
TECARTUS 0.4 - 2 x 10⁸ CELLS FOR INFUSION

How to use TECARTUS 0.4 - 2 x 10⁸ CELLS FOR INFUSION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
Tecartus 0.4 – 2 × 108cell dispersion for infusion
autologous anti-CD19 CD3+ cells (viable CAR+ T cells)
This medicine is subject to additional monitoring, which will allow for quick identification of new safety information. You can help by reporting any side effects you may get. The last section of the leaflet includes information on how to report side effects.
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- Your doctor will give you a patient information card. Read it carefully and follow the instructions.
- Always show the patient information card to the doctor or nurse who treats you or if you go to hospital.
- If you have any further questions, ask your doctor or nurse.
- If you get any side effects, talk to your doctor or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Tecartus and what is it used for
- What you need to know before you are given Tecartus
- How Tecartus is given
- Possible side effects
- Storage of Tecartus
- Contents of the pack and other information
1. What is Tecartus and what is it used for
Tecartus is a gene therapy medicine used to treat mantle cell lymphoma in adults. It is used when other medicines are no longer effective for your treatment (refractory or relapsed mantle cell lymphoma). This medicine is prepared specifically for you from your own modified white blood cells, known as autologous anti-CD19 CD3+ cells.
Mantle cell lymphoma is a cancer that affects part of the immune system (the body's defences). This cancer affects a type of white blood cell called B lymphocytes. In mantle cell lymphoma, B lymphocytes grow out of control and accumulate in the lymph tissue, bone marrow or blood.
How Tecartus works
Your white blood cells are taken from your blood and genetically modified so that they can target the cancer cells in your body. When you are given the Tecartus infusion in your blood, the modified white blood cells will destroy the cancer cells.
2. What you need to know before you are given Tecartus
Tecartus will not be given to you
- if you are allergic to any of the other ingredients of this medicine (listed in section 6). If you think you may be allergic, ask your doctor for advice.
- if you cannot receive the medicine to reduce the number of white blood cells in your blood (lymphodepletion chemotherapy) (see also section 3, ‘How Tecartus is given’).
Warnings and precautions
Tecartus is prepared from your own white blood cells and should only be given to you (autologous use).
Tests and checks
Before you are given Tecartus, your doctor will:
- check your lungs, heart and kidneys and check your blood pressure.
- look for signs of infection or inflammation and decide if you need treatment before you are given Tecartus.
- check if your cancer is getting worse.
- look for signs of graft-versus-host disease that can occur after a transplant. This happens when the transplanted cells attack your body, causing symptoms such as rash, nausea, vomiting, diarrhoea and bloody stools.
- check your uric acid and the number of cancer cells in your blood. This will show if you are likely to develop a complication called tumour lysis syndrome. You may be given medicines to help prevent this complication.
- check if you have hepatitis B, hepatitis C or HIV infection.
- check if you have been vaccinated in the last 6 weeks or if you are planned to receive a vaccine in the coming months.
- check if you have previously received treatment that targets the protein called CD19.
Sometimes, it may not be possible to give the planned treatment with Tecartus. If the infusion of Tecartus is delayed for more than 2 weeks after you received lymphodepletion chemotherapy, you may need to receive more chemotherapy (see also section 3, ‘How Tecartus is given’).
After you are given Tecartus
If you notice any of the following symptoms, tell your doctor or nurse immediately or seek urgent medical attention:
- chills, extreme tiredness, weakness, dizziness, headache, cough, difficulty breathing, fast or irregular heart rate, severe nausea, vomiting or diarrhoea; these can be symptoms of a complication called cytokine release syndrome. Take your temperature twice a day for 3 to 4 weeks after treatment with Tecartus. If your temperature is high, contact your doctor immediately.
- seizures, tremors or difficulty speaking or slurred speech, loss of consciousness or decreased level of consciousness, confusion and disorientation, loss of balance or coordination.
- fever (e.g. temperature over 38 °C), which can be a sign of infection.
- extreme tiredness, weakness and difficulty breathing, which can be symptoms of low red blood cell counts.
- bleeding or bruising easily, which can be symptoms of low platelet counts.
If any of the above applies to you (or you are not sure), talk to your doctor or nurse.
Your doctor will check your blood counts frequently as the number of blood cells and other components of the blood may decrease.
You will be asked to register in a registry for at least 15 years to better understand the long-term effects of Tecartus.
Do not donate blood, organs, tissues or cells for transplants.
Children and adolescents
Tecartus should not be given to children and adolescents under 18 years of age.
Other medicines and Tecartus
Tell your doctor or nurse if you are taking, have recently taken or might take any other medicines.
Before you are given Tecartus, tell your doctor or nurse if you are taking any medicine that weakens the immune system, such as corticosteroids, as these medicines may interfere with the effect of Tecartus.
You should not be given certain vaccines called live vaccines, in particular:
- in the 6 weeks before you receive the short course of lymphodepletion chemotherapy to prepare your body for the Tecartus cells.
- during treatment with Tecartus.
- after treatment while your immune system is recovering.
Ask your doctor if you need any vaccine.
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor for advice before being given this medicine. This is because the effects of Tecartus on pregnant or breast-feeding women are not known, and it may harm the unborn child or baby.
- a pregnancy test will be performed before you start treatment. Tecartus should only be given if the results show you are not pregnant.
Talk to your doctor about pregnancy if you received Tecartus.
Driving and using machines
Tecartus may cause problems such as altered consciousness or decreased consciousness, confusion and seizures (convulsions) in the 8 weeks after administration.
Do not drive, do not use machines or engage in activities that require heavy concentration for at least 8 weeks after treatment with Tecartus or until your doctor confirms that you have fully recovered.
Tecartus contains sodium, dimethyl sulfoxide (DMSO) and gentamicin
This medicine contains 300 mg of sodium (main component of cooking/table salt) in each infusion. This is equivalent to 15 % of the maximum recommended daily intake of sodium for an adult. It also contains DMSO and gentamicin, which may cause severe hypersensitivity reactions.
3. How Tecartus is given
Tecartus will always be given to you by a healthcare professional.
- since Tecartus is prepared from your own white blood cells, your cells will be collected to prepare your medicine. Your doctor will take some of your blood with a catheter placed in a vein (a procedure called leukaapheresis). Some white blood cells will be separated from the blood and the rest of the blood will be returned to the vein. This may take 3 to 6 hours and may need to be repeated.
- your white blood cells will be sent to a manufacturing site to make Tecartus. It usually takes 2 to 3 weeks to make Tecartus, but the time may vary.
Medicines given before treatment with Tecartus
a few days before you receive Tecartus, you will be given lymphodepletion chemotherapy, which will allow the modified white blood cells in Tecartus to multiply in your body once you are given the medicine.
during the 30 to 60 minutes before you are given Tecartus, you may be given other medicines. This is to help prevent infusion reactions and fever. These other medicines may include:
- paracetamol.
- an antihistamine such as diphenhydramine.
How Tecartus is given
Tecartus will always be given to you by a doctor in a qualified medical centre.
- Tecartus is given as a single dose.
- your doctor or nurse will give you a single infusion of Tecartus through a catheter placed in a vein (intravenous infusion) over about 30 minutes.
- Tecartus is your modified white blood cells. The healthcare professional handling the treatment will therefore take necessary precautions (wear gloves and goggles) to avoid possible transmission of infectious diseases and will follow local guidelines for the treatment of human origin waste for cleaning and disposal of any material that has come into contact with the treatment.
After you are given Tecartus
- you should stay near the hospital where you were treated for at least 4 weeks after treatment with Tecartus. Your doctor will recommend that you return to the hospital daily for at least 10 days or that you stay in hospital for the first 10 days after treatment with Tecartus. This is so that your doctor can check if your treatment is working and help you if you have any side effects.
4. Possible side effects
like all medicines, this medicine can cause side effects, although not everybody gets them. do not try to treat the side effects yourself.
Tecartus may cause side effects that can be serious or life-threatening. get urgent medical attentionif you experience any of the following side effects after the infusion of Tecartus.
very common: may affect more than 1 in 10 people
- fever, chills, low blood pressure that can cause symptoms such as dizziness, fainting, fluid accumulation in the lungs that can be severe and life-threatening (all of these are symptoms of a complication called cytokine release syndrome).
- loss of consciousness or decreased level of consciousness, confusion or memory loss due to brain function disorders, difficulty speaking or slurred speech, involuntary shaking (tremors), seizures (convulsions), sudden confusion with agitation, disorientation, hallucinations or irritability (delirium).
- fever, chills, which can be signs of infection.
other possible side effects
the following are other side effects. tell your doctor immediately if these side effects become severe or serious.
very common: may affect more than 1 in 10 people
- abnormally low number of white blood cells, which can increase the risk of infection.
- low number of cells that help blood to clot (thrombocytopenia), disorder of blood clotting: symptoms can include excessive or prolonged bleeding or bruising.
- high blood pressure.
- low number of red blood cells (the cells that carry oxygen): symptoms can include extreme tiredness with lack of energy.
- extreme tiredness.
- fast or slow heart rate.
- decrease in the level of oxygen that reaches the body tissues: symptoms can include changes in skin colour, confusion and rapid breathing.
- difficulty breathing, cough.
- nausea, constipation, diarrhoea, abdominal pain, vomiting, difficulty swallowing.
- muscle pain, joint pain, bone pain, pain in the limbs.
- lack of energy or strength, muscle weakness, difficulty moving, muscle spasms.
- headache.
- kidney problems that cause fluid accumulation in your body, fluid accumulation in the tissues (oedema) that can cause weight gain, difficulty breathing and decreased urine output.
- high levels of uric acid in the blood tests.
- low levels of sodium, phosphate, potassium or calcium in the blood tests.
- decreased appetite, mouth pain.
- difficulty sleeping, anxiety.
- swelling in the limbs, fluid accumulation around the lungs (pleural effusion).
- skin rash.
- low levels of immunoglobulins in the blood tests, which can lead to infections.
- increased levels of liver enzymes in the blood tests.
- blood clots: symptoms can include chest pain or upper back pain, difficulty breathing, coughing up blood or pain with cramps, swelling in only one leg, dark and warm skin around the painful area.
- nerve pain.
common: may affect up to 1 in 10 people
- low levels of albumin in the blood tests.
- excessive bleeding.
- irregular heart rate (arrhythmia).
- loss of control of body movements.
- dry mouth, dehydration.
- shortness of breath (respiratory failure).
- difficulty breathing that prevents you from speaking in full sentences and cough due to fluid accumulation in the lungs.
- increased intracranial pressure.
reporting of side effects
5. Storage of Tecartus
this information is intended only for healthcare professionals.
keep this medicine out of the sight and reach of children.
do not use this medicine after the expiry date which is stated on the container label and infusion bag after exp.
store in the vapour phase of liquid nitrogen ≤ -150 °c until time of thawing for use.
do not re-freeze.
this medicine contains genetically modified human blood cells. local guidelines for the treatment of human origin waste should be followed for the disposal of unused medicine or waste. this medicine will be given to you by qualified healthcare professionals, who will be responsible for the correct disposal of the product. this will help to protect the environment.
6. Container contents and additional information
Composition of Tecartus
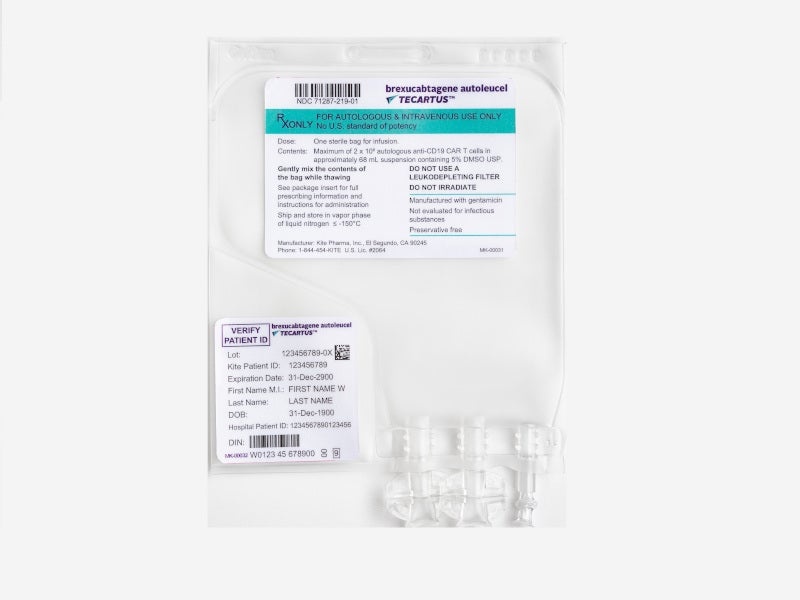
The active substance is autologous CD3+ cells transduced with anti-CD19. Each patient-specific infusion bag contains a dispersion of anti-CD19 CAR T cells in approximately 68 ml, for a target dose of 2 x 10^6 viable anti-CD19-positive CAR T cells/kg. The other components (excipients) are: Cryostor CS10, sodium chloride, human albumin. See section 2 "Tecartus contains sodium".
Appearance and container contents of the product
Tecartus is a transparent to opaque, white to red dispersion for infusion, supplied in a single patient-specific infusion bag enclosed in a metal container. One infusion bag contains approximately 68 ml of cell dispersion.
Marketing authorisation holder
Kite Pharma EU B.V.
Tufsteen 1
2132 NT Hoofddorp
Netherlands
Manufacturer
Kite Pharma EU B.V.
Tufsteen 1
2132 NT Hoofddorp
Netherlands
For further information about this medicinal product, please contact the local representative of the marketing authorisation holder:
Belgium/Belgique/Belgien Gilead Sciences Belgium SRL-BV Tel: + 32 (0) 24 01 35 50 | Lithuania Gilead Sciences Poland Sp. z o.o. Tel: + 48 22 262 8702 |
Greece Gilead Sciences Ireland UC Tel: + 353 (0) 1 686 1888 | Luxembourg/Luxemburg Gilead Sciences Belgium SRL-BV Tel: + 32 (0) 24 01 35 50 |
Czech Republic Gilead Sciences s.r.o. Tel: + 420 910 871 986 | Hungary Gilead Sciences Ireland UC Tel: + 353 (0) 1 686 1888 |
Denmark Gilead Sciences Sweden AB Tel: + 46 (0) 8 5057 1849 | Malta Gilead Sciences Ireland UC Tel: + 353 (0) 1 686 1888 |
Germany Gilead Sciences GmbH Tel: + 49 (0) 89 899890-0 | Netherlands Gilead Sciences Netherlands B.V. Tel: + 31 (0) 20 718 36 98 |
Estonia Gilead Sciences Poland Sp. z o.o. Tel: + 48 22 262 8702 | Norway Gilead Sciences Sweden AB Tel: + 46 (0) 8 5057 1849 |
Greece Gilead Sciences Ελλάς Μ.ΕΠΕ. Tel: + 30 210 8930 100 | Austria Gilead Sciences GesmbH Tel: + 43 1 260 830 |
Spain Gilead Sciences, S.L. Tel: + 34 91 378 98 30 | Poland Gilead Sciences Poland Sp. z o.o. Tel: + 48 22 262 8702 |
France Gilead Sciences Tel: + 33 (0) 1 46 09 41 00 | Portugal Gilead Sciences, Lda. Tel: + 351 21 7928790 |
Croatia Gilead Sciences Ireland UC Tel: + 353 (0) 1 686 1888 | Romania Gilead Sciences Ireland UC Tel: + 353 (0) 1 686 1888 |
Ireland Gilead Sciences Ireland UC Tel: + 353 (0) 214 825 999 | Slovenia Gilead Sciences Ireland UC Tel: + 353 (0) 1 686 1888 |
Iceland Gilead Sciences Sweden AB Tel: + 46 (0) 8 5057 1849 | Slovakia Gilead Sciences Slovakia s.r.o. Tel: + 421 232 121 210 |
Italy Gilead Sciences S.r.l. Tel: + 39 02 439201 | Finland Gilead Sciences Sweden AB Tel: + 46 (0) 8 5057 1849 |
Cyprus Gilead Sciences Ελλάς Μ.ΕΠΕ. Tel: + 30 210 8930 100 | Sweden Gilead Sciences Sweden AB Tel: + 46 (0) 8 5057 1849 |
Latvia Gilead Sciences Poland Sp. z o.o. Tel: + 48 22 262 8702 | United Kingdom Gilead Sciences Ltd Tel: + 44 (0) 8000 113700 |
Date of last revision of this leaflet:
This medicinal product has been authorised with a "conditional approval".
This type of approval means that more information on this medicinal product is expected. The European Medicines Agency will review any new information on this medicinal product at least once a year and this leaflet will be updated as necessary.
Other sources of information
Detailed information on this medicinal product is available on the European Medicines Agency website: http://www.ema.europa.eu. There are also links to other websites on rare diseases and orphan medicines.
This leaflet can be found in all EU/EEA languages on the European Medicines Agency website.
<------------------------------------------------------------------------------------------------------------------------>
This information is intended for healthcare professionals only:
It is important to read all the content related to this procedure before administering Tecartus. Precautions to be taken before handling or administering the medicinal product
- Tecartus contains genetically modified cells. Local guidelines for the handling of human-derived material should be followed for these medicinal products.
- In the administration centre, Tecartus should be transported in closed, breakage-proof and leak-proof containers.
- Tecartus is prepared from the patient's autologous blood collected by leukaapheresis. The patient's leukaapheresis material and Tecartus may pose a risk of transmission of infectious viruses to healthcare professionals (HCPs) handling the product. Therefore, HCPs handling the leukaapheresis material or Tecartus should take necessary precautions (wear gloves and goggles) to avoid possible transmission of infectious diseases.
Infusion preparation
- Check that the patient's identification (ID) matches the patient identifiers on the Tecartus metal container.
- Do not remove the infusion bag from the metal container if the patient-specific label information does not match the patient to be treated.
- Once the patient's ID has been confirmed, remove the infusion bag from the metal container.
- Check that the patient information on the metal container label matches that on the infusion bag label.
- Inspect the infusion bag for container integrity before thawing. If the bag is damaged, follow local guidelines for the handling of human-derived waste material (or contact Kite immediately).
- Place the infusion bag in a secondary bag.
- Thaw Tecartus at a temperature of approximately 37 °C, either by water bath or dry thawing, until no ice is visible in the infusion bag. Gently mix the contents of the bag to eliminate cellular aggregates. If cellular aggregates are still visible, continue to gently mix the contents of the bag. Small cellular aggregates should be eliminated by gentle manual mixing. Tecartus should not be washed, centrifuged and/or resuspended in a new medium before infusion. Thawing will take approximately 3 to 5 minutes.
- Once thawed, Tecartus is stable at room temperature (20 °C-25 °C) for up to 3 hours. However, infusion should be started within 30 minutes of complete thawing.
DO NOT use a leucodepletion filter.
Administration
- This medicinal product should be administered in a qualified medical centre by one or more physicians with experience in the treatment of haematological malignancies and who have received training on the administration and treatment of patients treated with Tecartus.
- Ensure that at least one dose of tocilizumab per patient and an emergency kit are available before infusion and during the recovery period. Hospitals and associated centres should have access to an additional dose of tocilizumab within 8 hours of each previous dose.
- Check that the patient's identity matches the patient identifiers on the infusion bag.
- Tecartus is intended for autologous use only.
- Tecartus should be administered as an intravenous infusion using latex-free intravenous lines and without a leucodepletion filter over a period of 30 minutes, either by gravity or using a peristaltic pump.
- During infusion, gently agitate the bag to prevent the formation of cellular aggregates. The entire contents of the infusion bag should be administered.
- Prior to infusion, use a sterile sodium chloride 9 mg/ml (0.9%) solution for injection to prime the lines, as well as to flush the lines after infusion. Once the total volume of Tecartus has been infused, flush the infusion bag with 10 to 30 ml of a sodium chloride 9 mg/ml (0.9%) solution for injection by reverse priming to ensure that as many cells as possible are infused into the patient.
Disposal of Tecartus
- All unused medicinal products or waste materials that have come into contact with Tecartus (solid and liquid waste) should be disposed of in accordance with local guidelines for the handling of human-derived waste material. Work surfaces and materials that may have come into contact with Tecartus should be decontaminated with a suitable disinfectant.
Accidental exposure
- Accidental exposure to Tecartus should be avoided. In the event of accidental exposure, local guidelines for the handling of human-derived material should be followed, which may include washing the contaminated skin and removing contaminated clothing.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to TECARTUS 0.4 - 2 x 10⁸ CELLS FOR INFUSIONDosage form: INJECTABLE PERFUSION, 260 - 500 × 10^6 cellsActive substance: idecabtagene vicleucelManufacturer: Bristol-Myers Squibb Pharma EeigPrescription requiredDosage form: INJECTABLE PERFUSION, 1.1-70x10^6/1.1-70x10^6 cells/mlActive substance: lisocabtagene maraleucelManufacturer: Bristol-Myers Squibb Pharma EeigPrescription requiredDosage form: INJECTABLE PERFUSION, 3.2 x 10^6 - 1 x 10^8 cellsActive substance: ciltacabtagene autoleucelManufacturer: Janssen-Cilag International N.VPrescription required
Online doctors for TECARTUS 0.4 - 2 x 10⁸ CELLS FOR INFUSION
Discuss questions about TECARTUS 0.4 - 2 x 10⁸ CELLS FOR INFUSION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






