la debe administrar un profesional sanitario con experiencia en el tratamiento del mieloma múltiple, SMD, LCM o LF.
- Cuando lenalidomida se utiliza para el tratamiento del mieloma múltiple en pacientes que no se pueden tratar con un trasplante de médula ósea o se han sometido a otros tratamientos antes, se toma con otros medicamentos (ver sección 1 “Para qué se utiliza Lenalidomida Sun”).
- Cuando lenalidomida se utiliza para el tratamiento del mieloma múltiple en pacientes que se han sometido a un trasplante de médula ósea o para tratar pacientes con SMD o LCM, se toma solo.
- Cuando lenalidomida se utiliza para el tratamiento del linfoma folicular, se toma con otro medicamento llamado “rituximab”.
Siga exactamente las instrucciones de administración de lenalidomida indicadas por su médico. En caso de duda, consulte a su médico o farmacéutico.
Si está tomando lenalidomida junto con otros medicamentos, debe consultar el prospecto de esos otros medicamentos para obtener información adicional sobre su uso y sus efectos.
Ciclo de tratamiento
Lenalidomida se toma ciertos días durante el periodo de 3 semanas (21 días).
- Un “ciclo de tratamiento” consta de 21 días.
- Dependiendo del día del ciclo, tomará uno o más medicamentos. Sin embargo, algunos días no tomará ningún medicamento.
- Después de terminar cada ciclo de 21 días, debe comenzar un nuevo “ciclo” durante los siguientes 21 días.
O
Lenalidomida se toma ciertos días durante el periodo de 4 semanas (28 días).
- Un “ciclo de tratamiento” consta de 28 días.
- Dependiendo del día del ciclo, tomará uno o más medicamentos. Sin embargo, algunos días no tomará ningún medicamento.
- Después de terminar cada ciclo de 28 días, debe comenzar un nuevo “ciclo” durante los siguientes 28 días.
Cuánto Lenalidomida Sun tomar
Antes de comenzar el tratamiento, su médico le indicará:
- qué cantidad de lenalidomida debe tomar;
- qué cantidad de los otros medicamentos debe tomar junto con lenalidomida, en su caso;
- qué días del ciclo de tratamiento debe tomar cada medicamento.
Cómo y cuándo tomar Lenalidomida Sun
- Trague las cápsulas enteras, preferiblemente con agua.
- No rompa, abra ni mastique las cápsulas. En el caso de que el polvo de una cápsula rota de lenalidomida entre en contacto con la piel, lave la piel de forma inmediata y cuidadosa con agua y jabón.
- Los profesionales sanitarios, cuidadores y familiares se deben poner guantes desechables cuando manipulen el blíster o la cápsula. Posteriormente, se deben quitar los guantes con cuidado para evitar la exposición cutánea, introducirlos en una bolsa de plástico de polietileno sellable y eliminarlos de acuerdo con los requisitos locales. A continuación, se deben lavar bien las manos con agua y jabón.
- Las mujeres embarazadas o que sospechen que puedan estarlo no deben manipular el blíster ni la cápsula.
- Las cápsulas pueden tomarse con o sin alimentos.
- Debe tomar lenalidomida aproximadamente a la misma hora en los días programados.
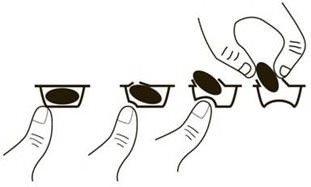
Toma de este medicamento
Para sacar la cápsula del blister:
- presione solo un extremo de la cápsula para que salga a través de la lámina.
- no presione en el centro de la cápsula ya que podría romperla.
Duración del tratamiento con Lenalidomida Sun
Lenalidomida se toma en ciclos de tratamiento, cada ciclo dura 21 o 28 días (ver “Ciclo de tratamiento” más arriba). Debe continuar los ciclos de tratamiento hasta que su médico le comunique que interrumpa el tratamiento.
Si toma más Lenalidomida Sun del que debe
Si toma más lenalidomida del que le han recetado, informe inmediatamente a su médico.
En caso de sobredosis o ingestión accidental, consulte inmediatamente a su médico o farmacéutico o llame al Servicio de Información Toxicológica, teléfono: 91 562 04 20, indicando el medicamento y la cantidad ingerida
Si olvidó tomar Lenalidomida Sun
Si olvida tomar lenalidomida a su hora habitual y
- han transcurrido menos de 12 horas: tome la cápsula inmediatamente.
- han transcurrido más de 12 horas: no tome la cápsula. Tome la próxima cápsula al día siguiente a la hora habitual.
Si tiene cualquier otra duda sobre el uso de este medicamento, pregunte a su médico o farmacéutico.
4. Posibles efectos adversos
Al igual que todos los medicamentos, este medicamento puede producir efectos adversos, aunque no todas las personas los sufran.
Si experimenta alguno de los siguientes efectos adversos graves, interrumpa el tratamiento con Lenalidomida Sun y acuda a un médico inmediatamente, porque podría requerir tratamiento médico de urgencia:
- Urticaria, erupciones, hinchazón de los ojos, boca o cara, dificultad para respirar o picor, que pueden ser síntomas de tipos graves de reacciones alérgicas llamadas angioedema y reacción anafiláctica.
- Reacción alérgica grave que puede comenzar como una erupción en una zona, pero se extiende produciendo una pérdida importante de piel por todo el cuerpo (síndrome de Stevens-Johnson y/o necrólisis epidérmica tóxica).
- Erupción generalizada, temperatura corporal alta, aumento de las enzimas hepáticas, anomalías en la sangre (eosinofilia), nódulos linfáticos engrosados y efectos sobre otros órganos del cuerpo (reacción al fármaco con eosinofilia y síntomas sistémicos, que también se conoce como síndrome DRESS o síndrome de hipersensibilidad al fármaco). Ver también sección 2.
Consulte inmediatamente a su médico si nota cualquiera de los siguientes efectos adversos graves:
- Fiebre, escalofríos, dolor de garganta, tos, úlceras bucales o cualquier otro síntoma de infección incluyendo en el torrente sanguíneo (sepsis).
- Hemorragia (sangrado) o hematoma (moratón) no debidos a una lesión.
- Dolor en el pecho (torácico) o en las piernas.
- Dificultad respiratoria.
- Dolor óseo, dolor muscular, confusión o cansancio que pueden deberse a niveles altos de calcio en la sangre.
Lenalidomida puede reducir el número de glóbulos blancos que combaten las infecciones y también de las células de la sangre que ayudan a coagular la sangre (plaquetas), lo que puede provocar trastornos hemorrágicos como sangrados de nariz y moratones. Lenalidomida también puede causar coágulos de sangre en las venas (trombosis).
Otros efectos adversos
Es importante señalar que un número reducido de pacientes puede desarrollar otros tipos de cáncer, y es posible que este riesgo aumente con el tratamiento con lenalidomida. Por lo tanto, su médico debe evaluar cuidadosamente los beneficios y los riesgos al recetarle lenalidomida.
Efectos adversos muy frecuentes(pueden afectar a más de 1 de cada 10 personas):
- Una disminución del número de glóbulos rojos lo que puede producir anemia que da lugar a cansancio y debilidad.
- Erupción cutánea, picor.
- Calambres musculares, debilidad muscular, dolor muscular, molestias musculares, dolor óseo, dolor de las articulaciones, dolor de espalda, dolor en las extremidades.
- Hinchazón generalizada que incluye hinchazón de los brazos y las piernas.
- Debilidad, cansancio.
- Fiebre y síntomas seudogripales que incluyen fiebre, dolor muscular, dolor de cabeza, dolor de oídos y escalofríos.
- Entumecimiento, hormigueo o sensación de escozor en la piel, dolores de manos o pies, mareos, temblor.
- Disminución del apetito, cambios en el sabor de las cosas.
- Aumento del dolor, tamaño del tumor o enrojecimiento alrededor del tumor.
- Pérdida de peso.
- Estreñimiento, diarrea, náuseas, vómitos, dolor de estómago, acidez de estómago.
- Niveles bajos de potasio o calcio y/o sodio en la sangre.
- Funcionamiento de la tiroides menor del que debería ser.
- Dolor de piernas (que podría ser un síntoma de trombosis), dolor de pecho o dificultad respiratoria (que podría ser un síntoma de coágulos de sangre en los pulmones, llamado embolia pulmonar).
- Infecciones de todo tipo, incluidas la infección de los senos paranasales que rodean la nariz (sinusitis), infección del pulmón y de las vías respiratorias altas.
- Dificultad respiratoria.
- Visión borrosa.
- Opacidad del ojo (cataratas).
- Problemas renales que incluyen riñones que no funcionan correctamente o que no son capaces de mantener un funcionamiento normal.
- Resultados anómalos en las pruebas hepáticas.
- Valores altos en los resultados de las pruebas hepáticas.
- Cambios en una proteína de la sangre que puede producir hinchazón de las arterias (vasculitis).
- Aumento de los niveles de azúcar en la sangre (diabetes).
- Disminución de los valores de azúcar en sangre.
- Dolor de cabeza.
- Sangrado nasal.
- Piel seca.
- Depresión, cambios en el estado de ánimo, dificultad para dormir.
- Tos.
- Bajada de la tensión arterial.
- Una sensación vaga de malestar en el cuerpo, sentirse mal.
- Inflamación dolorosa de la boca, sequedad de boca.
- Deshidratación.
Efectos adversos frecuentes(pueden afectar hasta 1 de cada 10 personas):
- Destrucción de glóbulos rojos (anemia hemolítica).
- Ciertos tipos de tumores de la piel.
- Sangrado de las encías, estómago o intestinos.
- Aumento de la tensión, latido cardiaco lento, rápido o irregular.
- Aumento de la cantidad de una substancia que se libera tras la destrucción normal o anormal de los glóbulos rojos.
- Aumento de un tipo de proteína que indica inflamación en el organismo.
- Oscurecimiento del color de la piel; cambio de color de la piel como resultado de un sangrado interno, normalmente causado por hematomas; inflamación de la piel causada por la acumulación de sangre; hematoma.
- Aumento del ácido úrico en la sangre.
- Erupciones cutáneas, enrojecimiento de la piel, piel agrietada, descamación o exfoliación de la piel, urticaria.
- Aumento de la sudoración, sudoración nocturna.
- Dificultad al tragar, dolor de garganta, dificultad para mantener la calidad de la voz o cambios en la voz.
- Goteo nasal.
- Fuerte aumento o disminución en la cantidad de orina frente a lo habitual o incapacidad de controlar la micción.
- Sangre en la orina.
- Dificultad respiratoria especialmente al tumbarse (que podría ser un síntoma de insuficiencia cardiaca).
- Dificultad para tener una erección.
- Ictus, desmayo, vértigo (trastorno del oído interno que provoca la sensación de que todo da vueltas), pérdida temporal del conocimiento.
- Dolor en el pecho que se extiende a brazos, cuello, mandíbula, espalda o estómago, sensación de sudoración y falta de aire, náuseas o vómitos, que pueden ser síntomas de un ataque al corazón (infarto de miocardio).
- Debilidad muscular, falta de energía.
- Dolor cervical, dolor en el pecho.
- Escalofríos.
- Hinchazón de las articulaciones.
- Flujo biliar del hígado más lento o bloqueado.
- Niveles bajos de fosfato o magnesio en la sangre.
- Dificultad para hablar.
- Daño hepático.
- Alteración del equilibrio, dificultad de movimientos.
- Sordera, pitidos en los oídos (tinnitus).
- Dolor en nervios, sensación anormal y desagradable, especialmente al tocar.
- Exceso de hierro en el organismo.
- Sed.
- Confusión.
- Dolor dental.
- Caída que puede causar lesiones.
Efectos adversos poco frecuentes(pueden afectar hasta 1 de cada 100 personas):
- Hemorragia en el interior del cráneo.
- Problemas circulatorios.
- Pérdida de la visión.
- Pérdida del deseo sexual (libido).
- Expulsión de grandes cantidades de orina con dolor de huesos y debilidad, que pueden ser síntomas de un trastorno renal (síndrome de Fanconi).
- Pigmentación amarilla en la piel, en las mucosas o en los ojos (ictericia), heces de color pálido, orina de color oscuro, picor de piel, erupción cutánea, dolor o hinchazón del estómago; éstos pueden ser síntomas de daño en el hígado (insuficiencia hepática).
- Dolor de estómago, hinchazón abdominal o diarrea, que pueden ser síntomas de una inflamación del intestino grueso (llamada colitis o tiflitis).
- Daño en las células de los riñones (llamado necrosis rubular renal).
- Cambios en el color de la piel, sensibilidad a la luz solar.
- Síndrome de lisis tumoral – se pueden producir complicaciones metabólicas durante el tratamiento del cáncer y algunas veces incluso sin tratamiento. Estas complicaciones se producen como consecuencia de los productos de descomposición de las células tumorales que mueren y pueden incluir: cambios en la bioquímica sanguínea, niveles altos de potasio, fósforo, ácido úrico y niveles bajos de calcio que, por tanto, generan cambios en la función renal y el ritmo cardiaco, crisis convulsivas y, algunas veces, la muerte.
- Aumento de la presión arterial dentro de los vasos sanguíneos que irrigan los pulmones (hipertensión pulmonar).
Efectos adversos de frecuencia no conocida(no puede estimarse a partir de los datos disponibles):
- Dolor repentino, o leve que empeora en la parte superior del estómago y/o espalda, que dura varios días, posiblemente acompañado de náuseas, vómitos, fiebre y un pulso rápido. Estos síntomas pueden deberse a una inflamación del páncreas.
- Silbidos o pitidos al respirar, dificultad respiratoria o tos seca, que pueden ser síntomas causados por una inflamación del tejido de los pulmones.
- Se han observado casos raros de degradación muscular (dolor, debilidad o hinchazón muscular) que pueden dar lugar a problemas de riñón (rabdomiólisis), algunos de ellos cuando se administra lenalidomida con una estatina (un tipo de medicamento para reducir el colesterol).
- Una enfermedad que afecta a la piel producida por la inflamación de los vasos sanguíneos pequeños, acompañada de dolor en las articulaciones y fiebre (vasculitis leucocitoclástica).
- Rotura de la pared del estómago o del intestino. Esto puede dar lugar a una infección muy grave. Informe a su médico si tiene dolor de estómago fuerte, fiebre, náuseas, vómitos, sangre en las heces o cambios en los hábitos intestinales.
- Infecciones virales, que incluyen herpes zóster (también conocido como la “culebrilla”, una enfermedad viral que produce una erupción cutánea dolorosa con ampollas) y la reaparición de la infección por hepatitis B (que puede producir un amarilleamiento de la piel y de los ojos, orina de color marrón oscuro, dolor de estómago en el lado derecho, fiebre y náuseas o sensación de estar enfermo).
- Rechazo de trasplante de órganos sólidos (tales como riñón, corazón).
Comunicación de efectos adversos
Si experimenta cualquier tipo de efecto adverso, consulte a su médico, farmacéutico o enfermero, incluso si se trata de posibles efectos adversos que no aparecen en este prospecto. También puede comunicarlos directamente a través del Sistema Español de Farmacovigilancia de medicamentos de Uso Humano: https://www.notificaram.es. Mediante la comunicación de efectos adversos usted puede contribuir a proporcionar más información sobre la seguridad de este medicamento.
5. Conservación de Lenalidomida Sun
- Mantener este medicamento fuera de la vista y del alcance de los niños.
- No utilice este medicamento después de la fecha de caducidad que aparece en el blíster y la caja después de “CAD”/“EXP”. La fecha de caducidad es el último día del mes que se indica.
- Conservar por debajo de 25ºC.
- No utilice este medicamento si observa indicios visibles de deterioro o signos de manipulación indebida.
- Los medicamentos no se deben tirar por los desagües ni a la basura. Devuelva a su farmacéutico el medicamento sin usar, de esta forma ayudará a proteger el medio ambiente.
6. Contenido del envase e información adicional
Composición de Lenalidomida Sun
Lenalidomida Sun 2,5/ 10/ 20 mg cápsulas duras EFG:
- El principio activo es lenalidomida. Cada cápsula contiene 2,5 / 10/ 20 mg de lenalidomida, respectivamente.
- Los demás componentes son:
- Contenido de las cápsulas: lactosa monohidrato (ver sección 2), celulosa microcristalina, croscarmelosa sódica y estearato de magnesio.
- Cubierta de la cápsula: dióxido de titanio (E171), carmín índigo (E132), gelatina y óxido de hierro amarillo (E172).
- Tinta de impresión: goma laca, óxido de hierro negro (E172) e hidróxido de potasio.
Lenalidomida Sun 5/ 25 mg cápsulas duras EFG:
- El principio activo es lenalidomida. Cada cápsula contiene 5/ 25 mg de lenalidomida, respectivamente.
- Los demás componentes son:
- Contenido de las cápsulas: lactosa monohidrato (ver sección 2), celulosa microcristalina, croscarmelosa sódica y estearato de magnesio.
- Cubierta de la cápsula: dióxido de titanio (E171), gelatina.
- Tinta de impresión: goma laca, óxido de hierro negro (E172) e hidróxido de potasio.
Lenalidomida Sun 7,5 mg cápsulas duras EFG:
- El principio activo es lenalidomida. Cada cápsula contiene 7,5 mg de lenalidomida.
- Los demás componentes son:
- Contenido de las cápsulas: lactosa monohidrato (ver sección 2), celulosa microcristalina, croscarmelosa sódica y estearato de magnesio.
- Cubierta de la cápsula: dióxido de titanio (E171), gelatina y óxido de hierro amarillo (E172).
- Tinta de impresión: goma laca, óxido de hierro negro (E172) e hidróxido de potasio.
Lenalidomida Sun 15 mg cápsulas duras EFG:
- El principio activo es lenalidomida. Cada cápsula contiene 15 mg de lenalidomida.
- Los demás componentes son:
- Contenido de las cápsulas: lactosa monohidrato (ver sección 2), celulosa microcristalina, croscarmelosa sódica y estearato de magnesio.
- Cubierta de la cápsula: dióxido de titanio (E171), carmín índigo (E132), gelatina.
- Tinta de impresión: goma laca, óxido de hierro negro (E172) e hidróxido de potasio.
Aspecto del producto y contenido del envase
Lenalidomida Sun 2,5 mg cápsulas duras EFG son cápsulas duras de gelatina de 14 mm de longitud, con tapa azul verdosa opaca y cuerpo blanco opaco, impresas con “RL” en la tapa y “78” en el cuerpo, y que contienen un polvo granular de blanco a blanquecino.
Lenalidomida Sun 5 mg cápsulas duras EFG son cápsulas duras de gelatina de 18 mm de longitud, con tapa y cuerpo blanco opacos, impresas con “RL” en la tapa y “79” en el cuerpo, y que contienen un polvo granular de blanco a blanquecino.
Lenalidomida Sun 7,5 mg cápsulas duras EFG son cápsulas duras de gelatina de 18 mm de longitud, con tapa amarillo pálido opaca y cuerpo blanco opaco, impresas con ”RL” en la tapa y “86” en el cuerpo, y que contienen un polvo granular de blanco a blanquecino.
Lenalidomida Sun 10 mg cápsulas duras EFG son cápsulas duras de gelatina de 21 mm de longitud, con tapa azul verdoso opaca y cuerpo amarillo pálido opaco, impresas con “RL” en la tapa y “80” en el cuerpo, y que contienen un polvo granular de blanco a blanquecino.
Lenalidomida Sun 15 mg cápsulas duras EFG son cápsulas duras de gelatina de 21 mm de longitud, con tapa azul opaca y cuerpo blanco opaco, impresas con “RL” en la tapa y “81” en el cuerpo, y que contienen un polvo granular de blanco a blanquecino.
Lenalidomida Sun 20 mg cápsulas dura EFG son cápsulas duras de gelatina de 21 mm de longitud, con tapa azul verdoso opaca y cuerpo azul opaco, impresas con “RL” en la tapa y “82” en el cuerpo, y que contienen un polvo granular de blanco a blanquecino.
Lenalidomida Sun 25 mg cápsulas duras EFG son cápsulas duras de gelatina de 21 mm de longitud, con tapa blanca opaca y cuerpo blanco opaco, impresas con “RL” en la tapa y “83” en el cuerpo, y que contienen un polvo granular de blanco a blanquecino.
Lenalidomida Sun 2,5 mg/5 mg/7,5 mg/10 mg/15 mg/20 mg/25 mg cápsulas duras EFG se disponen en envases que contienen 7, 14, 21, 28 o 42 cápsulas.
Lenalidomida Sun 2,5 mg/5 mg/7,5 mg/10 mg/15 mg/20 mg/25 mg cápsulas duras EFG se disponen en envases que contienen 7 x 1, 14 x 1, 21 x 1, 28 x 1 o 42 x 1 cápsulas.
Puede que solamente estén comercializados algunos tamaños de envases.
Titular de la autorización de comercialización
Sun Pharmaceutical Industries Europe B.V.
Polarisavenue 87
2132JH Hoofddorp
Países Bajos
Responsable de la fabricación
Sun Pharmaceutical Industries Europe B.V.
Polarisavenue 87
2132JH Hoofddorp
Países Bajos
Terapia S.A.
124 Fabricii Street
400 632 Cluj Napoca,
Rumanía
Pueden solicitar más información respecto a este medicamento dirigiéndose al representante local del titular de la autorización de comercialización:
Sun Pharma Laboratorios, S.L.
Rambla de Catalunya 53-55
08007 Barcelona
España
+34 93 342 78 90
Fecha de la última revisión de este prospecto:Enero 2024
Otras fuentes de información
La información detallada de este medicamento está disponible en la página web de la Agencia Europea de Medicamentos: https://www.aemps.gob.es/.
- País de registro
- Principio activo
- Requiere recetaSí
- Fabricante
- Esta información es de carácter general y no sustituye la consulta con un profesional sanitario.
- Alternativas a LENALIDOMIDA SUN 5 MG CAPSULAS DURAS EFGForma farmacéutica: CAPSULA, 10 mgPrincipio activo: LenalidomidaFabricante: Accord Healthcare S.L.U.Requiere recetaForma farmacéutica: CAPSULA, 15 mgPrincipio activo: LenalidomidaFabricante: Accord Healthcare S.L.U.Requiere recetaForma farmacéutica: CAPSULA, 2,5 mgPrincipio activo: LenalidomidaFabricante: Accord Healthcare S.L.U.Requiere receta
Médicos online para LENALIDOMIDA SUN 5 MG CAPSULAS DURAS EFG
Comenta la dosis, los posibles efectos secundarios, interacciones, contraindicaciones o la revisión de receta de LENALIDOMIDA SUN 5 MG CAPSULAS DURAS EFG, sujeto a valoración médica y a la normativa local.
Preguntas frecuentes






