
OCTREOTIDE TEVA 10 mg POWDER AND SOLVENT FOR PROLONGED-RELEASE INJECTABLE SUSPENSION

How to use OCTREOTIDE TEVA 10 mg POWDER AND SOLVENT FOR PROLONGED-RELEASE INJECTABLE SUSPENSION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
OctreotideTeva10 mg powder and solvent for prolonged-release suspension for injection EFG
OctreotideTeva20 mg powder and solvent for prolonged-release suspension for injection EFG
OctreotideTeva30 mg powder and solvent for prolonged-release suspension for injection EFG
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Octreotide Teva and what is it used for
- What you need to know before you use Octreotide Teva
- How to use Octreotide Teva
- Possible side effects
- Storage of Octreotide Teva
- Contents of the pack and other information
1. What is Octreotide Teva and what is it used for
Octreotide is a synthetic compound derived from somatostatin. Somatostatin is normally found in the human body, where it inhibits the release of certain hormones such as growth hormone. The advantages of octreotide over somatostatin are that it is more potent and its effects are longer-lasting.
What it is used for
- to treat acromegaly,
Acromegaly is a disease in which the body produces too much growth hormone. Normally, growth hormone controls the growth of tissues, organs, and bones. An excess of growth hormone means an increase in the size of bones and tissues, especially in the hands and feet. Octreotide significantly reduces the symptoms of acromegaly, which include headache, excessive sweating, numbness of the hands and feet, fatigue, and joint pain. In most cases, the overproduction of growth hormone is caused by an increase in the size of the pituitary gland (pituitary adenoma); treatment with this medicine can reduce the size of the adenoma.
This medicine is used to treat people who suffer from acromegaly:
- when other types of treatment for acromegaly (surgery or radiotherapy) are not suitable or have not worked properly;
- after radiotherapy, to cover the intermediate period until the radiotherapy is fully effective.
- to relieve symptoms associated with the overproduction of certain specific hormones and other related substances in the stomach, intestine, or pancreas.
The overproduction of certain specific hormones and other natural substances can be caused by rare disorders of the stomach, intestine, or pancreas. This disrupts the natural hormonal balance and causes a series of symptoms such as hot flashes, diarrhea, low blood pressure, skin rash, and weight loss. Treatment with this medicine helps control these symptoms.
- to treat neuroendocrine tumors located in the intestine (e.g., appendix, small intestine, or colon),
Neuroendocrine tumors are rare tumors that can be found in different parts of the body. Octreotide is also used to control the growth of these tumors when they are located in the intestine (e.g., appendix, small intestine, or colon)
- to treat pituitary tumors that produce too much thyroid-stimulating hormone (TSH).
An excess of thyroid-stimulating hormone (TSH) causes hyperthyroidism. Octreotide is used to treat people with pituitary tumors that produce too much thyroid-stimulating hormone (TSH):
- when other types of treatment (surgery or radiotherapy) are not suitable or have not worked;
- after radiotherapy, to cover the period until the radiotherapy is fully effective.
2. What you need to know before you use Octreotide Teva
Follow all instructions given by your doctor carefully. They may be different from the information contained in this leaflet.
Read the following instructions before using this medicine.
Do not useOctreotideTeva
- if you are allergic to octreotide or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Consult your doctor before starting treatment with Octreotide Teva:
- if you know you currently have gallstones or have had them in the past, or if you have any complications such as fever, chills, abdominal pain, or yellowing of the skin or eyes; inform your doctor, as prolonged use of this medicine may cause gallstones to form. Your doctor may want to check your gallbladder periodically.
- if you know you have diabetes, as this medicine may affect blood sugar levels. If you are diabetic, you should regularly check your blood sugar levels.
- if you have a history of vitamin B12 deficiency, your doctor may periodically check your B12 level.
Tests and checks
If you are treated with this medicine for a long period, your doctor may periodically check your thyroid function.
Your doctor will check your liver function.
Your doctor may check the functioning of your pancreatic enzymes.
Children
There is limited experience with the use of this medicine in children.
Using Octreotide Teva with other medicines
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
You can usually continue taking other medicines while being treated with this medicine. However, it has been reported that some medicines such as cimetidine, cyclosporine, bromocriptine, quinidine, and terfenadine are affected by this medicine.
If you are taking a medicine to control blood pressure (e.g., a beta-blocker or a calcium channel blocker) or an agent to control fluid and electrolyte balance, your doctor may need to adjust the dose.
If you are diabetic, your doctor may need to adjust your insulin dose.
If you are going to receive treatment with lutetium (177Lu) oxodotreotide, a radiopharmaceutical, your doctor may interrupt and/or adjust treatment with Sandostatin LAR for a short period.
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor for advice before using this medicine.
Octreotide should only be used during pregnancy if it is strictly necessary.
Women of childbearing age must use an effective contraceptive method during treatment.
You should not breastfeed during treatment with this medicine. It is not known whether octreotide passes into breast milk.
Driving and using machines
Octreotide Teva has no or negligible influence on the ability to drive and use machines. However, some of the side effects you may experience during treatment with this medicine, such as headache and fatigue, may reduce your ability to drive and use machines safely.
OctreotideTevacontains sodium
Octreotide Teva contains less than 23 mg of sodium (1 mmol) per dose; this is essentially “sodium-free”.
3. How to use Octreotide Teva
This medicine must always be administered as an injection into the muscle of the buttocks. With repeated administration, the right and left buttocks should be used alternately.
If you use moreOctreotideTevathan you should
No life-threatening adverse reactions have been reported after an overdose with Octreotide Teva.
The symptoms of overdose are: hot flashes, frequent urination, fatigue, depression, anxiety, and lack of concentration.
If you think you have suffered an overdose and experience any of these symptoms, inform your doctor immediately. You can also call the Toxicology Information Service, Tel. 91 562 0420.
If you forget to useOctreotideTeva
If you have forgotten your injection, it is recommended that you receive it as soon as you remember, and then continue with your usual schedule. It will not harm you to receive a dose a few days late, but your symptoms may temporarily recur until you return to your usual treatment schedule.
If you stop treatment withOctreotideTeva
If you stop treatment with this medicine, your symptoms may recur. Therefore, do not stop treatment with octreotide unless your doctor tells you to.
If you have any further questions on the use of this medicine, ask your doctor, nurse, or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Some side effects can be serious. If you get any of the following side effects, see a doctor immediately:
Very common(may affect more than 1 in 10 people):
- Gallstones, which can cause sudden back pain.
- Too much sugar in the blood.
Common(may affect up to 1 in 10 people)
- Decreased activity of the thyroid gland (hypothyroidism) that causes changes in heart rate, appetite, or weight; fatigue, feeling cold, or swelling in the front of the neck.
- Changes in thyroid function tests.
- Inflammation of the gallbladder (cholecystitis); symptoms may include pain in the upper right abdomen, fever, nausea, yellowing of the skin and eyes (jaundice).
- Too little sugar in the blood.
- Alteration of glucose tolerance.
- Slow heart rate.
Uncommon(may affect up to 1 in 100 people)
- Thirst, low urine output, dark urine, dry reddened skin.
- Fast heart rate.
Other serious side effects
- Hypersensitivity reactions (allergic reactions) including skin rash.
- A type of allergic reaction (anaphylaxis) that can cause difficulty swallowing or breathing, swelling, and tingling, possibly with a decrease in blood pressure with dizziness or loss of consciousness.
- Inflammation of the pancreas (pancreatitis); symptoms may include sudden pain in the upper abdomen, nausea, vomiting, diarrhea.
- Inflammation of the liver (hepatitis); symptoms may include yellowing of the skin and eyes (jaundice), nausea, vomiting, loss of appetite, general feeling of discomfort, itching, lightly colored urine.
- Irregular heart rate.
- Low platelet count in the blood; this can mean an increased risk of bleeding or bruising.
Tell your doctor immediately if you notice any of the above side effects.
Other side effects:
Tell your doctor, pharmacist, or nurse if you notice any of the following side effects. They are usually mild and tend to disappear as treatment progresses.
Very common(may affect more than 1 in 10 people):
- Diarrhea.
- Abdominal pain.
- Nausea.
- Constipation.
- Flatulence (gas).
- Headache.
- Local pain at the injection site.
Common(may affect up to 1 in 10 people):
- Discomfort in the stomach after eating (dyspepsia).
- Vomiting.
- Feeling of having a full stomach.
- Fatty stools.
- Watery stools.
- Change in stool color.
- Dizziness.
- Lack of appetite.
- Changes in liver function tests.
- Hair loss.
- Difficulty breathing.
- Weakness.
If you experience any side effects, talk to your doctor, nurse, or pharmacist.
Reporting of side effects
If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly through the Spanish Medicines Agency's online platform: http://www.notificaram.es. By reporting side effects, you can help provide more information on the safety of this medicine.
5. Storage of Octreotide Teva
Keep this medicine out of the sight and reach of children.
Store in the original packaging to protect from light.
Store in a refrigerator (between 2°C and 8°C). Do not freeze.
This medicine can be stored below 25°C on the day of injection.
Octreotide Teva should not be stored after reconstitution (it should be used immediately).
Do not use this medicine after the expiry date which is stated on the carton and on the label after EXP. The expiry date is the last day of the month shown.
Do not use this medicine if you notice the presence of particles or a change in color.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help protect the environment.
6. Container Content and Additional Information
Composition of Octreotide Teva
- The active ingredient is octreotide.
A vial contains 10 mg, 20 mg, or 30 mg of octreotide (as octreotide acetate).
- The other components are:
In the powder (vial): poly(DL-lactic-co-glycolic acid) and mannitol (E-421).
In the solvent (pre-filled syringe): sodium carmellose, mannitol (E-421), poloxamer, and water for injectable preparations.
Appearance of Octreotide Teva and Container Content
Octreotide 10 mg: Each container contains a glass vial with 10 mg of octreotide with a rubber stopper sealed with an aluminum cap with a dark blue tab, 1 pre-filled glass syringe with 2 ml of solvent, 1 safety injection needle, and a vial adapter or 3 vials with 10 mg of octreotide each, 3 pre-filled glass syringes with 2 ml of solvent, 3 safety injection needles, and 3 vial adapters.
Octreotide 20 mg: Each container contains a glass vial with 20 mg of octreotide with a rubber stopper sealed with an aluminum cap with an orange tab, 1 pre-filled glass syringe with 2 ml of solvent, 1 safety injection needle, and a vial adapter or 3 vials with 20 mg of octreotide each, 3 pre-filled glass syringes with 2 ml of solvent, 3 safety injection needles, and 3 vial adapters.
Octreotide 30 mg: Each container contains a glass vial with 30 mg of octreotide with a rubber stopper sealed with an aluminum cap with a dark red tab, 1 pre-filled glass syringe with 2 ml of solvent, 1 safety injection needle, and a vial adapter or 3 vials with 30 mg of octreotide each, 3 pre-filled glass syringes with 2 ml of solvent, 3 safety injection needles, and 3 vial adapters.
Only some pack sizes may be marketed.
Marketing Authorization Holder
Teva B.V.
Swensweg 5,
2031GA Haarlem,
Netherlands
Manufacturer
Merckle GmbH
Ludwig-Merckle-Str. 3,
Blaubeuren
89143, Germany
or
PLIVA HRVATSKA d.o.o. (PLIVA CROATIA Ltd.)
Prilaz baruna Filipovicá 25,
Zagreb, 10000
Croatia
or
PHARMATHEN INTERNATIONAL S.A.
Industrial Park Sapes,
Rodopi Prefecture, Block No 5,
Rodopi 69300,
Greece
For further information on this medicinal product, please contact the local representative of the marketing authorization holder:
Teva Pharma, S.L.U.
C/ Anabel Segura, 11, Edificio Albatros B, 1ª planta
28108, Alcobendas, Madrid (Spain)
Date of last revision of this leaflet: March 2022
Detailed and up-to-date information on this medicinal product is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es
------------------------------------------------------------------------------------------------------------------
This information is intended only for healthcare professionals:
How much Octreotide Teva should be used
Acromegaly
Treatment should be initiated with the administration of 20 mg of this medicinal product at intervals of 4 weeks for 3 months. Patients being treated with s.c. octreotide may start treatment with this medicinal product the day after the last dose of s.c. octreotide. Subsequent dose adjustment should be based on serum growth hormone (GH) and insulin-like growth factor 1 (IGF-1) concentrations and clinical symptoms.
For patients in whom clinical symptoms and biochemical parameters (GH; IGF-1) are not fully controlled after a period of 3 months (GH concentrations still above 2.5 micrograms/L), the dose may be increased to 30 mg every 4 weeks. If, after 3 months, GH, IGF-1, and/or symptoms are not adequately controlled at the 30 mg dose, the dose may be increased to 40 mg every 4 weeks.
For patients with GH concentrations consistently below 1 microgram/L and normalized serum IGF-1 concentrations, and in whom most reversible signs/symptoms of acromegaly have disappeared after 3 months of treatment with 20 mg, 10 mg of this medicinal product may be administered every 4 weeks. However, especially in this group of patients, it is recommended to closely monitor serum GH and IGF-1 concentrations and signs/symptoms at this low dose of the medicinal product.
For patients being treated with a stable dose of this medicinal product, GH and IGF-1 assessment should be performed every 6 months.
Gastroenteropancreatic neuroendocrine tumors
- Treatment of patients with symptoms associated with functional gastroenteropancreatic neuroendocrine tumors
Treatment should be initiated with the administration of 20 mg of this medicinal product at intervals of 4 weeks. Patients being treated with s.c. octreotide should continue at the previously effective dose for 2 weeks after the first injection of this medicinal product.
For patients in whom symptoms and biological markers are well-controlled after 3 months of treatment, the dose may be reduced to 10 mg of this medicinal product every 4 weeks.
For patients in whom symptoms are only partially controlled after 3 months of treatment, the dose may be increased to 30 mg of this medicinal product every 4 weeks.
For days when symptoms associated with gastroenteropancreatic tumors may increase during treatment with this medicinal product, additional administration of s.c. octreotide at the previously used dose is recommended. This may occur mainly in the first 2 months of treatment until therapeutic concentrations of octreotide are reached.
- Treatment of patients with advanced neuroendocrine tumors of the intestine or unknown origin where non-intestinal origin has been excluded
The recommended dose of octreotide is 30 mg administered every 4 weeks. Treatment with this medicinal product to control the tumor should be continued in the absence of tumor progression.
Treatment of thyrotropin-secreting adenomas
Treatment with octreotide should be initiated at a dose of 20 mg at intervals of 4 weeks for 3 months before considering a dose adjustment. Thereafter, the dose should be adjusted based on TSH and thyroid hormone response.
Instructions for preparation and intramuscular injection of Octreotide Teva
ONLY FOR INTRAMUSCULAR INJECTION
Injection kit components:
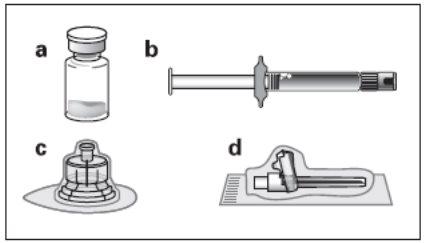
a A vial containing the powder of this medicinal product
b A pre-filled syringe containing the solvent for reconstitution
c A vial adapter for reconstitution of the medicinal product
d A safety injection needle
Follow the instructions below carefully to ensure the reconstitution of this medicinal product before intramuscular injection.
There are three critical steps in the reconstitution process of Octreotide Teva. If not performed correctly, it may result in inadequate administration of the medicinal product.
- The injection kit must reach room temperature.Remove the injection kit from the refrigerator and let it reach room temperature for at least 30 minutes before reconstitution, but not exceeding 24 hours.
- After adding the diluent solution, let the vial stand for 5 minutes to ensure that the powder is completely saturated.
- After saturation, moderately shakethe vial horizontally for at least 30 seconds, until a uniform suspension is formed. The octreotide suspension should only be prepared immediatelybefore administration.
Octreotide Teva must be administered only by an experienced healthcare professional.
Step 1
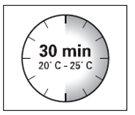
- Remove the injection kit from the refrigerator.
IMPORTANT:It is essential to start the reconstitution process
only after the injection kit has reached room temperature.
Let the kit reach room temperature for at least 30 minutes before reconstitution
but not exceeding 24 hours.
Note: The injection kit can be refrigerated again if necessary.
Step 2
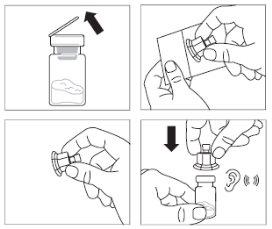
- Remove the plastic tab from the vial and clean
the rubber stopper of the vial with an alcohol swab.
- Remove the protective sleeve from the packaging and remove
the vial adapter from its packaging by holding between
the white luer lock and the plastic packaging.
DO NOTtouch the tip of the access device
anywhere.
- Place the vial on a flat surface. Place the
vial adapter on top of the vial and
press it down completely until it clicks
onto the vial. This will be confirmed when you hear a “click”.
- Clean the tip of the vial adapter with an alcohol swab.
 Step 3
Step 3
- Remove the smooth white cap from the pre-filled syringe
containing the diluent and screw the syringe onto
the vial adapter.
- Slowly press the plunger down until the entire diluent solution
is transferred to the vial.
Step 4
IMPORTANT:It is essential to let the vial stand for 5 minutes
to ensure that the diluent has completely saturated the powder.
Note: It is normal for the plunger to move upward, as there may be overpressure in the vial.
- At this point, prepare the patient for administration.
Step 5
 After the saturation period, ensure that the plunger
After the saturation period, ensure that the plunger
is pressed down to the bottom of the syringe.
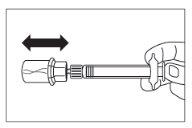
IMPORTANT: Keep the plunger pressed and moderately shake
the vial horizontallyfor at least 30 secondsto ensure that the powder is
completely suspended in the diluent (uniform suspension of milky consistency).
Repeat the moderate shaking for another 30 seconds
if the powder is not completely suspended.
 Step 6
Step 6
- Turn the syringe and vial upside down, and slowly pull the
plunger down until the entire contents of the vial are transferred to the syringe.
- Unscrew the syringe from the vial adapter.
Step 7

- Prepare the injection site with an alcohol swab.
- Screw the safety injection needle onto the syringe.
- If immediate administration is delayed, re-shake
the syringe moderately to ensure a uniform suspension
of milky consistency.
- Remove the protective cap from the needle.
- Gently tap the syringe to displace any visible air bubbles
and expel them from the syringe.
- Proceed immediatelyto Step 8 for patient administration.
Any delay in administration may cause sedimentation.
Step 8
- Octreotide must be administered only by intramuscular injection,
NEVERby intravenous administration.
 Insert the needle completely into the right or left buttock,
Insert the needle completely into the right or left buttock,
forming a 90-degree angle with the skin.
- Slowly aspirate with the plunger to check that a blood vessel
has not been penetrated (if so, change the injection site).
- Using constant pressureon the plunger, slowly administer until
the syringe is empty. Remove the needle from the injection site and
- activate the safety mechanism (as shown in Step 9).
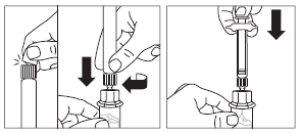
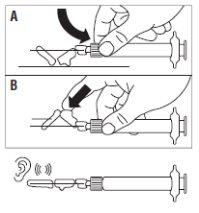 Step 9
Step 9
- Activate the safety mechanism on the needle, using
one of the following two methods:
- either by pressing the articulated section of the safety device
downward onto a rigid surface (Figure A)
- or by pressing the articulated part with a finger (Figure B)
- The sound of a “click” confirms proper activation.
- Note: Record the injection site in the patient's record and
alternate monthly
Discard the syringe immediately (in a sharps container).
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to OCTREOTIDE TEVA 10 mg POWDER AND SOLVENT FOR PROLONGED-RELEASE INJECTABLE SUSPENSIONDosage form: INJECTABLE, Octreotide 100 micrograms/mlActive substance: octreotideManufacturer: Gp Pharm S.A.Prescription requiredDosage form: INJECTABLE, Octreotide 500 micrograms/mlActive substance: octreotideManufacturer: Gp Pharm S.A.Prescription requiredDosage form: INJECTABLE, 200 micrograms/mlActive substance: octreotideManufacturer: Gp Pharm S.A.Prescription required
Online doctors for OCTREOTIDE TEVA 10 mg POWDER AND SOLVENT FOR PROLONGED-RELEASE INJECTABLE SUSPENSION
Discuss questions about OCTREOTIDE TEVA 10 mg POWDER AND SOLVENT FOR PROLONGED-RELEASE INJECTABLE SUSPENSION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions






