SEMGLEE 100 units/mL injectable solution in prefilled pen

Ask a doctor about a prescription for SEMGLEE 100 units/mL injectable solution in prefilled pen

How to use SEMGLEE 100 units/mL injectable solution in prefilled pen
Introduction
Package Leaflet: Information for the User
Semglee 100 units/ml solution for injection in pre-filled pen
insulin glargine
This medicinal product is subject to additional monitoring, which will allow for quick identification of new safety information. You can help by reporting any side effects you may get. The last section of section 4 will tell you how to report side effects.
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Semglee and what is it used for
- What you need to know before you use Semglee
- How to use Semglee
- Possible side effects
- Storing Semglee
- Contents of the pack and other information
1. What is Semglee and what is it used for
Semglee contains insulin glargine. This is a modified insulin, very similar to human insulin.
Semglee is used to treat diabetes mellitus in adult, adolescent, and child patients from 2 years of age.
Diabetes mellitus is a disease in which your body does not produce enough insulin to control the level of sugar in the blood. Insulin glargine has a long-acting and constant effect on reducing blood sugar levels.
2. What you need to know before you use Semglee
Do not use Semglee
- if you are allergic to insulin glargine or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Semglee in pre-filled pen is only suitable for subcutaneous injections. Consult your doctor if you need to inject your insulin by another method.
Consult your doctor, pharmacist, or nurse before you start using Semglee.
Strictly follow your doctor's instructions regarding dosage, control (blood and urine tests), diet, and physical activity (work and exercise), and injection technique.
If your blood sugar level is too low (hypoglycaemia), follow the guidelines for hypoglycaemia (see the box at the end of this leaflet).
Travel
Before travelling, consult your doctor. You may need to discuss:
- the availability of your insulin in the country you are visiting,
- insulin, needles, etc. supplies,
- the correct storage of insulin during travel,
- meal and insulin administration schedules during travel,
- the possible effects of crossing time zones,
- new health risks in the countries you are visiting,
- what to do in emergency situations when you are ill or become unwell.
Illnesses and injuries
The management of your diabetes may require special care in the following situations (e.g. adjustment of insulin dose, blood and urine tests):
- If you are ill or suffer a major injury, your blood sugar level may increase (hyperglycaemia).
- If you do not eat enough, your blood sugar level may fall too low (hypoglycaemia).
In most cases, you will need a doctor. Make sure to consult a doctor immediately.
If you have type 1 diabetes (insulin-dependent diabetes mellitus), do not stop taking your insulin and continue to take enough carbohydrates. Always inform the people in charge of your care or treatment that you need insulin.
Treatment with insulin can cause your body to produce antibodies to insulin (substances that act against insulin). However, only in very rare cases will you need to change your insulin dose.
Some patients with type 2 diabetes mellitus of long duration and previous heart disease or stroke who were treated with pioglitazone (an oral antidiabetic medication used to treat type 2 diabetes mellitus) and insulin developed heart failure. Inform your doctor as soon as possible if you experience signs of heart failure such as unusual shortness of breath or rapid weight gain or localized swelling (oedema).
Children
There is no experience with the use of Semglee in children under 2 years of age.
Using Semglee with other medicines
Some medicines can change your blood sugar levels (increase, decrease, or both, depending on the situation). In each case, you may need to adjust your insulin dose to avoid too low or too high blood sugar levels. Be careful when you start taking another medicine and also when you stop taking it.
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines. Ask your doctor before taking a medicine if it can affect your blood sugar level and what measures you should take.
Among the medicines that can cause a decrease in your blood sugar level (hypoglycaemia) are:
- all other medicines for treating diabetes,
- angiotensin-converting enzyme (ACE) inhibitors (used to treat certain heart diseases or high blood pressure),
- disopyramide (used to treat certain heart diseases),
- fluoxetine (used to treat depression),
- fibrates (used to reduce high lipid levels in the blood),
- monoamine oxidase inhibitors (MAOIs) (used to treat depression),
- pentoxifylline, propoxyphene, salicylates (such as acetylsalicylic acid, used to relieve pain and reduce fever),
- sulphonamides (a group of antibiotics).
Among the medicines that can cause an increase in your blood sugar level (hyperglycaemia) are:
- corticosteroids (such as "cortisone", used to treat inflammation),
- danazol (a medicine that acts on ovulation),
- diazoxide (used to treat high blood pressure),
- diuretics (used to treat high blood pressure or excess fluid retention),
- glucagon (a pancreatic hormone used to treat severe hypoglycaemia),
- isoniazid (used to treat tuberculosis),
- oestrogens and progestogens (such as the contraceptive pill used for birth control),
- phenothiazine derivatives (used to treat psychiatric diseases),
- somatotropin (growth hormone),
- sympathomimetic medicines (such as adrenaline or salbutamol, terbutaline for treating asthma),
- thyroid hormones (used to treat underactive thyroid gland),
- atypical antipsychotic medicines (such as clozapine, olanzapine),
- protease inhibitors (used to treat HIV).
Your blood sugar level may increase or decrease if you take:
- beta-blockers (used to treat high blood pressure),
- clonidine (used to treat high blood pressure),
- lithium salts (used to treat psychiatric diseases).
Pentamidine (used to treat some parasitic infections) can cause hypoglycaemia, which may sometimes be followed by hyperglycaemia.
Beta-blockers, like other sympatholytic medicines (such as clonidine, guanethidine, and reserpine), can mask or completely suppress the first warning symptoms that could help you recognise a hypoglycaemic attack.
If you are not sure whether you are taking any of these medicines, ask your doctor or pharmacist.
Using Semglee with alcohol
Your blood sugar levels may increase or decrease if you drink alcohol.
Pregnancy and breast-feeding
Consult your doctor or pharmacist before using any medicine.
Tell your doctor if you are planning to become pregnant or if you are already pregnant. Your insulin dose may need to be changed during pregnancy and after delivery. Careful monitoring of your diabetes and prevention of hypoglycaemia are important for the health of your baby.
If you are breast-feeding, consult your doctor, as you may need to adjust your insulin dose and diet.
Driving and using machines
Your ability to concentrate or react may be reduced if:
- you have hypoglycaemia (low blood sugar levels),
- you have hyperglycaemia (high blood sugar levels),
- you have vision problems.
Be aware of this possible problem and consider all situations that could be a risk for you or others (such as driving a vehicle or using machines). You should ask your doctor for advice on driving if:
- you have frequent episodes of hypoglycaemia,
- the first warning symptoms of a hypoglycaemic attack have decreased or disappeared.
Semglee contains sodium
This medicine contains less than 1 mmol (23 mg) of sodium per dose, which is essentially "sodium-free".
3. How to use Semglee
Follow exactly the instructions for administration of this medicine given by your doctor. If you are not sure, ask your doctor or pharmacist.
Although Semglee contains the same active substance as insulin glargine 300 units/ml, these medicines are not interchangeable. Changing from one insulin treatment to another requires medical prescription, supervision, and blood glucose monitoring. For more information, consult your doctor.
Dose
Based on your lifestyle and the results of your blood glucose tests and previous insulin treatment, your doctor will:
- determine the Semglee dose you need each day and at what time,
- tell you when to test your blood sugar level and if you need to carry out urine tests,
- tell you when you may need to inject a higher or lower dose of Semglee.
Semglee is a long-acting insulin. Your doctor may tell you to use it in combination with a short-acting insulin or with tablets to treat high blood sugar levels.
Many factors can influence your blood sugar level. You should be aware of these factors so that you can react correctly to changes in your blood sugar level and prevent it from becoming too high or too low. For more information, see the box at the end of the leaflet.
Use in children and adolescents
Semglee can be used in adolescents and children from 2 years of age. Use this medicine exactly as your doctor has told you.
Administration frequency
You need one injection of Semglee every day, always at the same time.
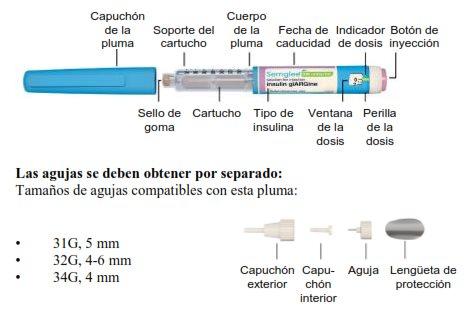
The Semglee pen delivers insulin in increments of 1 unit up to a maximum single dose of 80 units.
Method of administration
Semglee is injected under the skin. DO NOT inject Semglee into a vein, as this will change its action and may cause hypoglycaemia.
Your doctor will show you which area of the skin to inject Semglee into. With each injection, change the injection site within the area of skin you are using.
How to handle the Semglee pen
Semglee in pre-filled pen is only suitable for subcutaneous injections. Consult your doctor if you need to inject your insulin by another method.
Read carefully the "Instructions for Use" included in this leaflet. You must use the pen exactly as described in these Instructions for Use.
Before each use, insert a new needle. Only use needles compatible with the Semglee pen (see "Instructions for Use").
Before each injection, perform a safety test.
Inspect the cartridge before using the pen. Do not use Semglee if you notice particles in it. Only use Semglee if the solution is clear and colourless. Do not shake or mix before use.
To prevent the possible transmission of diseases, never share your pen with anyone else. This pen is for your use only.
Always use a new pen if you notice that your blood sugar control gets worse for no explainable reason. If you think you may have a problem with the Semglee pen, consult your doctor, pharmacist, or nurse.
Empty pens must not be refilled and must be disposed of safely.
Do not use the Semglee pen if it is damaged or not working properly (due to mechanical defects), it must be disposed of and a new Semglee pen used.
Insulin confusion
Always check the insulin label before each injection to avoid mix-ups between Semglee and other insulins.
If you use more Semglee than you should
If you have injected too much Semglee,your blood sugar level may become too low (hypoglycaemia). Check your blood sugar level frequently. In general, to prevent hypoglycaemia, you should eat more and check your blood sugar level. For more information on treating hypoglycaemia, see the box at the end of the leaflet.
If you forget to use Semglee
If you have missed a dose of Semgleeor if you have not injected enough insulin,your blood sugar level may become too high (hyperglycaemia). Check your blood sugar level frequently. For more information on treating hyperglycaemia, see the box at the end of the leaflet.
Do not take a double dose to make up for forgotten doses.
If you stop using Semglee
This could lead to severe hyperglycaemia (very high blood sugar levels) and ketoacidosis (increased acid in the blood because the body is breaking down fat instead of sugar). Do not stop your treatment with Semglee without consulting your doctor, who will tell you what to do.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist, or nurse.
4. Possible Adverse Effects
Like all medicines, Semglee can cause adverse effects, although not all people will experience them.
If you notice signs that your blood sugar level is too low (hypoglycemia),act immediately to raise your blood sugar level (see the box at the end of this leaflet). Hypoglycemia (low blood sugar) can be very serious and is very common during insulin treatment (it can affect more than 1 in 10 people). Low blood sugar means that there is not enough sugar in the blood. If your blood sugar level drops too low, you can lose consciousness (pass out). Severe hypoglycemia can cause brain damage and can be potentially fatal. For more information, see the box at the end of this leaflet.
Severe allergic reactions(rare, may affect up to 1 in 1,000 people): signs may include widespread skin reactions (skin rash and itching all over the body), severe swelling of the skin or mucous membranes (angioedema), difficulty breathing, low blood pressure with rapid heartbeat and sweating. Severe allergic reactions to insulins can be potentially fatal. Inform your doctor immediately if you notice signs of severe allergic reactions.
Skin changes at the injection site:
If you inject insulin too frequently in the same spot, the skin can shrink (lipoatrophy, may affect up to 1 in 100 people) or thicken (lipohypertrophy, may affect up to 1 in 10 people). Lumps under the skin caused by the accumulation of a protein called amyloid (cutaneous amyloidosis, frequency unknown) may also appear. Insulin may not work as well. Change the injection site with each injection to help prevent these skin changes.
Common Adverse Effects(may affect up to 1 in 10 people)
- Skin effects and allergic reactions at the injection site
Signs may include redness, intense pain when injecting, itching, hives, swelling, or inflammation. These reactions can spread around the injection site. Most mild reactions to insulin usually disappear within a few days or weeks.
- Skin effects and allergic reactions at the injection site
Signs may include redness, intense pain when injecting, itching, hives, swelling, or inflammation. These reactions can spread around the injection site. Most mild reactions to insulin usually disappear within a few days or weeks.
Rare Adverse Effects(may affect up to 1 in 1,000 people)
- Ocular reactions
A significant change (improvement or worsening) in blood sugar control can temporarily alter your vision. If you have proliferative retinopathy (a vision disorder related to diabetes), severe hypoglycemic attacks can cause temporary vision loss.
- General disorders
In rare cases, insulin treatment can also cause temporary water retention in the body, with swelling of the ankles and feet.
Very Rare Adverse Effects(may affect up to 1 in 10,000 people)
In very rare cases, dysgeusia (taste disorders) and myalgia (muscle pain) can occur.
Use in Children and Adolescents
In general, adverse effects in children and adolescents 18 years or younger are similar to those in adults.
Reports of injection site reactions (injection site reaction, pain at the injection site) and skin reactions (rash, hives) have been more frequently reported in children or adolescents 18 years or younger than in adults.
There is no experience in children under 2 years of age.
Reporting Adverse Effects
If you experience adverse effects, consult your doctor or pharmacist. This includes possible adverse effects not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting adverse effects, you can help provide more information on the safety of this medicine.
5. Storage of Semglee
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date stated on the carton and label of the pen after CAD/EXP. The expiry date is the last day of the month indicated.
Unused pens
Store in a refrigerator (between 2°C and 8°C). Do not freeze or place near the freezer compartment or a cold accumulator.
Keep the pre-filled pen in the outer packaging to protect it from light.
Pens in use
The pre-filled pen in use or to be carried as a spare should be stored for a maximum of 4 weeks below 30°C and protected from direct heat or direct light. Do not use after this time period. The pen in use should not be stored in a refrigerator.
The pen cap should be replaced after each injection to protect it from light.
Remove the needle after injection and store the pen without the needle. Also, make sure to remove the needle before disposing of the pen. Needles should not be reused.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of the packaging and medicines that are no longer needed. This will help protect the environment.
6. Container Contents and Additional Information
Semglee Composition
- The active substance is insulin glargine. Each ml of solution contains 100 units of insulin glargine (equivalent to 3.64 mg).
- The other components are: zinc chloride, metacresol, glycerol, sodium hydroxide (for pH adjustment) (see section 2 "Semglee contains sodium"), hydrochloric acid (for pH adjustment), and water for injectable preparations.
Product Appearance and Container Contents
Semglee 100 units/ml solution for injection in a pre-filled pen is a clear, colorless solution.
Each pen contains 3 ml of injection solution (equivalent to 300 units).
Semglee is available in packs of 1, 3, 5, and 10 pens or a multipack containing 2 packs, each with 5 pens.
Only some pack sizes may be marketed.
Marketing Authorization Holder
Biosimilar Collaborations Ireland Limited
Unit 35/36
Grange Parade,
Baldoyle Industrial Estate,
Dublin 13
DUBLIN
Ireland
D13 R20R
Manufacturer
Biosimilar Collaborations Ireland Limited
Block B, The Crescent Building, Santry Demesne
Dublin
D09 C6X8
Ireland
You can request more information about this medicinal product from the local representative of the marketing authorization holder:
Belgium Biocon Biologics Belgium BV Tel: 0080008250910 | Lithuania Biosimilar Collaborations Ireland Limited Tel: 0080008250910 |
Bulgaria Biosimilar Collaborations Ireland Limited Tel: 0080008250910 | Luxembourg Biocon Biologics France S.A.S Tel: 0080008250910 |
Czech Republic Biocon Biologics Germany GmbH Tel: 0080008250910 | Hungary Biosimilar Collaborations Ireland Limited Tel: 0080008250910 |
Denmark Biocon Biologics Finland OY Tel: 0080008250910 | Malta Biosimilar Collaborations Ireland Limited Tel: 0080008250910 |
Germany Biocon Biologics Germany GmbH Tel: 0080008250910 | Netherlands Biocon Biologics France S.A.S Tel: 0080008250910 |
Estonia Biosimilar Collaborations Ireland Limited Tel: 0080008250910 | Norway Biocon Biologics Finland OY Tel: +47 800 62 671 |
Greece Biocon Biologics Greece ΜΟΝΟΠΡΟΣΩΠΗ Ι.Κ.Ε Tel: 0080008250910 | Austria Biocon Biologics Germany GmbH Tel: 0080008250910 |
Spain Biocon Biologics Spain S.L. Tel: 0080008250910 | Poland Biosimilar Collaborations Ireland Limited Tel: 0080008250910 |
France Biocon Biologics France S.A.S Tel: 0080008250910 | Portugal Biocon Biologics Spain S.L. Tel: 0080008250910 |
Croatia Biocon Biologics Germany GmbH Tel: 0080008250910 | Romania Biosimilar Collaborations Ireland Limited Tel: 0080008250910 |
Ireland Biosimilar Collaborations Ireland Limited Tel: 1800 777 794 | Slovenia Biosimilar Collaborations Ireland Limited Tel: 0080008250910 |
Iceland Biocon Biologics Finland OY Tel: +345 8004316 | Slovakia Biocon Biologics Germany GmbH Tel: 0080008250910 |
Italy Biocon Biologics Spain S.L. Tel: 0080008250910 | Finland Biocon Biologics Finland OY Tel: 99980008250910 |
Cyprus Biosimilar Collaborations Ireland Limited Tel: 0080008250910 | Sweden Biocon Biologics Finland OY Tel: 0080008250910 |
Latvia Biosimilar Collaborations Ireland Limited Tel: 0080008250910 |
Date of Last Revision of this Leaflet: {month YYYY}.
Other Sources of Information
Detailed information on this medicinal product is available on the European Medicines Agency website: http://www.ema.europa.eu.
Semglee 100 units/ml solution for injection in a pre-filled pen. INSTRUCTIONS FOR USE
Read these Instructions for Use and the leaflet carefully before using the pre-filled pen Semglee and each time you use another pen. It may contain new information. This information does not replace consultation with your doctor, nurse, or pharmacist about your medical condition or treatment. If you cannot read or follow all the instructions on your own, ask for help from someone who is trained to use this pen. It is not recommended that blind or visually impaired people use this pen without the help of someone trained to use it.
If you do not follow these instructions each time you use the pen, you may inject too much insulin or too little. This can affect your blood sugar level.
Semglee is a disposable pre-filled pen injector that contains 300 units of insulin glargine in 3 ml of solution (100 units/ml). You can inject from 1 to 80 units in a single injection.
Do not share the pre-filled pen Semglee with another person, even if you have changed the needle. You may give other people a serious infection or get infected from them.
Assembly of the Pen:
Supplies Required:
Make sure you have the following items before injecting your dose:
- Semglee pen
- Disposable sterile hypodermic needle compatible with this pen
- 2 alcohol swabs
- Container for disposal of sharp objects
Storage
Before using the pen for the first time, store the packs that contain the pen in the refrigerator
(2 °C–8 °C).
Do notfreeze the pen.
After removing a pen from the refrigerator, place it on a flat surface and wait for it to reach room temperature, between 15 °C and 30 °C, before using it.
After the first use of the pen, store it at room temperature up to a maximum of
30 °C. Do not put the pen back in the refrigerator after use.
Always store the pen with the cap on to avoid contamination.
You must discard the pen you are using after 4 weeks of the first use, even if there is still insulin left. See Step 8 for disposal instructions.
Do notleave the needle attached to the pen during storage or reuse needles. Keep the pen and needles out of the sight and reach of children.
Always use a new sterile needle for each injection, as this prevents blocked needles and avoids infections.
Each Time You Use the Pen
- Wash your hands with water and soap before using the pen.
- Check the pen label to make sure you are injecting the correct type of insulin. The pen has a purple and white label and a purple injection button.
- Check the expiration date on the pen label. Do not use it after this date.
- Make sure the medicine in the pen cartridge looks clear and colorless. Do not use the pen if the medicine in the cartridge is cloudy, colored, or if you can see particles.
- Always use a new disposable sterile needle for each injection.
- Use an injection site that your healthcare professional has told you to use.
Step 1. Preparation of the Pen
A – Inspect the pen: check the purple and white label on the pen to make sure:
- It is the correct type of insulin.
- The expiration date has not passed.
B – Hold the pen body with one hand. Remove the pen cap with the other hand. Set the cap aside for later use.

C – Check the insulin through the cartridge holder to make sure:
- The appearance of the insulin is clear and colorless.
- There are no cracks, breaks, or leaks around the cartridge holder.
D – Clean the rubber seal (on the front of the cartridge) with a new alcohol swab.

Step 2. Attaching a New Needle
A – Take a new disposable sterile needle and remove the protective seal. Do notuse the needle if the protective seal is damaged or missing, as the needle may be contaminated.

B – While holding the needle body facing up, place the outer needle cap directly over the cartridge holder, as shown. If you try to place the outer needle cap sideways, the needle may bend or become damaged.

C – Turn the outer needle cap clockwise (to the right) until you feel it click firmly into place on the pen.

D – Carefully remove the outer needle cap and set it aside. Do not throw it away, as you will need it later.
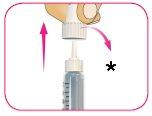
*Keep the outer needle cap
E – Carefully remove the inner needle cap and discard it.

- Discard the inner needle cap
Step 3. Preparation of the Pen Needle
A – Always prepare a new pen needle before each injection.
B – Turn the white dose dial to 2 units of dose. You will hear a "click" for each unit you turn.
If you turn past 2 units by mistake, turn the dose dial back the other way to correct the number of units.
B – Hold the pen body facing up with one hand.
D – Gently tap the cartridge with your finger to help large air bubbles move to the top of the cartridge. You may still see small bubbles. This is normal.

- TAP
E – With the pen straight, press the injection button until it stops moving and the dose window shows "0".
F – Repeat steps 3B to 3E up to three more times until you see drops of insulin at the needle tip.
Preparation is complete when you can see the drops of insulin.

If you do not see insulin at the needle tip after 4 attempts at preparation, the needle may be blocked. If this happens:
- Go to Step 7 for instructions on how to safely remove the needle.
- Start the process again at Step 2A to attach and prepare a new needle.
Step 4. Dose Selection
A – Check that the dose window shows "0".
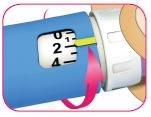
B – Turn the white dose dial until the yellow dose indicator is aligned with the desired dose.
As you turn the white dose dial to adjust your dose, it will extend and you will hear a "click" at each marked unit.
The dose can be corrected; to do this, you must turn the dose dial in either direction until the correct dose is aligned with the yellow dose indicator.

Example of 48 units selected
The pen will not allow you to dial a dose that exceeds the number of units left in the pen. If your dose exceeds the number of units left in the pen:
- Inject the amount left in the pen and use a new pen to administer the rest of the dose
or
- Take a new pen and inject the full dose.
Do notforce the dose dial beyond 80 units.
Do notpress the purple injection button while turning the dose dial.
Step 5. Selection and Cleaning of the Injection Site
A – Choose the injection site as your healthcare professional has told you, clean the area with a new alcohol swab, and let the skin dry before injecting the dose.
Injection sites include the arms, thighs, buttocks, and abdomen. You must change the injection sites for each injection.

Step 6. Injection of the Dose
A – If your healthcare professional has told you to do so, you can pinch the clean skin between your fingers.

B – Insert the needle into the skin straight, as your healthcare professional has told you.
Do notinject at an angle.
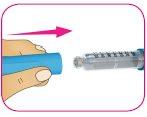
C – Press the purple injection button all the way down. The white dose dial will turn and you will hear "clicks" as you press.

- Press to administer
D – Keep the purple injection button pressed down for 10 seconds after the dose window shows "0" to make sure you inject all the insulin. If you do not keep the injection button pressed down for 10 seconds after the dose window shows "0", you may receive the wrong dose of the medicine.

- Hold down for 10 seconds
Do notpress the injection button sideways or block the white dose dial with your fingers, as this will prevent you from injecting the medicine.
Step 7. After the Injection
A – Take the outer needle cap that you set aside in Step 2D, hold it by the wide part, and carefully cover the needle without touching it.

B – Squeeze the wide part of the outer needle cap and unscrew the needle counterclockwise (to the left). Keep turning the needle until it comes off the pen. You may need to turn it several times to release the needle.

C – Place the needle in the container for disposal of sharp objects (see Step 8 for disposal instructions).

D – Put the pen cap back on the pen.
E – Store the pen at room temperature (below 30 °C). Do notstore the pen with a used needle attached.
Step 8. Disposal
Put the used needle in a container for disposal of sharp objects immediately after use. Do notthrow away (dispose of) loose needles in a household waste container.
If you do not have a container for sharp objects, you can use a household container that:
- is made of heavy-duty plastic,
- can be closed with a tight-fitting, puncture-resistant lid, that will not allow the sharp objects to come out of the container,
- is upright and stable during use,
- is leak-proof and
- is properly labeled to warn of hazardous waste inside the container.
The used pen can be thrown away in the household waste container once you have removed the needle.
Care of the Pen
- Always carry a spare pre-filled pen of insulin, as recommended by your healthcare professional, in case your pen is lost or damaged.
- Always use a new disposable needle for each injection.
- Read and follow the instructions carefully before using your pen, and make sure you understand how to use it correctly. Use a new, sterile needle for each injection.
- Keep the pen away from moisture, dust, direct sunlight, and places where the temperature may rise or fall too much (see the storage section at the beginning of these instructions).
- You can clean the outside of your pen with a damp cloth.
- Avoid dropping the pen, as this may cause the cartridge to break or damage the pen.
- Do notshare your pen with others, even if you have changed the needle. You may transmit a serious infection to others or get infected from them.
- Do notsoak or wash the pen. Do notuse alcohol, hydrogen peroxide, bleach, or any other liquid to clean the pen. Do notapply lubricants, such as oil. This could damage the pen.
- Do notattempt to repair a damaged or non-functional pen. Remove the needle as described in step 7 and discard the pen or return it to your pharmacist. Use a new pen instead.

How much does SEMGLEE 100 units/mL injectable solution in prefilled pen cost in Spain ( 2026)?
The average price of SEMGLEE 100 units/mL injectable solution in prefilled pen in January, 2026 is around 56.25 EUR. Prices may vary depending on the region, pharmacy, and whether a prescription is required. Always check with a local pharmacy or online source for the most accurate information.
- Country of registration
- Average pharmacy price56.25 EUR
- Availability in pharmaciesSupply issue reported
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to SEMGLEE 100 units/mL injectable solution in prefilled penDosage form: INJECTABLE, 100 U/mlActive substance: insulin glargineManufacturer: Eli Lilly Nederland B.V.Prescription requiredDosage form: INJECTABLE, UnknownActive substance: insulin glargineManufacturer: Sanofi-Aventis Deutschland GmbhPrescription requiredDosage form: INJECTABLE, UnknownActive substance: insulin glargineManufacturer: Sanofi-Aventis Deutschland GmbhPrescription required
Alternatives to SEMGLEE 100 units/mL injectable solution in prefilled pen in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to SEMGLEE 100 units/mL injectable solution in prefilled pen in Ukraine
Online doctors for SEMGLEE 100 units/mL injectable solution in prefilled pen
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for SEMGLEE 100 units/mL injectable solution in prefilled pen – subject to medical assessment and local rules.