
TEMOZOLOMIDE SUN 20 mg HARD CAPSULES


How to use TEMOZOLOMIDE SUN 20 mg HARD CAPSULES
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Temozolomide SUN 20 mg hard capsules EFG
temozolomide
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you experience any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What Temozolomide SUN is and what it is used for
- What you need to know before you take Temozolomide SUN
- How to take Temozolomide SUN
- Possible side effects
- Storing Temozolomide SUN
- Contents of the pack and other information
1. What Temozolomide SUN is and what it is used for
Temozolomide SUN contains a medicine called temozolomide. This medicine is an anti-tumour agent.
Temozolomide SUN is used to treat certain types of brain tumours:
- in adults with newly diagnosed glioblastoma multiforme. Temozolomide SUN is used first in combination with radiotherapy (concomitant phase of treatment) and then alone (monotherapy phase of treatment).
- in children aged 3 years and older and adults with malignant glioma, such as glioblastoma multiforme or anaplastic astrocytoma. Temozolomide SUN is used to treat these tumours if they come back or get worse after standard treatment.
2. What you need to know before you take Temozolomide SUN
Do not take Temozolomide SUN if:
- you are allergic to temozolomide or any of the other ingredients of this medicine (listed in section 6).
- you have had an allergic reaction to dacarbazine (a cancer medicine sometimes called DTIC). Signs of an allergic reaction include itching, difficulty breathing or wheezing, or swelling of the face, lips, tongue, or throat.
- you have a severely reduced number of certain types of blood cells, such as white blood cells or platelets (known as myelosuppression). These blood cells are important for fighting infection and for blood to clot properly. Your doctor will do a blood test to make sure you have enough of these cells before starting treatment.
Warnings and precautions
Talk to your doctor, pharmacist, or nurse before starting Temozolomide SUN
- because you will be closely monitored for the development of a severe respiratory infection called Pneumocystis jirovecii (PCP pneumonia). If you have been newly diagnosed with glioblastoma multiforme, you may be given Temozolomide SUN for 42 days in combination with radiotherapy. In this case, your doctor will also prescribe a medicine to help you avoid this type of pneumonia (PCP).
- if you have ever had or may currently have a hepatitis B infection, as Temozolomide SUN could reactivate hepatitis B, which can be fatal in some cases. Before starting treatment, your doctor will carefully examine you for signs of this infection.
- if you have a low red blood cell count (anaemia), low white blood cell and platelet count, or blood clotting problems before starting treatment, or if these problems develop during treatment. You will have regular blood tests during treatment to monitor the side effects of Temozolomide SUN on your blood cells. Your doctor may decide to reduce your dose, interrupt, discontinue, or change your treatment. You may also need other treatments. In some cases, it may be necessary to discontinue treatment with Temozolomide SUN.
- because there may be a small risk of other changes in blood cells, including leukaemia.
- if you have nausea (feeling sick) or vomiting, very common side effects of Temozolomide SUN (see section 4), your doctor may prescribe a medicine (antiemetic) to help prevent vomiting.
- If you vomit frequently before or during treatment, talk to your doctor about the best time to take Temozolomide SUN until the vomiting is under control. If you vomit after taking the medicine, do not take a second dose on the same day.
- if you have a fever or symptoms of an infection, contact your doctor immediately.
- if you are over 70 years old, you may be more likely to get infections, bleeding, or bruising.
- if you have liver or kidney problems, your dose of Temozolomide SUN may need to be adjusted.
Children and adolescents
Do not give this medicine to children under 3 years old, as its effect in this age group has not been studied. There is limited information in patients over 3 years who have taken Temozolomide SUN.
Taking Temozolomide SUN with other medicines
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine, as you should not receive treatment with Temozolomide SUN during pregnancy unless your doctor tells you to.
Both men and womenwho are taking Temozolomide SUN should use effective contraceptive methods (see also “Male fertility”).
You should stop breastfeeding during treatment with Temozolomide SUN.
Male fertility
Temozolomide SUN may cause permanent infertility. Male patients should use an effective contraceptive method and not get their partner pregnant until 6 months after finishing treatment. It is recommended to consult about sperm preservation before treatment.
Driving and using machines
Temozolomide SUN may make you feel tired or sleepy. If this happens, do not drive or use tools or machines, or ride a bike until you see how this medicine affects you (see section 4).
Temozolomide SUN contains lactose
Temozolomide SUN contains lactose (a type of sugar). If your doctor has told you that you have an intolerance to some sugars, talk to them before taking this medicine.
3. How to take Temozolomide SUN
Follow exactly the instructions given to you by your doctor or pharmacist. If you are not sure, talk to your doctor or pharmacist again.
Dose and duration of treatment
Your doctor will decide the dose of Temozolomide SUN that you need. The dose will depend on your size (height and weight) and whether you have a recurrent tumour and have had chemotherapy before.
You may be given other medicines (antiemetics) to take before and/or after Temozolomide SUN to prevent or control nausea and vomiting.
Patient with newly diagnosed glioblastoma multiforme
If you have been newly diagnosed, treatment will be in two phases:
- first, treatment with radiotherapy (concomitant phase)
- followed by treatment with Temozolomide SUN alone (monotherapy phase).
During the concomitant phase, your doctor will prescribe a dose of Temozolomide SUN of 75 mg/m2 (usual dose). You will take this dose every day for 42 to 49 days in combination with radiotherapy. The dose of Temozolomide SUN may be reduced or stopped depending on the results of your blood tests and how you react to the medicine during the concomitant phase.
Once radiotherapy is finished, treatment will be stopped for 4 weeks. This will help your body recover.
Then, you will start the monotherapy phase.
During the monotherapy phase, the dose and way of taking Temozolomide SUN may vary. Your doctor will decide the exact dose that you need. You may have up to six treatment periods (cycles). Each cycle lasts 28 days. The first dose will be 150 mg/m2. You will take the new dose of Temozolomide SUN once a day for the first 5 days ("dosing days") of each cycle. Then, you will not take Temozolomide SUN for 23 days. This is a 28-day treatment cycle.
After day 28, the next cycle will start. You will take Temozolomide SUN once a day for 5 days, followed by 23 days without taking it. The dose of Temozolomide SUN may be adjusted, reduced, or stopped depending on the results of your blood tests and how you react to the medicine during each treatment cycle.
Patient with recurrent or worsening tumours (malignant gliomas, such as glioblastoma multiforme or anaplastic astrocytoma) taking only Temozolomide SUN.
A treatment cycle with Temozolomide SUN lasts 28 days.
You will take Temozolomide SUN only once a day for the first 5 days. This daily dose will depend on whether you have had chemotherapy before.
If you have not had chemotherapy before, your first dose of Temozolomide SUN will be 200 mg/m2 once a day for the first 5 days. If you have had chemotherapy before, your first dose of Temozolomide SUN will be 150 mg/m2 once a day for the first 5 days. Then, you will not take Temozolomide SUN for 23 days. This is a 28-day treatment cycle.
After day 28, the next cycle will start. You will take Temozolomide SUN once a day for 5 days, followed by 23 days without taking it.
Before each new treatment cycle, you will have blood tests to check if the dose of Temozolomide SUN needs to be adjusted. Depending on the results of the blood tests, your doctor may adjust the dose for the next cycle.
How to take Temozolomide SUN
Take the dose of Temozolomide SUN that your doctor has prescribed for you once a day, preferably at the same time each day.
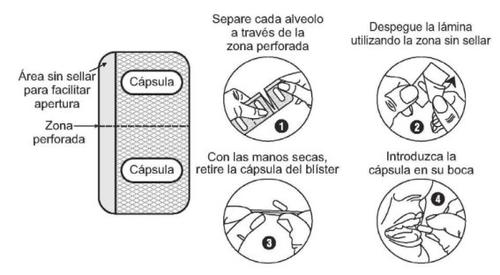
Take the capsules on an empty stomach, for example, at least one hour before breakfast. Swallow the capsule(s) whole with a glass of water. Do not open, crush, or chew the capsules. If a capsule is damaged, avoid contact of the powder with your skin, eyes, or nose. If you accidentally get it in your eyes or nose, rinse the area with water.
