HUMIRA 80 MG SOLUCION INYECTABLE EN PLUMA PRECARGADA


Cómo usar HUMIRA 80 MG SOLUCION INYECTABLE EN PLUMA PRECARGADA
Traducción generada por IA
Este contenido ha sido traducido automáticamente y se ofrece solo con fines informativos. No sustituye la consulta con un profesional sanitario.
Ver originalContenido del prospecto
Introducción
Prospecto: Información para el paciente
Humira 80mg solución inyectable en pluma precargada
adalimumab
Lea todo el prospecto detenidamente antes de empezar a usar este medicamento, porque contiene información importante para usted.
- Conserve este prospecto, ya que puede tener que volver a leerlo.
- Su médico le dará una tarjeta de información para el paciente,que contiene información de seguridad importante que necesita conocer antes y durante el tratamiento con Humira. Conserve esta tarjeta de información para el paciente.
- Si tiene alguna duda, consulte a su médico o farmacéutico.
- Este medicamento se le ha recetado solamente a usted y no debe dárselo a otras personas, aunque tengan los mismos síntomas que usted, ya que puede perjudicarles.
- Si experimenta efectos adversos, consulte a su médico o farmacéutico, incluso si se trata de efectos adversos que no aparecen en este prospecto. Ver sección 4.
Contenido del prospecto
- Qué es Humira y para qué se utiliza
- Qué necesita saber antes de empezar a usar Humira
- Cómo usar Humira
- Posibles efectos adversos
- Conservación de Humira
- Contenido del envase e información adicional
- Cómo inyectar Humira
1. Qué es Humira y para qué se utiliza
Humira contiene como sustancia activa adalimumab.
Humira se usa para tratar
- Artritis reumatoide
- Psoriasis en placas
- Hidradenitis supurativa
- Enfermedad de Crohn
- Colitis ulcerosa
- Uveitis no infecciosa
La sustancia activa de Humira, adalimumab, es un anticuerpo monoclonal humano. Los anticuerpos monoclonales son proteínas que atacan a una diana específica.
La diana de adalimumab es una proteína llamada factor de necrosis tumoral (TNFα), que interviene en el sistema inmune (defensa) y se encuentra en niveles elevados en las enfermedades inflamatorias descritas arriba. Mediante el ataque al TNFα, Humira disminuye el proceso de inflamación en esas enfermedades.
Artritis reumatoide
La artritis reumatoide es una enfermedad inflamatoria de las articulaciones.
Humira se utiliza para tratar la artritis reumatoide de moderada a grave en adultos. Puede que se le administren antes otros medicamentos modificadores de la enfermedad tales como metotrexato. En caso de que la respuesta a estos medicamentos no sea suficiente, se le administrará Humira.
Humira también puede usarse en el tratamiento de la artritis reumatoide grave, activa y progresiva sin tratamiento previo con metotrexato.
Humira puede reducir el daño de las articulaciones producido por la enfermedad inflamatoria y puede ayudar a que se muevan con más libertad.
Su médico decidirá si Humira debe utilizarse con metotrexato o en monoterapia.
Psoriasis en placas
La psoriasis en placas es una enfermedad de la piel que causa áreas enrojecidas, escamosas, con costras y cubiertas por escamas plateadas. La psoriasis en placas también puede afectar las uñas, provocando que se deterioren, se engrosen y se levanten del lecho de la uña, lo cual puede ser doloroso.
Humira se utiliza para tratar la psoriasis en placas crónica de moderada a grave en adultos.
Hidradenitis supurativa
La hidradenitis supurativa (a veces denominada acné inverso) es una enfermedad inflamatoria de la piel, crónica y a menudo dolorosa. Los síntomas pueden incluir nódulos sensibles (bultos) y abscesos (forúnculos) que pueden secretar pus. Normalmente afecta a áreas específicas de la piel, como debajo del pecho, de las axilas, zona interior de los muslos, ingle y nalgas. También puede haber cicatrices en las áreas afectadas.
Humira se utiliza para tratar
- la hidradenitis supurativa de moderada a grave en adultos y
- la hidradenitis supurativa de moderada a grave en adolescentes desde 12 a 17 años.
Humira puede reducir el número de nódulos y abscesos provocados por la enfermedad y el dolor que normalmente va asociado a esta enfermedad. Puede haber recibido otros medicamentos previamente. Si no responde lo suficientemente bien a esos medicamentos, recibirá Humira.
Enfermedad de Crohn
La enfermedad de Crohn es una enfermedad inflamatoria del tracto digestivo.
Humira se utiliza para tratar
- la enfermedad de Crohn de moderada a grave en adultos y
- la enfermedad de Crohn de moderada a grave en niños y adolescentes desde 6 a 17 años.
Puede haber recibido otros medicamentos previamente. Si no responde lo suficientemente bien a esos medicamentos, se le administrará Humira.
Colitis ulcerosa
La colitis ulcerosa es una enfermedad inflamatoria del intestino grueso.
Humira se utiliza para tratar
- la colitis ulcerosa de moderada a grave en adultos y
- la colitis ulcerosa de moderada a grave en niños y adolescentes desde los 6 hasta los 17 años
Puede haber recibido otros medicamentos previamente. Si no responde lo suficientemente bien a esos medicamentos, se le administrará Humira.
Uveítis no infecciosa
La uveítis no infecciosa es una enfermedad inflamatoria que afecta a ciertas partes del ojo.
Humira se utiliza para tratar
- adultos con uveítis no infecciosa con inflamación que afecta a la parte posterior del ojo.
- niños desde los 2 años de edad con uveítis crónica no infecciosa con inflamación que afecta a la parte frontal del ojo.
Esta inflamación puede conducir a una disminución de la visión y/o la presencia de motas en el ojo (puntos negros o líneas delgadas que se mueven a lo largo del campo de visión). Humira actúa reduciendo esta inflamación. Puede haber recibido otros medicamentos previamente. Si no responde lo suficientemente bien a esos medicamentos, se le administrará Humira.
2. Qué necesita saber antes de empezar a usar Humira
No use Humira:
- Si es alérgico a adalimumab o a alguno de los demás componentes de este medicamento (incluidos en la sección 6).
- Si padece tuberculosis activa u otras infecciones graves (ver “Advertencias y precauciones”). En caso de tener síntomas de cualquier infección, por ejemplo: fiebre, heridas, cansancio, problemas dentales, es importante que informe a su médico.
- Si padece insuficiencia cardiaca moderada o grave. Es importante que le diga a su médico si ha tenido o tiene algún problema cardiaco serio (ver “Advertencias y precauciones”).
Advertencias y precauciones
Consulte a su médico o farmacéutico antes de empezar a usar Humira.
Reacciones alérgicas
- Si notase una reacción alérgica con síntomas como opresión en el pecho, dificultad para respirar, mareo, hinchazón o sarpullido, interrumpa la administración de Humira y póngase en contacto con su médico inmediatamente ya que, en casos raros, estas reacciones pueden poner en peligro la vida.
Infecciones
- Si padece cualquier infección, incluyendo las crónicas, o una infección localizada en alguna parte del cuerpo (por ejemplo, una úlcera en la pierna) consulte a su médico antes de comenzar el tratamiento con Humira. Si no está seguro, póngase en contacto con su médico.
- Con el tratamiento con Humira podría contraer infecciones con más facilidad. Este riesgo puede ser mayor si tiene dañados los pulmones. Estas infecciones pueden ser graves e incluyen:
- tuberculosis
- infecciones causadas por virus, hongos, parásitos o bacterias
- infección grave en la sangre (sepsis)
En casos raros, estas infecciones podrían poner en peligro su vida. Por esta razón es importante que en el caso de que tenga síntomas como fiebre, heridas, cansancio o problemas dentales, se lo diga a su médico. Su médico le puede indicar que deje de utilizar Humira durante algún tiempo.
- Informe a su médico si reside o viaja por regiones donde las infecciones por hongos (por ejemplo: histoplasmosis, coccidioidomicosis o blastomicosis) son muy frecuentes.
- Informe a su médico si ha tenido infecciones recurrentes u otras enfermedades que aumentan el riesgo de contraer infecciones.
- Si tiene más de 65 años, puede ser más propenso a contraer infecciones durante el tratamiento con Humira. Usted y su médico deben prestar especial atención a los signos de infección mientras esté recibiendo tratamiento con Humira. Es importante que informe a su médico si presenta síntomas de infección, como fiebre, heridas, cansancio o problemas dentales.
Tuberculosis
- Es muy importante que informe a su médico si alguna vez ha sufrido tuberculosis o si ha estado en contacto directo con alguna persona que la haya padecido. Si tiene tuberculosis activa, no debe utilizar Humira.
- Dado que se han descrito casos de tuberculosis en pacientes en tratamiento con Humira, su médico le examinará en busca de signos o síntomas de tuberculosis antes de comenzar su tratamiento con Humira. Esto incluirá la realización de una evaluación médica minuciosa, incluyendo su historia médica y las pruebas apropiadas de diagnóstico (por ejemplo radiografía de tórax y la prueba de la tuberculina). La realización y resultados de estas pruebas debe anotarse en su tarjeta de información para el paciente.
- Se puede desarrollar tuberculosis durante el tratamiento incluso si usted ha recibido el tratamiento para prevenir la tuberculosis.
- Si apareciesen síntomas de tuberculosis (como por ejemplo: tos que no remite, pérdida de peso, falta de energía, febrícula), o de cualquier otra infección durante o una vez finalizado el tratamiento, póngase en contacto inmediatamente con su médico.
Hepatitis B
- Informe a su médico si es usted portador del virus de la hepatitis B (VHB), si ha tenido infecciones activas con VHB activo o si piensa que podría correr riesgo de contraer el VHB.
- Su médico le debe realizar un análisis para el VHB. En personas portadoras del VHB, Humira puede hacer que este virus se vuelva activo otra vez.
- En casos raros, especialmente si esta tomando otros medicamentos que suprimen el sistema inmune, la reactivación del VHB puede poner en peligro su vida.
Cirugía o intervención dental
- Si le van a realizar una intervención quirúrgica o dental, por favor informe a su médico de que está tomando Humira. Su médico le puede recomendar que interrumpa temporalmente el tratamiento con Humira.
Enfermedad desmielinizante
- Si padece o desarrolla una enfermedad desmielinizante (una enfermedad que afecta a la capa de aislamiento alrededor de los nervios, como la esclerosis múltiple),, su médico decidirá si debe ser tratado o continuar en tratamiento con Humira. Informe inmediatamente a su médico si experimenta síntomas tales como cambios en la visión, debilidad en brazos o piernas o entumecimiento u hormigueo en cualquier parte del cuerpo.
Vacunas
- Ciertas vacunas pueden causar infecciones y no deben administrarse si se está en tratamiento con Humira.
- Consulte con su médico antes de la administración de cualquier tipo de vacuna.
- Si es posible, se recomienda que reciba las vacunas previstas para su edad antes de iniciar el tratamiento con Humira.
- Si recibe Humira mientras esta embarazada, su hijo puede tener un riesgo mayor de sufrir infecciones durante aproximadamente los cinco meses siguientes a la última dosis de Humira que haya recibido durante su embarazo. Es importante que informe a su médico y a otros profesionales sanitarios sobre su uso de Humira durante el embarazo, para que ellos puedan decidir cuándo debe recibir alguna vacuna.
Insuficiencia cardiaca
- Si tiene insuficiencia cardiaca leve y está en tratamiento con Humira, puede ser monitorizado estrechamente por su médico. Es importante que le diga a su médico si ha tenido o tiene problemas cardíacos graves. Si desarrolla síntomas nuevos o empeoran sus síntomas (dificultad al respirar, o hinchazón de sus pies), debe ponerse en contacto con su médico inmediatamente. Su médico decidirá si debe seguir tomando Humira.
Fiebre, hematomas, sangrado o aspecto pálido
- En algunos pacientes, el organismo puede ser incapaz de producir un número suficiente del tipo de células sanguíneas que ayudan al cuerpo a luchar contra las infecciones o de las que contribuyen a parar las hemorragias. Su médico puede decidir si interrumpe el tratamiento. Si desarrolla fiebre persistente, ligeros hematomas o sangra fácilmente o su aspecto es pálido, llame a su médico inmediatamente
Cáncer
- En muy raras ocasiones se han dado casos de ciertos tipos de cáncer en niños y adultos tratados con Humira u otros agentes que bloquean el TNF.
- Las personas con artritis reumatoide de grados más graves y que padezcan la enfermedad desde hace mucho tiempo pueden tener un riesgo mayor que la media de desarrollar un linfoma (un cáncer que afecta al sistema linfático) y leucemia (un cáncer que afecta a la sangre y a la médula ósea).
- Si está en tratamiento con Humira el riesgo de padecer linfoma, leucemia u otros tipos de cáncer puede incrementarse. Se ha observado, en raras ocasiones, un tipo de linfoma poco frecuente y grave en pacientes en tratamiento con Humira. Algunos de estos pacientes recibían tratamiento también con azatioprina o 6- mercaptopurina.
- Informe a su médico si está tomando azatioprina o 6-mercaptopurina con Humira.
- Se han observado casos de cáncer de piel de tipo no melanoma en pacientes que usan Humira.
- Informe a su médico si durante o después del tratamiento aparecen nuevas lesiones en su piel o si las lesiones existentes cambian de apariencia.
- Se han registrado cánceres, diferentes del linfoma, en pacientes con una determinada enfermedad pulmonar, denominada Enfermedad Pulmonar Obstructiva Crónica (EPOC), tratados con otro agente bloqueante del TNF. Si tiene EPOC, o fuma mucho, debe consultar a su médico si el tratamiento con un bloqueante del TNF es adecuado en su caso.
Enfermedad autoinmune
- En raras ocasiones el tratamiento con Humira podría dar lugar a un síndrome similar al lupus. Contacte con su médico si tiene síntomas como erupción persistente sin explicación, fiebre, dolor de las articulaciones o cansancio.
Niños y adolescentes
- Vacunas: si es posible, su hijo debe ponerse al día con todas las vacunas antes de usar Humira.
Uso de Humira con otros medicamentos
Informe a su médico o farmacéutico si está tomando, ha tomado recientemente o pudiera tener que tomar cualquier otro medicamento.
No debe utilizar Humira junto con medicamentos que contengan los siguientes principios activos debido a un incremento del riesgo de infecciones graves:
- anakinra
- abatacept.
Humira se puede tomar junto con:
- metotrexato
- ciertos medicamentos antirreumáticos modificadores de la enfermedad (como por ejemplo: sulfasalazina, hidroxicloroquina, leflunomida y preparaciones inyectables a base de sales de oro)
- esteroides o medicamentos para el dolor, incluidos los antiinflamatorios no esteroideos (AINEs).
Si tiene alguna duda, consulte a su médico.
Embarazo y lactancia
- Debe considerar el uso de métodos anticonceptivos adecuados para evitar quedarse embarazada y continuar con su uso durante al menos 5 meses después del último tratamiento con Humira.
- Si está embarazada, cree que podría estar embarazada o tiene intención de tener un bebé, pida consejo a su médico sobre el uso de este medicamento.
- Humira debe usarse durante el embarazo solo si es necesario.
- Según un estudio en embarazo, no hubo un mayor riesgo de defectos congénitos cuando la madre había recibido tratamiento con Humira durante el embarazo comparado con las madres con la misma enfermedad que no recibieron tratamiento con Humira.
- Humira puede usarse durante la lactancia.
- Si utiliza Humira mientras está embarazada, su hijo puede tener un riesgo más alto de contraer una infección.
- Es importante que informe al pediatra y a otros profesionales sanitarios sobre el uso de Humira durante el embarazo antes de que el bebé reciba ninguna vacuna. Para más información sobre vacunas ver la sección “Advertencias y precauciones”.
Conducción y uso de máquinas
La influencia de Humira sobre la capacidad para conducir, montar en bicicleta o utilizar máquinas es pequeña. Puede producirse sensación de que la habitación da vueltas y alteraciones de la visión después de utilizar Humira.
3. Cómo usar Humira
Siga exactamente las instrucciones de administración de este medicamento indicadas por su médico. En caso de duda, consulte de nuevo a su médico.
Las dosis recomendadas de Humira en cada uno de los usos autorizados se muestran en la siguiente tabla. Su médico puede recetarle otra presentación de Humira si necesita una dosis diferente.
Artritis reumatoide | ||
Edad o peso corporal | Cuánto y con qué frecuencia se debe tomar | Notas |
Adultos | 40 mg en semanas alternas | En la artritis reumatoide, continúa el tratamiento con metotrexato durante el uso de Humira. Si su médico decide que el metotrexato es inapropiado, puede administrarse Humira en monoterapia. Si presenta artritis reumatoide y no recibe metotrexato con su tratamiento con Humira, su médico puede decidir administrarle 40 mg de Humira cada semana u 80 mg cada dos semanas. |
Psoriasis en placas | ||
Edad o peso corporal | ¿Cuánto y con qué frecuencia se debe tomar? | Notas |
Adultos | La dosis inicial es de 80 mg (una inyección de 80 mg), seguida de 40 mg en semanas alternas comenzando una semana después de la primera dosis. | Si obtiene una respuesta inadecuada, su médico puede aumentarle la dosis a 40 mg semanales u 80 mg cada dos semanas. |
Hidradenitis supurativa | ||
Edad o peso corporal | ¿Cuánto y con qué frecuencia se debe tomar? | Notas |
Adultos | La dosis inicial es de 160 mg (dos inyecciones de 80 mg en un día o una inyección de 80 mg por día durante dos días consecutivos), seguida de una dosis de 80 mg (una inyección de 80 mg) dos semanas más tarde. Después de dos semanas más, se continúa con una dosis de 40 mg cada semana u 80 mg cada dos semanas, según se lo haya recetado su médico. | Se recomienda que use un líquido antiséptico diario en las zonas afectadas. |
Adolescentes desde 12 a 17 años de edad con peso de 30 kg o más | La dosis inicial es de 80 mg (una inyección de 80 mg), seguida de 40 mg en semanas alternas comenzando una semana después. | Si obtiene una respuesta inadecuada con Humira 40 mg en semanas alternas, su médico puede aumentarle la dosis a 40 mg cada semana u 80 mg cada dos semanas. Se recomienda que use un líquido antiséptico diario en las zonas afectadas. |
Enfermedad de Crohn | ||
Edad o peso corporal | ¿Cuánto y con qué frecuencia se debe tomar? | Notas |
Niños, adolescentes y adultos desde 6 a 17 años de edad que pesen 40 kg o más | La dosis inicial es de 80 mg (una inyección de 80 mg), seguida de 40 mg dos semanas después. Si se necesita una respuesta más rápida, el médico puede prescribir una primera dosis de 160 mg (dos inyecciones de 80 mg en un día o una inyección de 80 mg por día durante dos días consecutivos), seguida de 80 mg (una inyección de 80 mg) dos semanas más tarde. A partir de entonces, la dosis habitual es de 40 mg en semanas alternas. | Su médico puede aumentarle la dosis a 40 mg cada semana u 80 mg cada dos semanas. |
Niños y adolescentes desde 6 a 17 años de edad, que pesen menos de 40 kg | La dosis inicial es de 40 mg, seguida de 20 mg dos semanas más tarde. Si se necesita una respuesta más rápida, el médico puede prescribir una primera dosis de 80 mg (una inyección de 80 mg), seguida de 40 mg dos semanas más tarde. A partir de entonces, la dosis habitual es de 20 mg en semanas alternas. | Su médico puede aumentarle la frecuencia de administración a 20 mg cada semana. |
Colitis ulcerosa | ||
Edad o peso corporal | ¿Cuánto y con qué frecuencia se debe tomar? | Notas |
Adultos | La dosis inicial es de 160 mg (dos inyecciones de 80 mg en un día o una inyección de 80 mg por día durante dos días consecutivos), seguida de 80 mg (una inyección de 80 mg) dos semanas más tarde. A partir de entonces, la dosis habitual es de 40 mg en semanas alternas. | Su médico puede aumentarle la dosis a 40 mg cada semana u 80 mg cada dos semanas. |
Niños y adolescentes desde los 6 años de edad con un peso inferior a 40 kg | Primera dosis de 80 mg (una inyección de 80 mg), seguida de 40 mg (una inyección de 40 mg) dos semanas después. A partir de entonces, la dosis habitual es de 40 mg en semanas alternas. | Debe continuar utilizando Humira a la dosis habitual, incluso después de cumplir los 18 años. |
Niños y adolescentes desde los 6 años de edad con un peso de 40 kg o superior | Primera dosis de 160 mg (dos inyecciones de 80 mg en un día o una inyección de 80 mg al día en dos días consecutivos), seguida de 80 mg (una inyección de 80 mg) dos semanas después. A partir de entonces, la dosis habitual es de 80 mg en semanas alternas. | Debe continuar utilizando Humira a la dosis habitual, incluso después de cumplir los 18 años. |
Uveítis no infecciosa | ||
Edad o peso corporal | ¿Cuánto y con qué frecuencia se debe tomar? | Notas |
Adultos | La dosis inicial es de 80 mg (una inyección de 80 mg), seguida de 40 mg en semanas alternas empezando una semana después de la primera dosis. | Se pueden seguir utilizando corticoesteroides u otros medicamentos que afecten al sistema inmunitario durante el tratamiento con Humira. Humira también se puede administrar en monoterapia. |
Niños y adolescentes desde los 2 años de edad con peso inferior a 30 kg | 20 mg en semanas alternas | Su médico le puede prescribir una dosis inicial de 40 mg que puede ser administrada una semana antes de empezar con la pauta habitual de 20 mg en semanas alternas. Se recomienda el uso de Humira en combinación con metotrexato. |
Niños y adolescentos desde los 2 años de edad con peso de 30 kg o más | 40 mg en semanas alternas | Su médico le puede prescribir una dosis inicial de 80 mg que puede ser administrada una semana antes de empezar con la pauta habitual de 40 mg en semanas alternas. Se recomienda el uso de Humira en combinación con metotrexato. |
Forma y vía de administración
Humira se inyecta bajo la piel (vía subcutánea).
En la sección 7 “Cómo inyectar Humira” se proporcionan las instrucciones detalladas sobre cómo inyectar Humira.
Si usa más Humira del que debe
Si accidentalmente se inyecta Humira con más frecuencia que la pautada por su médico o farmacéutico, debe informar de ello. Siempre lleve la caja del medicamento consigo, incluso si está vacía.
Si olvidó usar Humira
Si olvida administrarse una inyección, debe inyectarse la siguiente dosis de Humira tan pronto como lo recuerde. Después se administrará la siguiente dosis como habitualmente, como si no se hubiese olvidado una dosis.
Si interrumpe el tratamiento con Humira
La decisión de dejar de usar Humira debe ser discutida con su médico. Sus síntomas pueden volver si deja de utilizar Humira.
Si tiene cualquier otra duda sobre el uso de este medicamento, pregunte a su médico o farmacéutico.
4. Posibles efectos adversos
Al igual que todos los medicamentos, este medicamento puede producir efectos adversos, aunque no todas las personas los sufran. La mayoría de los efectos adversos son leves a moderados. Sin embargo, algunos pueden ser graves y requerir tratamiento. Los efectos adversos pueden aparecer al menos hasta 4 meses después de la última inyección de Humira.
Póngase en contacto con su médico inmediatamente si nota cualquiera de los siguientes efectos
- erupción grave, urticaria u otros signos de reacción alérgica
- hinchazón de la cara, manos, pies
- dificultad para respirar, tragar
- falta de aliento con la actividad física o al estar tumbado o hinchazón de pies
Póngase en contacto con su médico tan pronto como sea posible si nota alguno de los siguientes efectos
- signos de infección tales como fiebre, ganas de vomitar, heridas, problemas dentales, sensación de quemazón al orinar
- sensación de debilidad o cansancio
- tos
- hormigueo
- entumecimiento
- visión doble
- debilidad en brazos o piernas
- una protuberancia o una herida abierta que no se cura
- signos y síntomas de alteraciones en la sangre como fiebre persistente, cardenales, hemorragias, palidez
Los síntomas descritos anteriormente pueden ser signos de los efectos adversos listados a continuación, que se han observado con Humira.
Muy frecuentes(pueden afectar a más de 1 de cada 10 personas)
- reacciones en el lugar de inyección (incluyendo dolor, hinchazón, enrojecimiento o picor)
- infecciones del tracto respiratorio (incluyendo resfriado, moqueo, sinusitis, neumonía)
- dolor de cabeza
- dolor abdominal
- náuseas y vómitos
- sarpullido
- dolor muscular
Frecuentes(pueden afectar hasta 1 de cada 10 personas)
- infecciones graves (incluyendo envenenamiento sanguíneo y gripe)
- Infecciones intestinales (incluyendo gastroenteritis)
- infecciones de la piel (incluyendo celulitis y herpes)
- infección de oído
- infecciones orales (incluyendo infección dental y dolor frío)
- infecciones en el sistema reproductor
- infección del tracto urinario
- infecciones por hongos
- infección en las articulaciones
- tumores benignos
- cáncer de piel
- reacciones alérgicas (incluyendo alergia estacional)
- deshidratación
- cambios de humor (incluyendo depresión)
- ansiedad
- dificultad para dormir
- alteraciones sensoriales como hormigueo, escozor o entumecimiento
- migraña
- compresión de la raíz nerviosa (incluyendo dolor en la parte baja de la espalda y la pierna)
- alteraciones visuales
- inflamación del ojo
- inflamación del párpado e hinchazón del ojo
- vértigo (sensación de mareo o de que todo da vueltas)
- sensación de pulso acelerado
- alta presión sanguínea
- rubor
- hematomas (acumulación de sangre fuera de los vasos sanguíneos)
- tos
- asma
- dificultad para respirar
- sangrado gastrointestinal
- dispepsia (indigestión, hinchazón y ardor)
- reflujo ácido
- síndrome del ojo seco (incluyendo sequedad en ojos y boca)
- picores
- sarpullido con picor
- moratones
- inflamación de la piel (como eczema)
- rotura de uñas de las manos y los pies
- aumento de la transpiración
- pérdida de pelo
- psoriasis de nueva aparición o empeoramiento de la psoriasis existente
- espasmos musculares
- sangre en orina
- problemas renales
- dolor de pecho
- edema (hinchazón)
- fiebre
- disminución de plaquetas en sangre, lo que incrementa el riesgo de sangrado o moratones
- problemas de cicatrización
Poco frecuentes(pueden afectar hasta 1 de cada 100 personas)
- infecciones oportunistas (que incluyen tuberculosis y otras infecciones que ocurren cuando la resistencia a la enfermedad disminuye)
- infecciones neurológicas (incluyendo meningitis viral)
- infecciones del ojo
- infecciones bacterianas
- diverticulitis (inflamación e infección del intestino grueso)
- cáncer
- cáncer que afecta al sistema linfático
- melanoma
- alteraciones inmunológicas que pueden afectar a los pulmones, piel y ganglios linfáticos (la presentación más frecuente es sarcoidosis)
- vasculitis (inflamación de los vasos sanguíneos)
- temblor (sentirse tembloroso)
- neuropatía (trastorno del sistema nervioso)
- derrame cerebral
- pérdida de oído, zumbidos
- sensación de pulso irregular como brincos
- problemas del corazón que pueden causar dificultad para respirar o hinchazón de tobillos
- ataque al corazón
- saco en la pared de una arteria mayor, inflamación y coagulación en una vena, bloqueo de un vaso sanguíneo
- enfermedades pulmonares que pueden causar dificultad para respirar (incluyendo inflamación)
- embolia pulmonar (bloqueo de una arteria del pulmón)
- derrame pleural (almacenamiento anormal de fluido en el espacio pleural)
- inflamación del páncreas que causa un dolor grave en el abdomen y la espalda
- dificultad para tragar
- edema facial (hinchazón de la cara)
- inflamación de la vesícula; piedras en la vesícula
- grasa en el hígado
- sudores nocturnos
- cicatrices
- crisis muscular anormal
- lupus eritematoso sistémico (incluyendo inflamación de la piel, corazón, pulmones, articulaciones y otros órganos)
- interrupciones del sueño
- impotencia
- inflamaciones
Raros(pueden afectar hasta 1 de cada 1000 personas)
- leucemia (cáncer que afecta a la sangre y la médula ósea)
- reacción alérgica grave con shock
- esclerosis múltiple
- alteraciones nerviosas (como inflamación del nervio óptico y síndrome de Guillain-Barré que puede provocar debilidad muscular, sensaciones anormales, hormigueo en los brazos y la parte superior del cuerpo)
- parada cardiaca
- fibrosis pulmonar (cicatriz en el pulmón)
- perforación intestinal (orificio en el intestino)
- hepatitis
- reactivación del virus de la hepatitis B
- hepatitis autoinmune (inflamación del hígado causada por el propio sistema inmunológico del cuerpo)
- vasculitis cutánea (inflamación de los vasos sanguíneos en la piel)
- síndrome de Stevens-Johnson (los síntomas tempranos incluyen malestar, fiebre, dolor de cabeza y sarpullido)
- edema facial (hinchazón de la cara) asociado con reacciones alérgicas
- eritema multiforme (erupción inflamatoria en la piel)
- síndrome similar al lupus
- angioedema (inflamación de la piel localizada)
- reacción liquenoide en la piel (sarpullido rojizo-morado con picor)
Frecuencia no conocida(no se puede estimar la frecuencia a partir de los datos disponibles)
- linfoma hepatoesplénico de células T (cáncer sanguíneo raro que a menudo es mortal)
- carcinoma de células de Merkel (un tipo de cáncer de piel)
- sarcoma de Kaposi, un cáncer poco común relacionado con la infección por el virus del herpes humano 8. El sarcoma de Kaposi suele manifestarse con mayor frecuencia como lesiones cutáneas de color púrpura
- fallo hepático
- empeoramiento de una enfermedad llamada dermatomiositis (visto como erupción cutánea acompañada de debilidad muscular)
- aumento de peso (para la mayoría de pacientes, el aumento de peso fue reducido)
Algunos efectos adversos observados con Humira pueden no tener síntomas y sólo pueden ser identificados mediante un análisis de sangre. Estos incluyen:
Muy frecuentes(pueden afectar a más de 1 de cada 10 personas)
- bajo recuento sanguíneo de células blancas
- bajo recuento sanguíneo de células rojas
- aumento de lípidos en sangre
- aumento de enzimas hepáticas
Frecuentes(pueden afectar hasta 1 de cada 10 personas)
- alto recuento sanguíneo de células blancas
- bajo recuento sanguíneo de plaquetas
- aumento de ácido úrico en sangre
- valores anormales de sodio en sangre
- bajo nivel de calcio en sangre
- bajo nivel de fosfato en sangre
- azúcar en sangre alta
- valores altos de lactato deshidrogenasa en sangre
- presencia de autoanticuerpos en sangre
- bajo nivel de potasio en sangre
Poco frecuentes(pueden afectar hasta 1 de cada 100 personas)
- valores de bilirrubina elevados (análisis de función hepática)
Raros(pueden afectar hasta 1 de cada 1000 personas)
- recuentos bajos en sangre para células blancas, células rojas y plaquetas
Comunicación de efectos adversos
Si experimenta cualquier tipo de efecto adverso, consulte con su médico o farmacéutico, incluso si se trata de posibles efectos adversos que no aparecen en este prospecto. También puede comunicarlos directamente a través del sistema nacional de notificación incluido en el Apéndice V. Mediante la comunicación de efectos adversos usted puede contribuir a proporcionar más información sobre la seguridad de este medicamento.
5. Conservación de Humira
Mantener este medicamento fuera de la vista y del alcance de los niños.
No utilice este medicamento después de la fecha de caducidad que aparece en el envase después de “CAD”.
Conservar en nevera (entre 2?C y 8?C). No congelar.
Conservar la pluma precargada en el embalaje exterior para protegerla de la luz.
Almacenamiento alternativo:
Cuando sea necesario (por ejemplo cuando esté de viaje), puede almacenar una pluma precargada individual de Humira a temperatura ambiente (hasta 25ºC) durante un periodo máximo de 14 días – asegúrese de protegerlo de la luz. Una vez que se ha sacado de la nevera para almacenar la pluma a temperatura ambiente, debe usarla en los siguientes 14 días o desecharla, incluso si la vuelve a meter en la nevera.
Debe anotar la fecha en la que retiró la pluma de la nevera y la fecha después de la cual debe desechar la pluma.
Los medicamentos no se deben tirar por los desagües ni a la basura. Pregunte a su médico o farmacéutico cómo deshacerse de los envases y de los medicamentos que ya no necesita. De esta forma, ayudará a proteger el medio ambiente.
6. Contenido del envase e información adicional
Composición de Humira
El principio activo es adalimumab.
Los demás componentes son: manitol, polisorbato 80 y agua para preparaciones inyectables.
Aspecto del producto y contenido del envase
Humira 80 mg solución inyectable en pluma precargada se suministra como una solución estéril de 80 mg de adalimumab disuelto en 0,8 ml de solución.
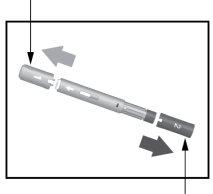
La pluma precargada de Humira es una pluma bicolor gris/ciruela de un solo uso que contiene una jeringa de cristal con Humira. Tiene dos tapas: una es gris y tiene un “1” impreso y la otra es ciruela y tiene impreso un “2”. Tiene una ventana en cada una de las caras de la pluma a través de la cual puede ver la solución de Humira que contiene la jeringa.
La pluma precargada de Humira está disponible en envases que contienen:
- 1 pluma precargada para uso por el paciente con 2 toallitas empapadas en alcohol (1 de recambio).
- 3 plumas precargadas para uso por el paciente con 4 toallitas empapadas en alcohol (1 de recambio)
Puede que solamente estén comercializados algunos tamaños de envases.
Humira puede estar disponible en vial, en jeringa precargada y/o en pluma precargada.
Titular de la autorización de comercialización
AbbVie Deutschland GmbH & Co. KG
Knollstrasse
67061 Ludwigshafen
Alemania
Responsable de la fabricación
AbbVie Biotechnology GmbH
Knollstrasse
67061 Ludwigshafen
Alemania
Pueden solicitar más información respecto a este medicamento, dirigiéndose al representante local del titular de la autorización de comercialización.
België/Belgique/Belgien AbbVie SA Tél/Tel: +32 10 477811 | Lietuva AbbVie UAB Tel: +370 5 205 3023 |
???????? ???? ???? ???.:+359 2 90 30 430 | Luxembourg/Luxemburg AbbVie SA Belgique/Belgien Tél/Tel: +32 10 477811 |
Ceská republika AbbVie s.r.o. Tel: +420 233 098 111 | Magyarország AbbVie Kft. Tel.:+36 1 455 8600 |
Danmark AbbVie A/S Tlf: +45 72 30-20-28 | Malta V.J.Salomone Pharma Limited Tel: +356 21220174 |
Deutschland AbbVie Deutschland GmbH & Co. KG Tel: 00800 222843 33 (gebührenfrei) Tel: +49 (0) 611 / 1720-0 | Nederland AbbVie B.V. Tel: +31 (0)88 322 2843 |
Eesti AbbVie OÜ Tel: +372 623 1011 | Norge AbbVie AS Tlf: +47 67 81 80 00 |
Ελλ?δα AbbVie ΦΑΡΜΑΚΕΥΤΙΚΗ Α.Ε. Τηλ: +30 214 4165 555 | Österreich AbbVie GmbH Tel: +43 1 20589-0 |
España AbbVie Spain, S.L.U. Tel: +34 91 384 09 10 | Polska AbbVie Polska Sp. z o.o. Tel.: +48 22 372 78 00 |
France AbbVie Tél: +33 (0) 1 45 60 13 00 | Portugal AbbVie, Lda. Tel: +351 (0)21 1908400 |
Hrvatska AbbVie d.o.o. Tel + 385 (0)1 5625 501 | România AbbVie S.R.L. Tel: +40 21 529 30 35 |
Ireland AbbVie Limited Tel: +353 (0)1 4287900 | Slovenija AbbVie Biofarmacevtska družba d.o.o. Tel: +386 (1)32 08 060 |
Ísland Vistor hf. Tel: +354 535 7000 | Slovenská republika AbbVie s.r.o. Tel: +421 2 5050 0777 |
Italia AbbVie S.r.l. Tel: +39 06 928921 | Suomi/Finland AbbVie Oy Puh/Tel: +358 (0)10 2411 200 |
Κ?προς Lifepharma (Z.A.M.) Ltd Τηλ.: +357 22 34 74 40 | Sverige AbbVie AB Tel: +46 (0)8 684 44 600 |
Latvija AbbVie SIA Tel: +371 67605000 |
Fecha de la última revisión de este prospecto
La información detallada de este medicamento está disponible en la página web de la Agencia Europea de Medicamentos: http://www.ema.europa.eu.
Para solicitar una copia de este prospecto en
- Cómo inyectar Humira
- Las siguientes instrucciones explican cómo inyectarse Humira usted mismo usando la pluma precargada. Lea detenidamente todas las instrucciones primero y a continuación sígalas paso a paso.
- Su médico, enfermero o farmacéutico le indicará la técnica para inyectarse usted mismo.
- No intente ponerse la inyección usted mismo hasta no estar seguro de que comprende cómo preparar y administrar la inyección.
- Después de que le formen correctamente, usted mismo u otra persona, como un familiar o amigo, pueden poner la inyección.
- Utilice solo cada pluma precargada para una inyección.
Humira Pluma precargada
Tapa gris1 Funda blanca de aguja Flecha blanca Tapa de color ciruela2
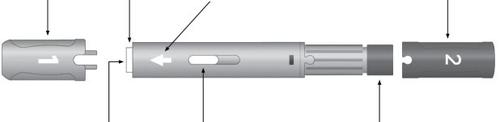
Aguja Visor para inspección Botón activador de color ciruela
No use la pluma precargada y llame a su médico o farmacéutico si
- el líquido está turbio, presenta coloración o tiene escamas o partículas en él
- ha pasado la fecha de caducidad (CAD)
- el líquido ha estado congelado o se ha dejado expuesto a la luz solar directa
- la pluma precargada se ha caído o aplastado
No retire todas las tapas hasta justo antes de la inyección. Mantener fuera de la vista y del alcance de los niños.
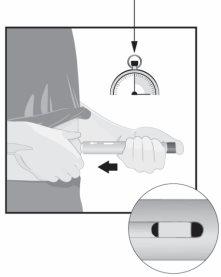
PASO1 Saque Humira de la nevera. Deje Humira a temperatura ambiente entre 15 y 30minutosantes de la inyección.
| |
PASO2 Pluma
Toallita | Compruebe la fecha de caducidad (CAD). Nouse la pluma precargada si la fecha de caducidad (CAD) ya ha pasado. Sobre una superficie lisa y limpia coloque
Lávese las manos y séquelas. |
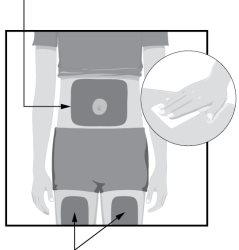
PASO3 Zonas inyectables
Zonas inyectables | Escoja un lugar de su cuerpo para poner la inyección:
Limpie el lugar de inyección con la toallita impregnada en alcohol con movimientos circulares.
|
PASO4
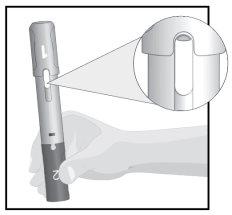
| Mantenga la pluma precargada con la tapa gris 1 mirando hacia arriba. Compruebe el visor de inspección.
|
PASO5 Tapa 1
Tapa2 | Tire de la tapa gris 1 directamente para sacarla. Tírela y novuelva a colocarla.
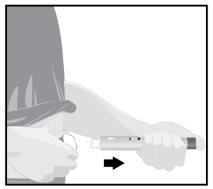
Tire de la tapa 2 de color ciruela para sacarla. Tírela y novuelva a colocarla. La pluma precargada está ahora lista para su uso. Gire la pluma precargada de forma que la flecha blanca señale hacia el lugar de la inyección. |
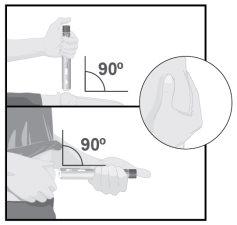
PASO6
| Apriete la piel en la zona de la inyección con su otra mano para hacer que se eleve y manténgala agarrada con firmeza hasta que haya terminado de administrar la inyección. Apunte la flecha blanca hacia el lugar de la inyección (muslo o abdomen). Coloque la funda blanca de la aguja recta (en un ángulo de 90°)contra el lugar de la inyección. Sostenga la pluma precargada de forma que pueda ver el visor de inspección. Nopresione el botón activador de color ciruela hasta que esté preparado para administrar la inyección. |
PASO7 15segundos
| Empuje con firmezala pluma precargadacontra el lugar de la inyección antes de iniciar la administración. Siga apretandopara evitar que la pluma precargada se salga de la piel durante la inyección. Aprieteel botón activador de color ciruela y cuente lentamente hasta 15segundos.
La inyección se ha completado cuando el indicador amarillo ha dejado de moverse. |
PASO8
| Cuando la inyección se haya completado, separe la pluma precargada con lentitud de la piel. La funda blanca de la aguja cubrirá la punta de la aguja.
Si hay más de algunas gotas de líquido en el lugar de la inyección, póngase en contacto con su médico, enfermero o farmacéutico. Después de completar la inyección, coloque una bolita de algodón o una gasa sobre la piel en el lugar de la inyección.
|
PASO9 Tire la pluma precargada en un contenedor de desecho especial (contenedor de objetos punzantes) según se lo haya indicado su médico, enfermero o farmacéutico.
Las tapas, la toallita impregnada en alcohol, la bola de algodón o la gasa, el blíster y el embalaje pueden tirarse en la basura doméstica. |
- País de registro
- Principio activo
- Requiere recetaSí
- Fabricante
- Esta información es de carácter general y no sustituye la consulta con un profesional sanitario.
- Alternativas a HUMIRA 80 MG SOLUCION INYECTABLE EN PLUMA PRECARGADAForma farmacéutica: INYECTABLE, 20 mgPrincipio activo: AdalimumabFabricante: Amgen Europe B.V.Requiere recetaForma farmacéutica: INYECTABLE, 20 mgPrincipio activo: AdalimumabFabricante: Amgen Europe B.V.Requiere recetaForma farmacéutica: INYECTABLE, 40 mgPrincipio activo: AdalimumabFabricante: Amgen Europe B.V.Requiere receta
Médicos online para HUMIRA 80 MG SOLUCION INYECTABLE EN PLUMA PRECARGADA
Comenta la dosis, los posibles efectos secundarios, interacciones, contraindicaciones o la revisión de receta de HUMIRA 80 MG SOLUCION INYECTABLE EN PLUMA PRECARGADA, sujeto a valoración médica y a la normativa local.
Preguntas frecuentes