
PROPOFOL FARMAK 20 mg/ml Injectable Emulsion for Infusion

How to use PROPOFOL FARMAK 20 mg/ml Injectable Emulsion for Infusion
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Propofol Farmak 20mg/ml injectable emulsion and for infusion EFG
Read all of this leaflet carefully before you are given this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- If you experience any side effects, talk to your doctor, pharmacist or nurse, even if it is not listed in this leaflet. See section 4.
Contents of the pack
- What Propofol Farmak is and what it is used for
- What you need to know before you are given Propofol Farmak
- How to use Propofol Farmak
- Possible side effects
- Storage of Propofol Farmak
- Contents of the pack and other information
1. What Propofol Farmak is and what it is used for
Propofol Farmak contains the active substance propofol. It belongs to a group of medicines called “general anaesthetics”. General anaesthetics are used to produce unconsciousness (sleep) to enable surgical operations or other procedures to be performed. They can also be used to sedate you (to make you sleepy but not completely asleep).
Propofol Farmak will be given to you by injection or infusion by a doctor.
Propofol Farmak 20 mg/ml is used for:
- induction and maintenance of general anaesthesia in adults, adolescents and children over 3 years.
- sedation of patients over 16 years old who are receiving artificial respiration in intensive care.
- sedation of adults, adolescents and children over 3 months during diagnostic and surgical procedures, alone or in combination with local or regional anaesthesia.
2. What you need to know before you are given Propofol Farmak
Propofol Farmak must not be used:
- If you are allergic to propofol, peanut or soya or any of the other ingredients of this medicine (listed in section 6).
- If you are 16 years old or younger for sedation in intensive care.
Warnings and precautions
Tell your doctor or anaesthetist before you are given propofol and if any of the following apply to you or have applied in the past.
Propofol should be given with extreme caution and under close supervision, if you:
- have advanced heart failure.
- have any other severe heart disease.
- are receiving electroconvulsive therapy (ECT, a treatment for psychiatric problems).
Generally, propofol should be given with caution to elderly or weak patients.
Before you are given propofol, tell your anaesthetist or intensive care doctor if you have:
- heart disease.
- lung disease.
- kidney disease.
- liver disease.
- seizures (epilepsy).
- high pressure inside the skull (raised intracranial pressure). In combination with low blood pressure, this can reduce the amount of blood that reaches the brain.
- altered fat levels in the blood. If you are receiving total parenteral nutrition (nutrition through a vein), your blood fat levels should be monitored.
- if your body has lost a lot of water (you are hypovolaemic).
If you have any of the following conditions, you should be treated before you are given propofol:
- heart failure.
- when not enough blood is reaching the tissues (circulatory failure).
- severe breathing problems (respiratory failure).
- dehydration (hypovolaemia).
- seizures (epilepsy).
Propofol may increase the risk of
- seizure.
- a nervous reflex that slows down the heart rate (vagotonia, bradycardia).
- changes in blood flow to the body's organs (haemodynamic effects on the cardiovascular system) if you are overweight and receive high doses of propofol.
Involuntary movements can occur during sedation with propofol. Doctors will take into account how this may affect surgical procedures performed under sedation and will take necessary precautions.
Very rarely, after anaesthesia, there may be a period of unconsciousness associated with muscle stiffness. This requires observation by healthcare professionals, but no other treatment is needed. It will resolve on its own.
The injection of Propofol Farmak can be painful. Local anaesthesia can be used to reduce the pain, but it can have its own side effects.
You will not be able to leave the hospital until you are fully awake.
If you are able to go home soon after receiving propofol, you should not do so without an escort.
Children and adolescents
The use of Propofol Farmak 20 mg/ml injectable emulsion and for infusion EFG is not indicated in children under 3 years of age.
Propofol must not be given to children and adolescents under 16 years old for sedation in the intensive care unit, as its safety has not been established in this patient group for this indication.
Other medicines and Propofol Farmak
Tell your doctor if you are taking, have recently taken or might take any other medicines. This includes medicines that you buy without a prescription and herbal medicines.
In particular, tell your doctor, anaesthetist or nurse if you are taking any of the following medicines:
- rifampicin (for tuberculosis, TB)
- midazolam (used to induce sedation and relieve anxiety and muscle tension).
You should be careful if you are also taking or receiving any of the following medicines:
- pre-anaesthetic medication (your anaesthetist will know which medicines may be affected by propofol)
- other anaesthetics, including general, regional, local and inhalational anaesthetics (lower doses of propofol may be needed. Your anaesthetist will know)
- sedatives (analgesics)
- strong sedatives (fentanyl or opioids)
- parasympatholytic medicines (medicines used to treat, for example, painful spasms of organs, asthma or Parkinson's disease)
- benzodiazepines (medicines used to treat anxiety)
- suxamethonium (muscle relaxant)
- medicines that affect many of the body's internal functions, such as heart rate, for example, atropine
- medicines or drinks that contain alcohol
- neostigmine (medicine used to treat a disease called myasthenia gravis)
- ciclosporin (medicine used to prevent transplant rejection)
- valproate (medicine used to treat epilepsy or mental disorders)
Propofol Farmak with food, drinks and alcohol
After you have been given this medicine, you should not eat, drink or consume alcohol until you are fully recovered.
Pregnancy, breast-feeding and fertility
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor for advice before taking this medicine.
The safety of propofol during pregnancy has not been established. Animal studies have shown reproductive toxicity.
Propofol should not be used during pregnancy unless absolutely necessary. However, propofol may be used during an induced abortion.
Propofol crosses the placenta and may cause neonatal depression (neonatal depression syndrome due to drugs). You should stop breast-feeding and discard any expressed breast milk for 24 hours after receiving propofol.
Driving and using machines
After receiving propofol, you may still feel sleepy for some time.
Do not drive or use tools or machines until you are sure that the effects have worn off.
If you are able to go home soon after receiving propofol, do not drive or go home without an escort, or use tools or machines.
Ask your doctor when you can resume these activities and return to work.
Propofol Farmak contains soya oil and sodium
Propofol Farmak contains soya oil. If you are allergic to peanut or soya, do not use this medicine.
This medicine contains less than 1 mmol of sodium (23 mg) per 100 ml, i.e. it is essentially “sodium-free”.
3. How to use Propofol Farmak
Propofol will only be given to you in hospitals or suitable therapeutic units by or under the direct supervision of your anaesthetist or intensive care doctor.
Dose
The dose of propofol varies from one patient to another. The amount of propofol you need depends on your age, size and physical condition. Your doctor will give you the correct dose to induce and maintain anaesthesia or to achieve the necessary level of sedation, carefully observing your responses and vital signs (pulse, blood pressure, breathing, etc.).
You may need several different medicines to keep you asleep or sedated, pain-free, breathing healthily and to keep your blood pressure stable. Your doctor will decide which medicines you need and when you need them.
Use in children and adolescents
Propofol Farmak 20 mg/ml injectable emulsion and for infusion EFG for use in children and adolescents over 3 years of age
The use of Propofol Farmak 20 mg/ml injectable emulsion and for infusion EFG is not recommended in children under 3 years of age.
Propofol must not be given to children and adolescents under 16 years old for sedation in the intensive care unit, as its safety has not been established in this patient group for this indication.
Method of administration
Propofol Farmak is for intravenous use. Your anaesthetist may use a needle or a cannula. Propofol Farmak will be injected into a vein either manually or using electric pumps.
Before use, the rubber membrane should be cleaned with an alcohol spray or an alcohol-impregnated swab.
Duration of treatment
When used for sedation, propofol should not be given for more than 7 days.
If you have been given more propofol than you should
Circulatory and respiratory depression may occur. In the event of respiratory arrest, artificial respiration is required; in the event of a drop in blood pressure, the usual measures are required, such as placing the patient's head in a low position, possibly plasma substitutes (blood volume expanders) and, if necessary, vasoconstrictor agents.
Your doctor will make sure that you receive the correct amount of propofol for you and for the procedure you are undergoing.
However, each person needs a different dose, and if you receive a dose that is too high for you, your anaesthetist may need to take measures to ensure that your heart and breathing receive the necessary support.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Side effects that may occur during anaesthesia
The following side effects may occur during anaesthesia (while you are being given the injection or when you are sleepy or asleep). Your doctor will be monitoring you for these. If they occur, your doctor will give you the necessary treatment.
Very common (may affect more than 1 in 10 people)
- Pain at the injection site (while the injection is being given, before you fall asleep).
Common (may affect up to 1 in 10 people)
- Slow or fast heart beats.
- Low blood pressure.
- Changes in breathing pattern (low breathing rate, respiratory arrest).
- Hiccup.
- Cough (may also occur when waking up).
Uncommon (may affect up to 1 in 100 people)
- Swelling and redness or blood clots in the vein along the injection site.
Rare (may affect up to 1 in 1,000 people)
- Body twitching or convulsions (may also occur when waking up).
Very rare (may affect up to 1 in 10,000 people)
- Severe allergic reaction causing difficulty breathing, swollen and red skin, flushing. Fluid accumulation in the lungs that can make you very short of breath (may also occur when waking up).
- Unusual urine colour (may also occur when waking up).
Frequency not known (cannot be estimated from the available data)
- Involuntary movements.
- Severe skin and tissue reaction after accidental application outside the vein.
- Prolonged, often painful erection (priapism).
Side effects that may occur after anaesthesia
The following side effects may occur after anaesthesia (when you are waking up or after you have woken up).
Common (may affect up to 1 in 10 people)
- Headache.
- Feeling sick (nausea), being sick (vomiting).
- Cough.
Rare (may affect up to 1 in 1,000 people)
- Dizziness, shivering and feeling cold.
- Excitement.
Very rare (may affect up to 1 in 10,000 people)
- Being unconscious after the operation (when this has happened, patients have recovered without problems).
- Pancreatitis (inflammation of the pancreas) causing severe stomach pain (a causal relationship has not been established).
- Post-operative fever.
Frequency not known (cannot be estimated from the available data)
- Feeling of euphoria.
- Feeling of sexual excitement.
- Irregular heart beats.
- Changes in ECG (ECG type Brugada).
- Increased liver size.
- Kidney failure.
- Breakdown of muscle cells (rhabdomyolysis), increased blood acidity, high levels of potassium and fat in the blood, heart failure.
- Drug abuse, especially by healthcare professionals.
- Prolonged, often painful erection (priapism).
- Hepatitis (inflammation of the liver), acute liver failure (symptoms may include yellowing of the skin and eyes, itching, dark urine, stomach pain and sensitivity of the liver (indicated by pain under the front of the ribcage on the right side), sometimes with loss of appetite).
When Propofol Farmak is given in combination with lidocaine (a local anaesthetic used to reduce pain at the injection site), the following side effects may rarely occur:
- dizziness
- vomiting
- drowsiness
- seizures
- slow heart rate (bradycardia)
- irregular heart rhythm (cardiac arrhythmias)
- shock
Reporting of side effects
If you experience any side effects, talk to your doctor, pharmacist or nurse, even if it is not listed in this leaflet.
You can also report side effects directly to the Spanish Medicines Agency's Pharmacovigilance System for Human Use: https://www.notificaram.es. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Propofol Farmak
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the ampoule/vial and on the outer packaging after EXP. The expiry date is the last day of the month stated.
Do not store above 25°C. Do not freeze.
Once opened, the medicine should be used immediately.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Container Content and Additional Information
Composition of:
Propofol Farmak 20 mg/ml injectable and perfusion emulsion EFG
- The active ingredient is propofol.
1 ml of emulsion contains 20 mg of propofol.
1 vial of 20 ml contains 400 mg of propofol.
- 1 vial of 50 ml contains 1,000 mg of propofol.
1 vial of 100 ml contains 2,000 mg of propofol.
- The other components are soybean oil, egg phospholipids, glycerol, sodium hydroxide, disodium edetate, and water for injectable preparations.
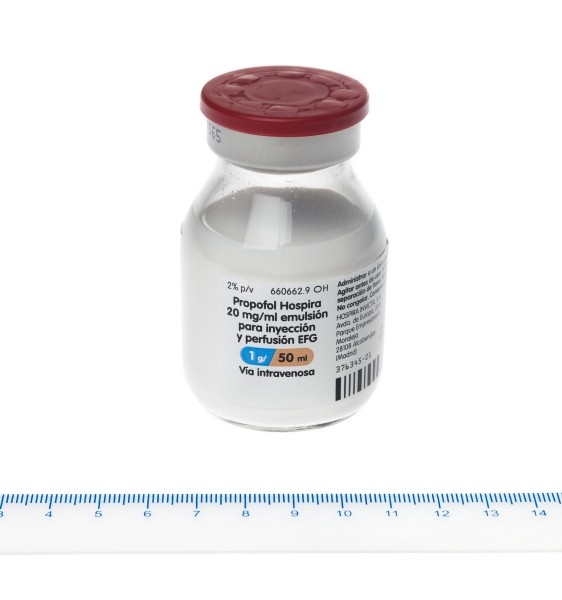
Appearance of Propofol Farmak and Container Content
Injectable and perfusion emulsion.
Propofol Farmak is a white or almost white, homogeneous emulsion.
Propofol Farmak 20 mg/ml is available in
- colorless glass vials of 20 ml with a bromobutyl rubber stopper and an aluminum cap. 5 vials in a cardboard package.
- glass vials of 50 ml and 100 ml with a bromobutyl rubber stopper and an aluminum cap. 1 vial in a cardboard package.
Only some package sizes may be marketed.
Marketing Authorization Holder and Manufacturer
Marketing Authorization Holder
Farmak International Sp. z o.o.
ul. Koszykowa, 65
00-667 Warsaw
Poland
Manufacturer
Farmak International Sp. z o.o.
Pilsudskiego 141, lodzkie
92-318, Lódz
Poland
This medicinal product is authorized in the Member States of the European Economic Area under the following names:
Germany: Propofol Farmak 20 mg/ml Emulsion zur Injektion / Infusion
Poland: Propofol Farmak, 20 mg/mL, emulsja do wstrzykiwan / infuzji
Spain: Propofol Farmak 20 mg/ml injectable and perfusion emulsion EFG
Date of the Last Revision of this Leaflet:
Other Sources of Information
Detailed information on this medicinal product is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS): http://www.aemps.gob.es/
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to PROPOFOL FARMAK 20 mg/ml Injectable Emulsion for InfusionDosage form: INJECTABLE, 1% propofolActive substance: propofolManufacturer: Aspen Pharma Trading LimitedPrescription requiredDosage form: INJECTABLE, 20 mg propofol/ mlActive substance: propofolManufacturer: Aspen Pharma Trading LimitedPrescription requiredDosage form: INJECTABLE, 10 mg/mlActive substance: propofolManufacturer: Baxter Holding B.V.Prescription required
Online doctors for PROPOFOL FARMAK 20 mg/ml Injectable Emulsion for Infusion
Discuss questions about PROPOFOL FARMAK 20 mg/ml Injectable Emulsion for Infusion, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions