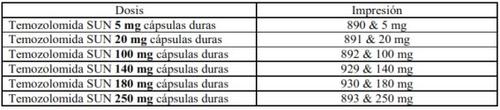
Depending on the dose that you have been prescribed, you may need to take more than one capsule at a time. You may need to take different amounts of the active ingredient to reach the required dose. The marking on the capsule is different for each dose (see table below).
You must make sure you understand and remember the following:
- the number of capsules you should take each day. Ask your doctor or pharmacist to write it down for you (including the imprint on the capsules)
- which days you should take the medicine.
Check the dose with your doctor each time you start a new cycle, as it may be different from the last cycle.
Take Temozolomide SUN exactly as your doctor has told you. It is very important that you talk to your doctor or pharmacist if you are not sure. Taking this medicine in the wrong way can have serious consequences for your health.
If you take more Temozolomide SUN than you should
If you accidentally take more capsules of Temozolomide SUN than you should, contact your doctor or pharmacist or nurse immediately.
If you forget to take Temozolomide SUN
Take the missed dose as soon as possible on the same day. If a whole day has passed, talk to your doctor. Do not take a double dose to make up for a missed dose, unless your doctor tells you to.
If you have any questions about the use of this medicine, ask your doctor, pharmacist, or nurse.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people will suffer from them.
Consult your doctor immediatelyif you experience any of the following side effects:
- severe allergic reaction with hypersensitivity (hives, wheezing, or difficulty breathing)
- uncontrolled bleeding
- seizures (convulsions)
- fever
- chills
- severe headache that does not go away.
Treatment with Temozolomida SUN may cause a decrease in the number of certain types of blood cells. This can make you more prone to bruising or bleeding, anemia (shortage of red blood cells), fever, as well as reduce your resistance to infections. The decrease in blood cells usually occurs during a short period of time. In some cases, it may be prolonged and cause a very strong type of anemia (aplastic anemia). Your doctor will perform regular blood tests to detect any changes that may occur and decide if you need specific treatment. In some cases, the dose may be reduced or treatment with Temozolomida SUN may be suspended.
Adverse effects observed in clinical trials
Temozolomida SUN in combination with radiotherapy in newly diagnosed glioblastoma
Patients receiving treatment with Temozolomida SUN along with radiotherapy may experience some of the adverse effects suffered by patients who only receive treatment with Temozolomida SUN. The following side effects may occur, which may require medical attention.
Very common (may affect more than 1 in 10 people):loss of appetite, headache, constipation (difficulty evacuating), nausea (discomfort), vomiting, skin rash, hair loss, fatigue.
Common (may affect up to 1 in 10 people):oral infections, wound infections, decrease in the number of blood cells (neutropenia, thrombocytopenia, lymphopenia, leucopenia), increased blood sugar, weight loss, change in mental state or alertness, anxiety/depression, drowsiness, difficulty speaking, balance disturbance, dizziness, confusion, memory loss, difficulty concentrating, inability to fall asleep or stay asleep, tingling sensation, bruising, tremors, abnormal or blurred vision, double vision, hearing problems, shortness of breath, cough, blood clots in the legs, fluid retention, swollen legs, diarrhea, stomach or abdominal pain, heartburn, stomach discomfort, difficulty swallowing, dry mouth, skin irritation or redness, dry skin, itching, muscle weakness, joint pain, muscle pain, frequent urination, difficulty retaining urine, allergic reaction, fever, radiation injury, facial swelling, pain, altered taste, altered liver function tests.
Uncommon (may affect up to 1 in 100 people):flu-like symptoms, red spots under the skin, low potassium levels in the blood, weight gain, mood changes, hallucinations, and memory loss, partial paralysis, loss of coordination, altered sensations, partial loss of vision, dry or painful eyes, deafness, middle ear infection, ringing in the ears, ear pain, palpitations (feeling the heartbeat), blood clots in the lungs, high blood pressure, pneumonia, sinusitis, bronchitis, flu or cold, stomach swelling, difficulty controlling bowel movements, hemorrhoids, skin peeling, increased sensitivity of the skin to sunlight, changes in skin color, increased sweating, muscle damage, back pain, difficulty urinating, vaginal bleeding, sexual impotence, absence or heavy menstrual periods, vaginal irritation, breast pain, hot flashes, chills, tongue discoloration, change in sense of smell, thirst, and dental changes.
Monotherapy with Temozolomida SUN in recurrent or progressive glioma
The following adverse effects may occur, which may require medical attention.
Very common (may affect more than 1 in 10 people):decrease in the number of blood cells (neutropenia or lymphopenia, thrombocytopenia), loss of appetite, headache, vomiting, nausea (discomfort), constipation (difficulty evacuating), fatigue.
Common (may affect up to 1 in 10 people):weight loss, tendency to sleep, dizziness, tingling sensation, difficulty breathing, diarrhea, abdominal pain, stomach pain, skin rash, itching, hair loss, fever, weakness, chills, discomfort, pain, altered taste.
Uncommon (may affect up to 1 in 100 people):decrease in the number of blood cells (pancytopenia, anemia, leucopenia).
Rare (may affect up to 1 in 1,000 people):cough, infections including pneumonia.
Very rare (may affect up to 1 in 10,000 people):skin redness, hives (rash), skin rash, allergic reactions.
Other adverse effects
There have been frequent reports of elevated liver enzymes. There have been infrequent reports of increased bilirubin, bile flow problems (cholestasis), hepatitis, liver damage, including fatal liver failure.
Very rare cases of severe skin rash with swelling of the skin, even on the palms of the hands and soles of the feet, or painful redness of the skin or blisters on the body or in the mouth have been observed. Consult your doctor immediatelyif this occurs.
Very few adverse effects have been observed in the lungs as a result of Temozolomida SUN. Patients usually present with difficulty breathing and cough. Consult your doctor if you notice any of these symptoms.
In very rare cases, patients being treated with Temozolomida SUN and similar medications may have a minimal risk of developing a secondary cancer, such as leukemia.
Infrequent cases of new or recurrent infections (reactivations) due to cytomegalovirus and reactivated hepatitis B virus infections have been reported. Infrequent cases of brain infections caused by the herpes virus (herpetic meningoencephalitis), including fatal cases, have been reported. Infrequent cases of sepsis (when bacteria and their toxins circulate in the blood and start damaging organs) have been reported.
Infrequent cases of diabetes insipidus have been reported. The symptoms of diabetes insipidus include frequent urination and thirst.
Reporting of adverse effects
If you experience any type of adverse effect, consult your doctor, pharmacist, or nurse, even if it is a possible adverse effect that is not listed in this prospectus. You can also report them directly through the national reporting system included in Appendix V. By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Storage of Temozolomida SUN
Keep this medicine out of the sight and reach of children, preferably in a locked cabinet. Accidental ingestion can cause death in children.
Do not use this medicine after the expiration date that appears on the label and packaging. The expiration date is the last day of the month indicated.
Do not store above 25°C.
Consult your pharmacist if you notice any change in the appearance of the capsules.
Medicines should not be thrown away through the drain or into the trash. Ask your pharmacist how to dispose of the packaging and medicines that are no longer needed. This will help protect the environment.
6. Package contents and additional information
Composition of Temozolomida SUN
- The active ingredient is temozolomide. Each hard capsule contains 20 mg of temozolomide.
- The other ingredients are:
capsule content:lactose, sodium starch glycolate (Type B), tartaric acid, stearic acid (see section 2 "Temozolomida SUN contains lactose")
capsule shell:gelatin, titanium dioxide (E171), sodium lauryl sulfate
printing ink:shellac, propylene glycol, yellow iron oxide (E172).
Appearance of Temozolomida SUN and package contents
Temozolomida SUN 20 mg hard gelatin capsules have a white opaque cap and body and are printed with yellow ink. The cap is printed with '891'. The body is printed with '20 mg' and two lines.
The hard capsules are available in blisters containing 5 capsules. For the 20-capsule presentations, 4 blisters of 5 capsules will be included in a box.
Only some pack sizes may be marketed.
Marketing authorization holder and manufacturer
Sun Pharmaceutical Industries Europe B.V.
Polarisavenue 87
2132 JH Hoofddorp
Netherlands
You can request more information about this medicine by contacting the local representative of the marketing authorization holder.
België/Belgique/Belgien/????????/Ceská republika/
Danmark/Eesti/Ελλ?δα/Hrvatska/Ireland/Ísland/
Κ?προς/Latvija/Lietuva/Luxembourg/Luxemburg/Magyarország/
Malta/Nederland/Norge/Österreich/Portugal/
Slovenija/Slovenská republika/Suomi/Finland/Sverige
Sun Pharmaceutical Industries Europe B.V.
Polarisavenue 87
2132 JH Hoofddorp
Nederland/Pays-Bas/Niederlande/???????????/Nizozemsko/
Nederlandene/Holland/Ολλανδ?α/Nizozemska/The Netherlands/Holland/
Ολλανδ?α/Niderlande/Nyderlandai/Pays-Bas/Niederlande/Hollandia/
L-Olanda/Nederland/Nederland/Niederlande/Países Baixos/
Nizozemska/Holandsko/Alankomaat/Nederländerna/Nederländerna
Tel./???./tlf./τηλ./Sími/τηλ./Tlf./Puh./
+31 (0)23 568 5501
Deutschland
Sun Pharmaceuticals Germany GmbH
Hemmelrather Weg 201
51377 Leverkusen
Deutschland
tel. +49 214 403 990
España
Laboratorios Ranbaxy S.L.
Passeig de Gràcia, 9
08007 Barcelona
España
tel. +34 93 342 78 90
France
Ranbaxy Pharmacie Generiques
11-15, Quai de Dion Bouton
92800 Puteaux
France
Tel. +33 1 41 44 44 50
Italia
Ranbaxy Italia S.p.A.
Viale Giulio Richard, 1
20143 – Milano
Italia
tel. +39 02 33 49 07 93
Polska
Ranbaxy (Poland) Sp. Z o. o.
ul. Kubickiego 11
02-954 Warszawa
Polska
Tel. +48 22 642 07 75
România
Terapia S.A.
Str. Fabricii nr 124
Cluj-Napoca, Judetul Cluj
România
Tel. +40 (264) 501 500
United Kingdom
Ranbaxy UK Ltd
a Sun Pharma Company
Millington Road 11
Hyde Park, Hayes 3
5th Floor
UB3 4AZ HAYES
United Kingdom
tel. +44 (0) 208 848 8688
Date of the last revision of this prospectus:
Other sources of information
Detailed information about this medicine is available on the European Medicines Agency website: http://www.ema.europa.eu.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to TEMOZOLOMIDE SUN 20 mg HARD CAPSULESDosage form: CAPSULE, 100 mgActive substance: temozolomideManufacturer: Merck Sharp & Dohme B.V.Prescription requiredDosage form: CAPSULE, 100 mgActive substance: temozolomideManufacturer: Merck Sharp & Dohme B.V.Prescription requiredDosage form: CAPSULE, 140 mgActive substance: temozolomideManufacturer: Merck Sharp & Dohme B.V.Prescription required
Online doctors for TEMOZOLOMIDE SUN 20 mg HARD CAPSULES
Discuss questions about TEMOZOLOMIDE SUN 20 mg HARD CAPSULES, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






