
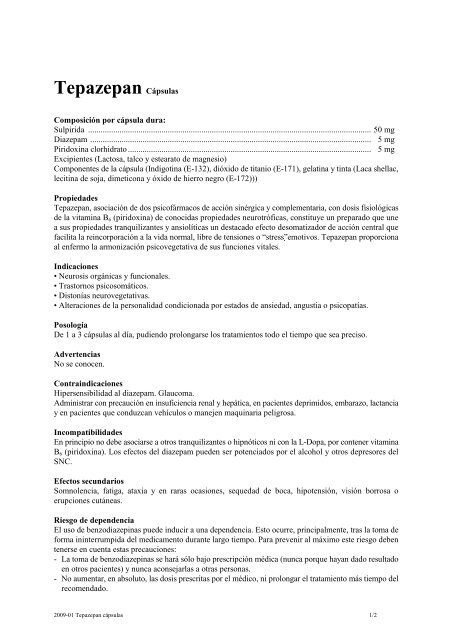
TEPAZEPAN 50 mg/5 mg/5 mg HARD CAPSULES

How to use TEPAZEPAN 50 mg/5 mg/5 mg HARD CAPSULES
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
Tepazepan 50 mg/5 mg/ 5 mghard capsules
sulpiride/diazepam/pyridoxine hydrochloride
Read the entire package leaflet carefully before starting to take the medication, as it contains important information for you.
- Keep this package leaflet, as you may need to read it again.
- If you have any doubts, consult your doctor or pharmacist.
- This medication has been prescribed to you only, and you should not give it to others, even if they have the same symptoms as you, as it may harm them.
- If you experience side effects, consult your doctor or pharmacist, even if they are not listed in this package leaflet. See section 4.
Contents of the Package Leaflet:
- What is Tepazepan and what is it used for
- What you need to know before taking Tepazepan
- How to take Tepazepan
- Possible side effects
- Storage of Tepazepan
- Package contents and additional information
1. What is Tepazepan and what is it used for
Tepazepan contains the active ingredients diazepam and sulpiride.
Diazepam belongs to the group of medications called benzodiazepines.
Sulpiride belongs to the group of antipsychotic medications, also known as neuroleptics.
Additionally, it contains the active ingredient pyridoxine hydrochloride (vitamin B6), a water-soluble vitamin involved in human metabolic processes.
Tepazepan is indicated for the treatment of depression in patients with anxiety.
This treatment will only be used for the treatment of a severe disorder that limits activity or subjects the patient to significant stress.
2. What you need to know before taking Tepazepan
Do not take Tepazepan
- If you are allergic (hypersensitive) to diazepam (or other benzodiazepines), sulpiride (or other benzamides), pyridoxine hydrochloride (vitamin B6), or any of the other components of this medication (listed in section 6).
- If you have been diagnosed with pheochromocytoma (tumor of the adrenal gland).
- If you are pregnant (planning or suspect you may be).
- If you are breastfeeding your child.
- If you have been diagnosed with prolonged QT interval or bradycardia.
- If you are being treated with levodopa or ropinirol (medications for Parkinson's disease) or neuroleptics (medications for mental illness).
- If you have been diagnosed with arrhythmias.
- If you are taking anti-arrhythmic medications, such as quinidine, disopyramide, amiodarone, or sotalol.
- If you are taking cisapride, thioridazine, erythromycin, vincamine, halofantrine, pentamidine, or sparfloxacin.
- If you are being treated with medications that prolong the QT interval (see section "Other medications and Tepazepan").
- If you have electrolyte disturbances (potassium, magnesium), anorexia (loss of appetite), vomiting, or diarrhea, or if you are taking medications that can trigger these disturbances, such as diuretics, intravenous amphotericin B, glucocorticoids, or tetracosactide.
- If you have myasthenia gravis (severe muscle weakness).
- If you have respiratory failure.
- If you have sleep apnea syndrome.
- If you have severe liver failure.
- If you have narrow-angle glaucoma (increased intraocular pressure).
- If you have severe chronic hypercapnia (elevated carbon dioxide levels in the blood).
- If you have muscle problems.
- If you have prolactin-dependent tumors (hormone that stimulates milk secretion), such as prolactinomas of the pituitary gland and breast cancer.
Warnings and precautions
Consult your doctor before starting to take this medication:
- If you have any liver or kidney disorders.
- If you have muscle weakness.
- If you have other diseases or if someone in your family has a history of blood clots, as these medications may be associated with the formation of blood clots.
- If you have allergies.
- If you have a history of drug or alcohol abuse.
- If you are taking other medications.
- If you have a clinical condition that may favor the appearance of cardiac rhythm disorders, as this medication may increase the risk of severe cardiac rhythm disturbances.
- If you are at risk of having a stroke.
- If you have kidney failure.
- If you have a history of epilepsy, as it may favor the appearance of epileptic seizures and convulsions.
- In patients taking antiparkinsonian medication for a condition other than Parkinson's disease.
- If you experience fever of unknown origin and muscle stiffness, as it could be a sign of malignant neuroleptic syndrome, a potentially fatal complication characterized by elevated body temperature, muscle stiffness, and nervous system dysfunction (autonomic dysfunction). If you experience a fever of unknown origin, you should discontinue treatment with sulpiride (see "Possible side effects").
- If you have diabetes mellitus or are at risk of developing diabetes.
- If you experience an infection or fever of unknown origin, inform your doctor, as it could be a sign of blood disorders (see "Possible side effects"). There have been reports of leukopenia (decreased white blood cell count), neutropenia (decreased neutrophil count), and agranulocytosis (decreased granulocyte count) with the use of antipsychotics.
Consult your doctor or pharmacist if you experience such symptoms.
It is not recommended to take this medication for the treatment of psychoses or anxiety associated with depression. Behavioral disorders may appear, mainly in elderly patients, and treatment should be discontinued in such cases.
The use of benzodiazepines may lead to dependence. This occurs mainly after uninterrupted use of the medication for a long time. To minimize the risk of dependence, the following precautions should be taken:
- The use of benzodiazepines will only be done under medical prescription (never because they have been effective for other patients) and will never be recommended to other people.
- Do not increase the prescribed doses or prolong treatment beyond the recommended time.
- Consult your doctor regularly to decide whether to continue treatment.
Elderly patients
In elderly patients, the doctor may prescribe a lower dose (e.g., half the average dose) and monitor the response to treatment. Please follow your doctor's instructions carefully.
If you have any liver or kidney disorders or muscle weakness, your doctor will decide whether you should take a lower dose or not take it at all.
Children
Tepazepan should not be administered to children.
Other medications and Tepazepan
Inform your doctor or pharmacist if you are taking, have recently taken, or may need to take any other medication.
Before starting treatment, your doctor should be informed if you are taking other medications (including those that have not been prescribed). This is extremely important because the simultaneous use of more than one medication can increase or decrease its effect. Therefore, you should not take other medications at the same time as Tepazepan unless your doctor is informed and approves it beforehand.
Medications containing cisapride, cimetidine, ketoconazole, fluvoxamine, fluoxetine, and omeprazole temporarily increase the sedative effect of Tepazepan, increasing the risk of somnolence.
Similarly, the metabolism of phenytoin may be affected if you are taking Tepazepan. Therefore, if you are taking this medication, your doctor will adjust the doses accordingly.
Patients with Parkinson's disease treated with levodopa should not take this medication.
Certain medications that inhibit liver enzymes may increase the activity of this medication.
Inform your doctor if you are taking or have taken any of the following medications:
- Anti-arrhythmic medications such as quinidine, disopyramide, amiodarone, and sotalol.
- Medications that induce a decrease in heart rate, such as diltiazem, verapamil, clonidine, and guanfacine; digitalis.
- Medications that induce a decrease in potassium and magnesium levels.
- Other medications, such as cisapride, thioridazine, intravenous erythromycin, vincamine, halofantrine, pentamidine, sparfloxacin, methadone, pimozide, haloperidol, and sultoprid.
- Medications containing pyridoxine with L-Dopa, barbiturates, and phenytoin (anti-arrhythmic).
- Lithium and lithium salts (medications for the treatment of manic-depressive disorder or bipolar affective disorder).
- Sucralfate (medication for the treatment and prevention of duodenal ulcers).
- Antacids.
- Medications for lowering blood pressure.
- Medications that depress the central nervous system, including narcotics, analgesics, sedating antihistamines, barbiturates, benzodiazepines, and other anxiolytic medications.
The concomitant use of this medication and opioids (strong analgesics, medications for substitution therapy, and some cough medications) increases the risk of somnolence, breathing difficulties (respiratory depression), coma, and can be fatal. Therefore, concomitant use should only be considered when other treatment options are not possible.
However, if your doctor prescribes this medication along with opioids, the dose and duration of concomitant treatment should be limited by your doctor.
Please inform your doctor about all opioid medications you are taking and follow your doctor's dosage recommendations closely. It may be helpful to inform friends or family members to be aware of the signs and symptoms mentioned above. Contact your doctor if you experience such symptoms.
Taking Tepazepan with food, drinks, and alcohol
During treatment, avoid alcoholic beverages. The effect of alcohol may increase sedation, which can affect your ability to drive or operate machinery. If you need additional information on this point, consult your doctor.
Do not consume grapefruit juice during treatment with Tepazepan.
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or plan to become pregnant, consult your doctor or pharmacist before using this medication.
Pregnancy
Newborns of mothers who have used sulpiride in the last trimester of pregnancy may experience the following symptoms: tremors, muscle stiffness, and/or weakness, somnolence, agitation, breathing difficulties, and feeding problems. If your newborn experiences any of these symptoms, contact your doctor.
Breastfeeding
Benzodiazepines are excreted in breast milk, so it is not recommended to use this medication during breastfeeding. If your doctor considers that you need to take it, you should replace breastfeeding with formula feeding.
Driving and using machines
This medication may alter your ability to drive or operate machinery, as it can cause somnolence, decrease attention, or decrease reaction time. The appearance of these effects is more likely at the start of treatment or when the dose is increased. Do not drive or operate machinery if you experience any of these effects.
Tepazepan contains lactose
This medication contains lactose. If your doctor has told you that you have an intolerance to certain sugars, consult with them before taking this medication.
3. How to take Tepazepan
Follow your doctor's instructions for administration of this medication exactly. If in doubt, consult your doctor or pharmacist again.
This medication is for oral administration.
Swallow the capsules without chewing, with water or another non-alcoholic beverage.
The dose of this medication should be as indicated by your doctor and at the times indicated by them, according to your individual needs.
Your doctor will indicate the duration of your treatment. Do not stop treatment before your doctor indicates it and under the conditions they prescribe.
Remember to take your medication.
Follow these instructions unless your doctor has given you different instructions:
Adults
The recommended starting dose is 1 to 3 capsules per day, unless your doctor indicates otherwise.
Elderly patients
The recommended starting dose is 1 capsule per day.
Patient with mild or moderate kidney or liver impairment
The recommended starting dose is 1 capsule per day.
Patient with muscle weakness
The recommended starting dose is 1 capsule per day.
Use in children
Its use is not recommended in children.
Treatment duration
The treatment duration should be as short as possible and never exceed 2-3 months, including the gradual withdrawal period.
Do not prolong treatment beyond the recommended time.
To avoid withdrawal symptoms, do not stop taking this medication abruptly, especially if you have been taking it for a long time.
This medication should be taken at least two hours before antacids and sucralfate.
It is advisable for your doctor to review the treatment periodically, especially if you have a history of alcoholism, drug abuse, or severe personality disorders.
If you think the effect of this medication is too strong or too weak, inform your doctor or pharmacist.
If you take more Tepazepan than you should
In case of overdose or accidental ingestion, consult your doctor or pharmacist immediately, or call the Toxicology Information Service, phone 91 562 04 20, indicating the medication and the amount ingested.
In case of overdose, muscle spasms of the face, neck, and tongue may occur. Some patients may develop parkinsonian manifestations (tremors, rigidity) with vital risk and coma.
In case of overdose, appropriate supportive measures should be instituted, recommending close monitoring of vital functions and cardiac function until the patient recovers.
In case of severe extrapyramidal symptoms (tremors, increased muscle tone, decreased movement, hypersalivation, etc.), anticholinergic agents should be administered.
If you forget to take Tepazepan
Do not take a double dose to make up for forgotten doses. If you forget to take a dose, wait for the next scheduled dose.
If you interrupt treatment with Tepazepan
When stopping this medication, you may experience restlessness, anxiety, insomnia, lack of concentration, headache, and sweating.
It is not recommended to interrupt medication abruptly, but rather to gradually reduce the dose, always following the doctor's instructions.
If you have any other doubts about the use of this medication, ask your doctor or pharmacist.
4. Possible Adverse Effects
Like all medicines, this medicine may cause adverse effects, although not all people suffer from them.
Diazepam
Frequent Adverse Effects(may affect up to 1 in 10 patients):
- Fatigue, muscle weakness.
Very Rare Adverse Effects(may affect up to 1 in 10,000 people)
- Alteration of heart rhythm, cardiac arrest.
- Jaundice (yellowish appearance of the skin and eyes).
- Increase in transaminases and alkaline phosphatase in blood.
Unknown Frequency(cannot be estimated from available data):
- Confusion, deterioration of alertness, headache, dizziness, ataxia (inability to coordinate voluntary muscle movements), difficulty articulating words, and memory loss.
- Restlessness, agitation, irritability, disorientation, aggressiveness, nervousness, hostility, anxiety, delirium (incoherence of ideas), fits of rage, nightmares, hallucinations, psychosis, hyperactivity, inappropriate behavior, and other behavioral changes. Decreased libido, sleep disorder (nightmares), depression, dependence (administration of the medicine, even at therapeutic doses, may lead to the development of physical dependence: suppression of treatment may lead to the development of withdrawal or rebound phenomena. Cases of abuse have been reported).
- Blurred vision, double vision (diplopia).
- Vertigo.
- Orthostatic hypotension (decrease in blood pressure when standing up) and circulatory disorders.
- Respiratory depression, respiratory failure.
- Dry mouth, constipation, increased salivation, nausea.
- Rash (skin inflammation), itching, urticaria (red patches).
- Urinary retention, urinary incontinence.
Sulpiride
Frequent Adverse Effects(may affect up to 1 in 10 patients):
- Sedation or somnolence, dose-related extrapyramidal disorder (abnormal movements) such as restlessness, akathisia (inability to sit or remain seated), tremors, parkinsonism (symptoms similar to those of Parkinson's disease, which usually occur at the start of treatment. These symptoms are generally reversible if antiparkinsonian medication is administered).
- Insomnia (difficulty sleeping).
- Increased levels of the hormone prolactin (hyperprolactinemia).
- Constipation.
- Increased liver enzymes.
- Maculopapular rash (appearance of red patches and papules on the skin).
- Chest pain, milk secretion from the breasts outside of pregnancy.
- Weight gain.
Infrequent Adverse Effects(may affect up to 1 in 100 patients):
- Dystonia (muscle spasms), dyskinesia (abnormal and involuntary movements), increased muscle tone.
- Leukopenia (decrease in the number of white blood cells).
- Orthostatic hypotension (decrease in blood pressure when standing up).
- Increased salivation.
- Amenorrhea in a fertile woman, breast enlargement, abnormal orgasm, impotence.
Rare Adverse Effects(may affect up to 1 in 1,000 patients):
- Oculogyric crisis (involuntary deviation of the gaze).
- Ventricular fibrillation, ventricular arrhythmia (change in heart rhythm), ventricular tachycardia (rapid succession of heartbeats whose cause resides in the ventricles).
Unknown Frequency(cannot be estimated from available data):
- Seizures, malignant neuroleptic syndrome (complication characterized by elevated body temperature, muscle rigidity, and even death), decreased or slowed involuntary movements (hypokinesia), tardive dyskinesia (characterized by rhythmic and involuntary movements mainly of the tongue and/or face, as has been reported with all neuroleptics, after administration for more than 3 months. Antiparkinsonian medication is ineffective or may worsen symptoms).
- Confusion.
- Prolongation of the QT interval (heart conduction problems) and alteration of heart rhythm (torsades de pointes), cardiac arrest, sudden death.
- Neutropenia (decrease in the number of white blood cells called neutrophils) and agranulocytosis (decrease in a type of white blood cells, granulocytes).
- Anaphylactic reactions (severe allergic reaction), urticaria, difficulty breathing (dyspnea), decrease in blood pressure, and anaphylactic shock (severe allergic reaction that can be life-threatening).
- Increased blood pressure, blood clots in the veins, especially in the legs (symptoms include swelling, pain, and redness in the leg), these clots can move through the blood vessels to the lungs, causing chest pain and difficulty breathing. If you experience any of these symptoms, seek medical attention immediately.
- Torticollis, trismus (contraction of the jaw muscles).
- Withdrawal syndrome in newborns, extrapyramidal symptoms (involuntary movements).
- Enlargement of the breasts in men.
- Increased level of creatine phosphokinase in blood (an indicator of muscle damage).
If you consider that any of the adverse effects you are experiencing is serious or if you notice any adverse effect not mentioned in this prospectus, inform your doctor or pharmacist.
A small increase in the number of deaths has been reported in elderly patients with dementia treated with antipsychotics, compared to those who do not receive this treatment.
Reporting of Adverse Effects
If you experience any type of adverse effect, consult your doctor or pharmacist, even if it is a possible adverse effect that does not appear in this prospectus.
You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines: www.notificaram.es. By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Storage of Tepazepan
Keep out of sight and reach of children.
Do not use this medicine after the expiration date that appears on the packaging after CAD. The expiration date is the last day of the month indicated.
Do not store at a temperature above 30 °C.
Medicines should not be thrown away through wastewater or household waste. Deposit the packaging and medicines you no longer need at the SIGRE Point of the pharmacy. In case of doubt, ask your pharmacist how to dispose of the packaging and medicines you no longer need. This will help protect the environment.
6. Package Contents and Additional Information
Composition of Tepazepan
The active ingredients are sulpiride, diazepam, and pyridoxine hydrochloride. Each capsule contains 50 mg of sulpiride, 5 mg of diazepam, and 5 mg of pyridoxine hydrochloride.
The other components are: lactose, talc, and magnesium stearate.
The components of the capsule are: indigotine (E-132), titanium dioxide (E-171), gelatin, and ink (shellac lacquer, soy lecithin, dimethicone, and black iron oxide (E-172).
Appearance of the Product and Package Contents
Tepazepan is presented in the form of hard gelatin capsules of blue color.
It is presented in packages of 30 capsules packaged in blisters.
Marketing Authorization Holder and Manufacturer
Kern Pharma, S.L.
Venus, 72 – Pol. Ind. Colón II
08228 Terrassa - Barcelona
Spain
Date of the Last Revision of this Prospectus:February 2025
Detailed information about this medicine is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es
- Country of registration
- Average pharmacy price2.76 EUR
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to TEPAZEPAN 50 mg/5 mg/5 mg HARD CAPSULESDosage form: CAPSULE, 5/50 mg/mgActive substance: Benzodiazepine derivativesManufacturer: Neuraxpharm Spain S.L.Prescription requiredDosage form: TABLET, 0.25 mgActive substance: alprazolamManufacturer: Laboratorios Alter S.A.Prescription requiredDosage form: TABLET, 0.5 mgActive substance: alprazolamManufacturer: Laboratorios Alter S.A.Prescription required
Online doctors for TEPAZEPAN 50 mg/5 mg/5 mg HARD CAPSULES
Discuss questions about TEPAZEPAN 50 mg/5 mg/5 mg HARD CAPSULES, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions











