
SEVORANE 100% LIQUID FOR INHALATION

How to use SEVORANE 100% LIQUID FOR INHALATION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
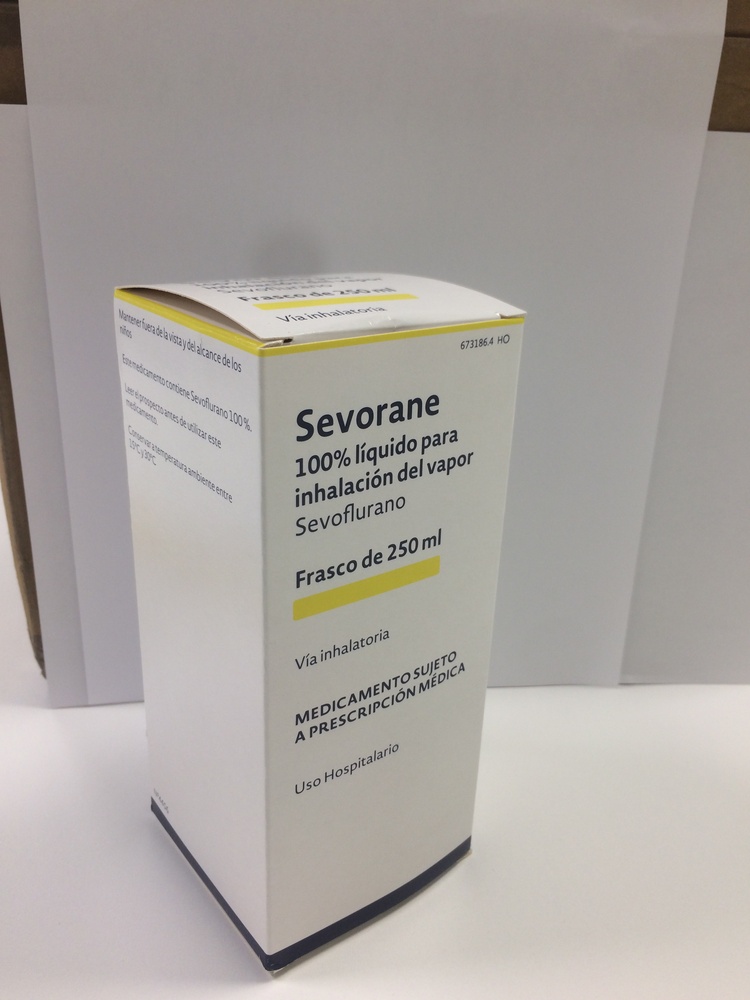
SEVORANE
100% Liquid for Inhalation Vapor
Sevoflurane
Read the entire package leaflet carefully before starting to use this medication, as it contains important information for you.
- Keep this package leaflet, as you may need to read it again. If you have any questions, ask your doctor, pharmacist, or nurse.
- This medication has been prescribed to you and should not be given to others, even if they have the same symptoms, as it may harm them.
- If you experience side effects, consult your doctor, pharmacist, or nurse, even if they are side effects not listed in this package leaflet. See section 4.
Contents of the Package Leaflet:
- What is SEVORANE and what is it used for
- What you need to know before starting to use SEVORANE
- How to use SEVORANE
- Possible side effects
- Storage of SEVORANE
- Package Contents and Additional Information
1. What is SEVORANE and what is it used for
SEVORANE is an inhalation anesthetic that belongs to the group of halogenated hydrocarbons.
SEVORANE is used for the induction and maintenance of general anesthesia in adults and children, both inpatient and outpatient.
2. What you need to know before starting to use SEVORANE
Do not use SEVORANE,
- If you are allergic to sevoflurane or any of the other components of this medication (listed in section 6) or to other halogenated anesthetics.
- If you are susceptible to malignant hyperthermia
- If you have been informed that you should not undergo general anesthesia.
Warnings and Precautions
Consult your doctor, pharmacist, or nurse before starting to use SEVORANE.
- It should be administered via or under the supervision of personnel trained in the administration of general anesthetics, with adequate facilities for airway maintenance, artificial ventilation, and additional oxygen and circulatory resuscitation.
- The exact concentration of sevoflurane being released from the vaporizer must be known. As volatile anesthetics differ in their physical properties, only vaporizers specifically calibrated for sevoflurane can be used. The administration of general anesthesia must be individualized based on the patient's response.
- As anesthesia becomes deeper, there is a greater decrease in blood pressure and respiratory depression.
- If you are sensitive to malignant hyperthermia, it could trigger an increase in skeletal muscle metabolism, producing a high need for oxygen, hypercapnia (increased carbon dioxide in the blood), and may include muscle rigidity, rapid pulse (tachycardia), altered breathing, bluish discoloration of the skin, altered heart rhythm (arrhythmias), and/or unstable blood pressure. During superficial anesthesia, other signs may appear: acute hypoxia (sudden decrease in oxygen in the body), hypercapnia (increased carbon dioxide in the blood), and hypovolemia (decrease in circulating blood volume).
- In clinical trials, a case of malignant hyperthermia was reported. Additionally, there have been post-marketing reports of malignant hyperthermia. Some of these reports have been fatal.
- Treatment of malignant hyperthermia includes discontinuation of SEVORANE and administration of sodium dantrolene intravenously.
- Rarely, cardiac arrhythmias (irregular heartbeat) and death have occurred in children during the postoperative period, mainly in patients with diseases affecting the nervous system and muscles (such as Duchenne muscular dystrophy) and in many cases with the concomitant administration of other medications that act at this level (succinylcholine).
- If you have heart problems, a type of tachycardia may occur that your doctor will need to treat, as it can be fatal in exceptional cases.
- In pediatric patients with Pompe disease, isolated cases of ventricular arrhythmia have been reported.
- Caution should be exercised when administering general anesthesia, including when using SEVORANE, to patients with mitochondrial disorders.
- After marketing, rare cases of moderate to severe liver disease or hepatitis (inflammation of the liver) with or without jaundice (yellowing of the skin and eyes) have been seen.
- When SEVORANE is used in patients with pre-existing liver disease or in treatment with medications known to cause liver damage, the doctor must decide whether to use it or not.
- If you are repeatedly exposed to halogenated hydrocarbons, including SEVORANE, in a relatively short interval, your risk of liver damage may increase.
- The decrease in blood pressure is related to the concentration of SEVORANE and the depth of anesthesia. Special caution should be exercised in patients with lower than usual blood pressure, in patients with lower blood volume, or others with problems of this type caused, for example, by other medications.
- As with all anesthetics, it is essential to maintain stable blood pressure and blood volume to avoid myocardial ischemia (obstruction of blood flow to the heart muscle) in patients with coronary artery disease.
- The recovery from general anesthesia should be carefully evaluated before leaving the recovery room.
- Although recovery of consciousness after SEVORANE administration usually occurs within minutes, the impact on intellectual function during the 2 or 3 days following anesthesia has not been studied. As with other anesthetics, small mood changes may persist for several days after administration.
- If you have kidney function damage.
- If you are at risk of increased intracranial pressure.
- The use of SEVORANE has been associated with seizures that have appeared in young people and adults with or without predisposing risk factors. The anesthesiologist will judge whether to use this medication or not in cases where there may be a risk of seizures.
- In children, seizures can occur from 2 years of age. The anesthesiologist will judge whether to use this medication in cases where there may be a risk of seizures.
- The anesthesiologist should adequately replace desiccated CO2 absorbers.
- If you have taken narcotic medications or other medications that may cause respiratory depression, your doctor will monitor your breathing and provide assistance if necessary.
Use in People Over 80 Years Old
If you are an 80-year-old patient, the required dose is approximately half of that required for a 20-year-old.
Use of SEVORANE with Other Medications
Tell your doctor or pharmacist if you are using, have recently used, or may need to use any other medication, especially those used for blood pressure, heart disorders, anxiety, tuberculosis, muscle relaxants, herbal preparations, or alcohol.
Tell your doctor if you are being treated with opioids such as alfentanil and sufentanil, as their combination with SEVORANE may lead to a joint and more significant alteration of heart rhythm, blood pressure, and respiratory frequency.
It is essential to inform your doctor if you are taking or have recently taken any of the following medications:
- Succinylcholine (used as a muscle relaxant during anesthesia): its use in combination with sevoflurane may cause severe cardiac arrhythmias during the postoperative period.
- Non-selective IMAO antidepressants. Treatment with these medications should be suspended 2 weeks before surgery.
- Calcium channel blocker antihypertensives, as there is a risk of hypotension, particularly dihydropyridine derivatives.
- Beta-sympathomimetics (such as isoprenaline) and alpha and beta sympathomimetics (such as epinephrine and norepinephrine): due to the potential risk of ventricular arrhythmias, sevoflurane should be used with caution in combination with these medications.
Pregnancy, Breastfeeding, and Fertility
If you are pregnant or breastfeeding, think you may be pregnant, or plan to become pregnant, consult your doctor or pharmacist before using this medication.
- It should not be used during pregnancy unless clearly necessary.
- It has been used during cesarean section operations. The safety of SEVORANE during the dilation period or vaginal delivery has not been demonstrated. SEVORANE has a relaxing effect on the uterus, with the potential risk of uterine bleeding. The doctor will decide whether to use it or not in these cases.
- It is unknown whether SEVORANE or its metabolites are excreted in breast milk.
- Caution should be exercised when SEVORANE is administered to breastfeeding women.
- No impairment of fertility has been demonstrated in animals treated with SEVORANE.
Driving and Using Machines
Do not drive or operate tools or machines after receiving SEVORANE, as this medication may affect your reaction ability. Your doctor will indicate how long you should wait before driving or using machines again.
3. How to Use SEVORANE
Follow the administration instructions for the medication contained in this package leaflet or as indicated by your doctor, pharmacist, or nurse. If in doubt, ask your doctor, pharmacist, or nurse.
SEVORANE is administered by a healthcare professional properly trained, using a vaporizer specifically calibrated for this product, so that the released concentration can be exactly controlled.
Your doctor will decide what dose of SEVORANE is most suitable for you.
If You Use More SEVORANE Than You Should
If you receive more SEVORANE than you should, the doctor will interrupt the administration and apply the necessary measures.
In case of overdose or accidental ingestion, consult the Toxicology Information Service, phone 91.562.04.20, indicating the medication and the amount ingested.
4. Possible Side Effects
Like all medications, this medication can cause side effects, although not everyone will experience them.
Most side effects are mild or moderate and transient.
Sevoflurane may cause decreases in cardiac and respiratory function.
Nausea and vomiting have been observed in the postoperative period, common sequelae of surgery and general anesthesia, which may be due to inhalation anesthesia, other agents administered during or after the operation, and the patient's response to the surgical procedure.
The most commonly observed side effects are:
In adult patients: decreased blood pressure, nausea, delirium, and vomiting;
In elderly patients: slowing of heart rate, decreased blood pressure, and nausea; and
In children: agitation, cough, vomiting, and nausea.
The following table shows all side effects, at least possibly related to sevoflurane in clinical trials and post-marketing experience, ordered by frequency and classified by MedDRA organ and system classes. The following frequency groups have been used: Very common side effects (in more than 1 in 10 people); Common side effects (between 1 and 10 in 100 people); Uncommon side effects (between 1 and 10 in 1,000 people); Rare side effects (between 1 and 10 in 10,000 people); Very rare side effects (in less than 1 in 10,000 people), including isolated events. Post-marketing adverse reactions are reported voluntarily in a population with unknown exposure frequency. Therefore, it is not possible to estimate the frequency of adverse reactions, and the frequency is "unknown". The type, severity, and frequency of adverse effects in patients who received SEVORANE in clinical trials are comparable to those in patients with reference treatment.
Side Effects from Clinical Trials and Post-Marketing Experience
Organ/System Classification | Frequency | Adverse Reactions |
Immune System Disorders | Unknown | Anaphylactic reaction (severe allergic reaction throughout the body) Anaphylactoid reaction (other type of allergic reaction) Hypersensitivity (allergic reaction) |
Psychiatric Disorders | Very Common | Agitation |
Nervous System Disorders | Common | Somnolence Dizziness Headache |
Cardiac Disorders | Unknown Very Common | Seizure Dystonia (involuntary muscle contractions) Bradycardia (decreased heart rate) |
Common | Tachycardia (increased heart rate) | |
Uncommon | Complete atrioventricular block (heart disorder) | |
Unknown | Cardiac arrest Prolonged QT interval associated with Torsade de Pointes | |
Vascular Disorders | Very Common | Hypotension (lower than usual blood pressure) |
Common | Hypertension (higher than usual blood pressure) | |
Respiratory, Thoracic, and Mediastinal Disorders | Very Common | Cough |
Common | Respiratory disorder Laryngospasm (larynx spasm) | |
Unknown | Bronchospasm (bronchial spasm) Dyspnea (difficulty breathing) Wheezing (whistling sound when breathing) | |
Gastrointestinal Disorders | Very Common | Nausea Vomiting |
Common | Increased salivation | |
Hepatobiliary Disorders | Unknown | Hepatitis (inflammation of the liver) Liver failure (liver malfunction) Liver necrosis (dead liver tissue) |
Skin and Subcutaneous Tissue Disorders | Unknown | Contact dermatitis (skin inflammation due to contact with a substance) Itching Rash Facial swelling Urticaria |
General Disorders and Administration Site Conditions | Common | Chills Pyrexia (elevated body temperature) |
Unknown | Chest discomfort Malignant hyperthermia (see below) | |
Investigations | Common | Abnormal blood glucose Abnormal liver function test Abnormal white blood cell count Increased fluoride |
Injury, Poisoning, and Procedural Complications | Common | Hypothermia (lower than usual body temperature) |
Description of Selected Adverse Reactions
Transient increases in inorganic fluoride levels in the serum may occur during and after anesthesia with SEVORANE. Inorganic fluoride concentrations usually reach their maximum within 2 hours after the end of SEVORANE anesthesia and return to preoperative levels within 48 hours. In clinical trials, elevated fluoride concentrations were not associated with impaired renal function.
There have been rare reports of postoperative hepatitis. Additionally, there have been rare post-marketing reports of liver failure and liver necrosis associated with the use of potent volatile anesthetics, including SEVORANE. However, the actual incidence and the relationship of SEVORANE to these events cannot be established with certainty.
There have been rare reports of hypersensitivity (including contact dermatitis, skin rash, dyspnea, wheezing, chest discomfort, facial swelling, or anaphylactic reaction), particularly in association with long-term professional exposure to inhaled anesthetics, including SEVORANE.
In susceptible individuals, potent inhalation anesthetics can trigger a hypermetabolic state of skeletal muscle, producing a very high demand for oxygen and the clinical syndrome known as malignant hyperthermia.
Pediatric Population
The use of SEVORANE has been associated with seizures. Many of these have appeared in children from 2 years of age and in young people, most of whom did not have risk factors that would predispose them to seizures. A clinical judgment should be made before using SEVORANE in patients who may be at risk of seizures.
Reporting of Side Effects
If you experience any side effects, consult your doctor, pharmacist, or nurse, even if they are side effects not listed in this package leaflet. You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines: https://www.notificaram.es. By reporting side effects, you can contribute to providing more information on the safety of this medication.
5. Storage of SEVORANE
Keep this medication out of sight and reach of children.
It should be stored at room temperature between 15 and 30°C.
Do not use this medication after the expiration date shown on the packaging after CAD.:. The expiration date is the last day of the month indicated.
6. Container Content and Additional Information
Composition of SEVORANE
The active ingredient is sevoflurane. This medication contains 100% sevoflurane.
It contains at least 300 ppm of water as protection against ambient Lewis acid. It does not contain other additives or preservatives.
Product Appearance and Container Content
SEVORANE is presented as a non-flammable volatile liquid in 250 ml amber polyethylene naphthalate containers. The vaporized liquid is administered by inhalation with a specific vaporizer.
Marketing Authorization Holder and Manufacturer
Marketing Authorization Holder:
AbbVie Spain S.L.U. Avenida de Burgos, 91- 28050 Madrid.
Manufacturer:
AbbVie S.r.l., S.R. 148 Pontina km 52 SNC, 04011 Campoverde di Aprilia (LT) Italy.
Date of Last Revision of this Prospectus: February 2016
Detailed information about this medication is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es/
--------------------------------------------------------------------------------------------------------------------
Additional Information for Healthcare Professionals
DOSAGE
Premedication should be selected according to the needs of each patient and at the discretion of the anesthesiologist.
Surgical Anesthesia
Sevoflurane should be administered through a vaporizer specifically calibrated for use with this medication so that the released concentration can be regulated.
The concentration of sevoflurane released by the vaporizer during anesthesia should be known. The dosage should be individualized and adjusted to achieve the desired effect, according to the patient's age and clinical condition.
Induction of Anesthesia
The dose should be individualized and adjusted to achieve the desired effect, according to the patient's age and clinical condition. A short-acting barbiturate or other induction medication may be administered intravenously, followed by inhalation of sevoflurane. Induction of anesthesia may be performed by inhalation of sevoflurane in oxygen (O2) or in combination with an oxygen-nitrous oxide mixture (O2/N2O). For induction of anesthesia, inhaled concentrations of up to 8% sevoflurane typically produce surgical anesthesia in less than 2 minutes, in both adults and children.
Maintenance of Anesthesia
Levels of surgical anesthesia can be maintained with concentrations of 0.5 - 3% sevoflurane in O2 with or without concomitant use of nitrous oxide.
Table 1
MAC (Minimum Alveolar Concentration) Values for Adults and Pediatric Patients by Age
Patient Age (years) | Sevoflurane in oxygen | Sevoflurane in 65%N2O/35%O2 |
0 - 1 month* | 3.3 % | |
1 - < 6 months | 3.0 % | |
6 months- < 3 years | 2.8 % | 2.0@ |
3 – 12 | 2.5 % | |
25 | 2.6 % | 1.4 % |
40 | 2.1 % | 1.1 % |
60 | 1.7 % | 0.9 % |
80 | 1.4 % | 0.7 % |
*Neonates are at term gestational age. MAC values have not been determined in premature infants | ||
@ In pediatric patients 1 to < 3 years, 60% N2O/40% O2 was used |
Recovery
Recovery times after sevoflurane anesthesia are generally short. Therefore, patients may require early treatment for postoperative pain.
Elderly Patients
MAC decreases with age. The mean concentration of sevoflurane required to achieve MAC in an 80-year-old patient is approximately 50% of that required in a 20-year-old patient.
Pediatric Population
Refer to Table 1 for MAC values by age in pediatric patients.
INSTRUCTIONS FOR CORRECT ADMINISTRATION OF THE PREPARATION
Sevoflurane should be administered with a vaporizer specifically calibrated for this product, using a filling system designated for sevoflurane vaporizers or other filling systems for vaporizers.
Replacement of Desiccated CO2Absorbents:
Rare cases of extreme heat, smoke, and/or spontaneous fire in the anesthesia machine during the use of sevoflurane with desiccated CO2 absorbents, specifically those containing potassium hydroxide, have been reported. An unusually delayed increase or unexpected decrease in the inspired concentration of sevoflurane compared to the vaporizer setting may be associated with excessive heating of the CO2 absorbent container.
A exothermic reaction that increases the degradation of sevoflurane and the production of degradation products may occur when the CO2 absorbent becomes desiccated, such as after the passage of dry gas through the CO2 absorbent containers for an extended period. In an experimental anesthesia respiratory circuit using desiccated CO2 absorbents and maximum concentrations of sevoflurane (8%) for prolonged periods (> 2 hours), sevoflurane degradation products (methanol, formaldehyde, carbon monoxide, and compounds A, B, C, and D) were observed. The formaldehyde concentrations observed in the anesthesia respiratory circuit (using absorbents containing sodium hydroxide) were consistent with levels known to cause mild respiratory irritation. The clinical relevance of the degradation products observed in this extreme experimental model is unknown.
When an anesthesiologist suspects that the CO2 absorbent may be desiccated, it should be replaced before administering sevoflurane. The color indicator of many CO2 absorbents does not necessarily change as a result of desiccation. Therefore, the lack of significant color change should not be taken as assurance of adequate hydration. CO2 absorbents should be replaced routinely, regardless of the color of the absorbent indicator.
INTERACTIONS
Beta-sympathomimetic agents, such as isoproterenol, and alpha and beta-sympathomimetic agents, such as epinephrine and norepinephrine, should be used with caution during sevoflurane narcosis due to a potential risk of ventricular arrhythmias.
Non-Selective MAO Inhibitors:
The combination of non-selective MAO inhibitors and sevoflurane should be avoided due to the risk of preoperative collapse. Treatment should be discontinued 2 weeks before surgery.
Calcium Channel Blockers:
Sevoflurane may produce marked hypotension, particularly in combination with dihydropyridine derivatives. Caution should be exercised when using calcium channel blockers concomitantly with inhaled anesthetics, due to the risk of an additive negative inotropic effect.
Succinylcholine:
The simultaneous administration of succinylcholine and inhaled anesthetic agents has been associated with rare cases of increased serum potassium that resulted in cardiac arrhythmias and death during the postoperative period in pediatric patients.
Sevoflurane has been shown to be safe and effective when administered concomitantly with a wide variety of medications frequently used in surgical interventions, such as medications acting on the central and peripheral nervous system, skeletal muscle relaxants, anti-infectious agents including aminoglycosides, hormones, and synthetic substitutes, hemoderivatives, and cardiovascular medications including epinephrine.
Epinephrine/Adrenaline:
Sevoflurane is similar to isoflurane in sensitizing the myocardium to the arrhythmogenic effect produced by exogenous administration of epinephrine.
Indirect-Acting Sympathomimetic Agents:
There is a risk of acute hypertensive episodes with the concomitant use of sevoflurane and indirect-acting sympathomimetic agents (amphetamines, ephedrine).
Beta-Blockers:
Sevoflurane may increase the negative inotropic, chronotropic, and dromotropic effects of beta-blockers by blocking cardiovascular compensatory mechanisms.
Verapamil:
When verapamil and sevoflurane were administered simultaneously, deterioration of atrioventricular conduction was observed.
St. John's Wort:
In patients treated long-term with St. John's Wort, severe hypotension and delayed recovery from anesthesia have been reported after the use of halogenated inhalational anesthetics.
Barbiturates:
The administration of sevoflurane is compatible with the administration of barbiturates commonly used in surgical interventions.
Benzodiazepines and Opioids:
It is expected that the administration of benzodiazepines and opioids will decrease the MAC of sevoflurane, as occurs with other inhaled anesthetics. The administration of sevoflurane is compatible with the administration of benzodiazepines and opioids commonly used in surgical interventions.
When sevoflurane is combined with opioids such as alfentanil and sufentanil, it may lead to a synergistic failure of cardiac rhythm, blood pressure, and respiratory frequency.
CYP2E1 Inducers:
Medications and compounds that increase the activity of the CYP2E1 isoenzyme of cytochrome P450, such as isoniazid and alcohol, may increase the metabolism of sevoflurane and lead to significant increases in plasma fluoride concentrations. The concomitant use of sevoflurane and isoniazid may potentiate the hepatotoxic effects of isoniazid.
Nitrous Oxide:
As with other halogenated volatile anesthetics, the MAC of sevoflurane decreases when administered in combination with nitrous oxide. The equivalent MAC is reduced by 50% in adults and 25% in pediatric patients, approximately.
Neuromuscular Blockers:
As with other inhaled anesthetics, sevoflurane affects the intensity and duration of neuromuscular blockade produced by non-depolarizing muscle relaxants. When administered to supplement anesthesia with alfentanil-N2O, sevoflurane potentiates the neuromuscular blockade induced by pancuronium, vecuronium, or atracurium. The dose adjustments for these muscle relaxants when administered with sevoflurane are similar to those required with isoflurane. The effect of sevoflurane on succinylcholine and the duration of depolarizing neuromuscular blockade has not been studied.
The reduction of the dose of neuromuscular blockers during the induction of anesthesia may produce a delay in optimal conditions for endotracheal intubation or inadequate muscle relaxation, since the potentiation of neuromuscular blockers is observed a few minutes after starting the administration of sevoflurane.
Among non-depolarizing agents, interactions have been studied with vecuronium, pancuronium, and atracurium. In the absence of specific guidelines: (1) for endotracheal intubation, do not reduce the dose of non-depolarizing muscle relaxants; and (2) during maintenance of anesthesia, it is likely that the dose of non-depolarizing neuromuscular blockers will need to be reduced when compared to anesthesia with N2O/opioids. The administration of supplemental doses of muscle relaxants should be based on the response to nerve stimulation.
OVERDOSAGE
In case of apparent overdose, the following should be done: discontinue administration of SEVORANE, establish an airway, initiate assisted or controlled ventilation with oxygen, and maintain adequate cardiovascular function.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to SEVORANE 100% LIQUID FOR INHALATIONDosage form: PULMONARY INHALATION, 1 ml/mlActive substance: sevofluraneManufacturer: Baxter S.L.Prescription requiredDosage form: PULMONARY INHALATION, 100 % (V/V)Active substance: sevofluraneManufacturer: Elc Group S.R.O.Prescription requiredDosage form: PULMONARY INHALATION, 100% v/vActive substance: sevofluraneManufacturer: Piramal Critical Care B.V.Prescription required
Online doctors for SEVORANE 100% LIQUID FOR INHALATION
Discuss questions about SEVORANE 100% LIQUID FOR INHALATION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions















