
METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSION
Ask a doctor about a prescription for METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSION

How to use METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSION
Introduction
PATIENT INFORMATION LEAFLET
Patient Information Leaflet: Information for the Patient
Metronidazole Noridem 5mg/ml solution for infusion EFG
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
The name of this medicine is Metronidazole Noridem 5mg/ml solution for infusion EFG.
From now on, this leaflet will refer to the medicine as Metronidazole Noridem.
Contents of the pack
- What Metronidazole Noridem is and what it is used for
- What you need to know before you use Metronidazole Noridem
- How to use Metronidazole Noridem
- Possible side effects
- Storage of Metronidazole Noridem
- Contents of the pack and other information
1. What Metronidazole Noridem is and what it is used for
Antibiotics are used to treat bacterial infections and are not effective against viral infections such as the flu or the common cold.
It is essential that you follow the instructions regarding dosage, administration interval, and treatment duration as indicated by your doctor.
Do not store or reuse this medicine. If you have any leftover antibiotic after completing treatment, return it to the pharmacy for proper disposal. Do not throw medicines down the drain or into the trash.
Metronidazole Noridem belongs to a group of medicines known as antibioticsand is used to treat severe infections caused by bacteria that can be destroyed by the active ingredient metronidazole.
It is possible that you will be given Metronidazole Noridem for the treatment of one of the following diseases:
- Infections of the blood, brain, lungs, bones, genital tract, pelvic area, liver, intestine, and stomach.
In case of necessity, your treatment may be complemented with other antibiotics. Metronidazole Noridem may be administered as a preventive measure before surgical interventions that involve a high risk of infection by what is known as anaerobic bacteria, mainly in gynecology or stomach and intestinal surgery.
2. What you need to know before you use Metronidazole Noridem
Do not use Metronidazole Noridem
- if you are allergic to metronidazole, to other similar substances, or to any of the other components of this medicine (listed in section 6).
Warnings and precautions
Consult your doctor, pharmacist, or nurse before starting treatment with Metronidazole Noridem if you have:
- Severe liver damage
- A blood disorder or
- A brain, spinal cord, or neurological disease
Therefore, your doctor will very carefully determine whether you should receive treatment with Metronidazole Noridem.
If, during treatment, obvious signs of seizures or any other type of nervous disorder (e.g., numbness of the legs) appear, your treatment will be reviewed as soon as possible.
If you suffer from severe diarrhea, which may be due to a serious disease of the large intestine called "pseudomembranous colitis", treatment should be discontinued or reviewed immediately (see also section 4). Since prolonged use of metronidazole can negatively affect blood cell formation (see section 4), your blood cell counts will be monitored during treatment.
If you receive this medicine, your urine may darken.
There have been reports of severe liver toxicity/liver failure, with a fatal outcome, in patients with Cockayne syndrome who took products containing metronidazole.
If you have Cockayne syndrome, your doctor should also closely monitor liver function while you are receiving treatment with metronidazole and after treatment.
If you develop any of the following symptoms, inform your doctor immediately and stop taking metronidazole:
- Stomach pain, loss of appetite, nausea, vomiting, fever, discomfort, fatigue, jaundice, dark urine, clay-colored stools, or itching.
Generally, treatment with Metronidazole Noridem should not be continued for more than 10 days. The treatment period will only be extended in exceptional circumstances and only if absolutely necessary. Repeated treatment with metronidazole will be restricted to cases where it is absolutely necessary. If this is the case, you will be subject to rigorous monitoring.
Other medicines and Metronidazole Noridem
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
Amiodarone (used to treat irregular heartbeats)
If you receive this medicine, your heart function should be monitored. If you notice any abnormality in heart function, dizziness, or fainting, you should see a doctor.
Barbiturates (the active ingredient in sleeping pills)
Phenobarbital reduces the duration of action of metronidazole, so it may be necessary to increase the dose of metronidazole.
Contraceptive pill
The contraceptive pill you are taking may be less effective while you are being treated with metronidazole.
Busulfan
Metronidazole should not be administered to patients who are receiving busulfan because the likelihood of toxic effects is higher in this case.
Carbamazepine (a medicine for the treatment of epilepsy)
Caution should be exercised when administering this combination because metronidazole may increase the duration of action of carbamazepine.
Cimetidine (a medicine for the treatment of digestive disorders)
Cimetidine may reduce the elimination of metronidazole in isolated cases and, as a consequence, cause an increase in metronidazole serum concentrations.
Coumarin derivatives (medicines that inhibit blood coagulation)
Metronidazole may enhance the inhibition of blood coagulation exerted by coumarins. Therefore, if you are taking a medicine that inhibits blood clot formation (e.g., warfarin), you may need a lower dose during treatment with metronidazole.
Cyclosporine (a medicine used to suppress undesirable immune responses)
When administered simultaneously with metronidazole, cyclosporine blood levels may increase, so your doctor will need to adjust your cyclosporine dose accordingly.
Disulfiram (used in the treatment of alcohol withdrawal)
If you are taking disulfiram, you should not receive metronidazole, or disulfiram treatment should be discontinued. The combined use of these two medicines can cause confusion up to the point of severe mental disorder (psychosis).
Medicines containing alcohol
See the section "Use of Metronidazole Noridem with food, drinks, and alcohol".
Fluorouracil (an anticancer medicine)
The daily dose of fluorouracil may need to be reduced when administered with metronidazole because metronidazole may cause an increase in fluorouracil blood levels.
Lithium (used to treat mental illnesses)
Treatment with lithium-containing preparations requires close monitoring, especially during treatment with metronidazole, and the dose of the lithium-containing preparation may need to be adjusted. Before administering metronidazole, lithium treatment should be gradually reduced or discontinued.
Mycophenolate mofetil (used to prevent rejection reactions after organ transplantation)
Metronidazole may weaken its effect, so close monitoring of the effect of the medicine is recommended.
Phenytoin (a medicine for the treatment of epilepsy)
If you are taking phenytoin, your doctor will treat you with metronidazole with caution because metronidazole may increase the duration of action of phenytoin. On the other hand, phenytoin may reduce the effect of metronidazole.
Tacrolimus (used to suppress undesirable immune responses)
When starting and stopping treatment with metronidazole, your blood levels of this medicine and kidney function should be monitored.
Use of Metronidazole Noridem with food, drinks, and alcohol
Alcohol
While you are being treated with metronidazole and up to 48 hours after administration, you should not consume any type of alcoholic beverage or medicine that contains alcohol because it can cause intolerance reactions, such as dizziness and vomiting.
Pregnancy, breastfeeding, and fertility
If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before using this medicine.
Fertility
Studies in animals have only indicated a possible negative influence of metronidazole on the male reproductive system when high doses were administered, far above the maximum recommended dose in humans.
Contraception in men and women
If you are taking a contraceptive pill, see the section "Other medicines and Metronidazole Noridem".
Pregnancy
If you are pregnant, your doctor will not treat you with metronidazole unless it is considered absolutely necessary.
Breastfeeding
During treatment with metronidazole, you should not breastfeed, nor should you resume breastfeeding until 2-3 days have passed since the end of treatment because metronidazole is excreted in breast milk.
Driving and using machines
During treatment with Metronidazole Noridem, you may feel drowsy, dizzy, confused, see or hear things that do not exist (hallucinations), have seizures, or experience temporary vision problems (such as blurred or double vision). If you experience these effects, do not drive or use tools or machines.
Metronidazole Noridem contains sodium.
This medicine contains 310.58 mg of sodium (the main component of table/cooking salt) per 100 ml. This is equivalent to 15.5% of the maximum recommended daily sodium intake for an adult.
3. How to use Metronidazole Noridem
Posology
The dose depends on the nature and severity of the disease you are suffering from, your age, and your body weight, as well as your response to treatment.
Generally, the following dosage regimens are prescribed:
Adults and adolescents
Treatment of amoebiasis
1.50 g per day (500 mg three times a day, intravenous infusions).
Treatment of infections
Adults
You will be administered 100 ml of medicine (500 mg of metronidazole) every 8 hours.
In most cases, treatment will last 7 days. Only exceptionally will the treatment be prolonged, although it should not normally exceed 10 days.
The dose will be the same as for patients with kidney disease.
In the case of patients with liver disease, lower doses may be necessary.
If you have been treated with a hemodialysis machine, your doctor will schedule the infusion after the dialysis has finished. It is not necessary to adjust the usual dose.
Prevention of infections that may arise after surgery
If used in the prevention of infections during surgery, you may be administered 500 mg of the medicine before surgery. The dose will be repeated 8 and 16 hours after surgery.
Elderly patients
Your doctor will administer this medicine to you with special caution.
Use in children
The dose in children is based on body weight (BW).
Treatment of amoebiasis
35-50 mg/kg/day intravenously, divided into 3 doses, for 5-10 days. The maximum dose should not exceed 2,400 mg/day.
Treatment of infections
Age | Posology |
From 8 weeks to 12 years | 20-30 mg of metronidazole per kg of body weight per day, in a single dose or divided into 7.5 mg of metronidazole per kg of body weight every 8 hours. If the infection is severe, the daily dose may be increased to 40 mg of metronidazole per kg of body weight. |
Less than 8 weeks | 15 mg of metronidazole per kg of body weight in a single daily dose or divided into 7.5 mg/kg of body weight every 12 hours. |
Neonates less than 40 weeks of gestational age | Since metronidazole can accumulate in these patients during the first weeks of life, metronidazole blood levels will be checked a few days after treatment. |
Generally, treatment will last 7 days.
Prevention of infections that may arise after surgery:
Age | Posology |
Less than 12 years | 20-30 mg of metronidazole per kg of body weight in a single dose administered 1-2 hours before surgery |
Neonates less than 40 weeks of gestational age | 10 mg of metronidazole per kg of body weight in a single dose before surgery |
Method of administration and duration of treatment
Metronidazole Noridem is administered through a drip directly into a vein (intravenous infusion).
The infusion of a vial usually lasts 60 minutes, but it should not be administered in less than 20 minutes.
The total treatment period with metronidazole is usually 7 days and should not exceed 10 days, unless absolutely necessary (see also the section "Warnings and precautions"). If you are receiving other antibiotics at the same time, your doctor will administer those medicines separately.
If you use more Metronidazole Noridem than you should:
The side effects described in the next section may appear as signs or symptoms of an overdose. There have been reports of attempted suicide and accidental overdose with single oral doses of metronidazole of up to 12 g.
Symptoms were limited to vomiting, ataxia, and mild disorientation.
There is no known antidote or specific treatment for a massive overdose, but metronidazole can be removed from the body through dialysis (treatment with a hemodialysis machine).
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them.
Adverse effects appear mainly with high doses or with prolonged use.
If you notice any of the following side effects, talk to your doctor immediately:
Rare(may affect up to 1 in 1000 people):
- Persistent severe diarrhea (possibly a symptom of a severe intestinal infection called pseudomembranous colitis; see the paragraph Emergency treatment of pseudomembranous enterocolitis)
- Severe acute hypersensitivity reactions, including anaphylactic shock
Very rare(may affect up to 1 in 10,000 people):
- White blood cell and platelet counts may decrease during treatment (granulocytopenia, agranulocytosis, pancytopenia, thrombocytopenia)
- Hepatitis (inflammation of the liver), jaundice, liver inflammation
- Cerebral disorders, lack of coordination
- Non-bacterial meningitis (aseptic meningitis)
- Severe inflammatory rash on mucous membranes and skin, accompanied by fever, redness, and blistering (in extreme cases, even skin detachment in extended areas (Stevens-Johnson syndrome))
Frequency not known(cannot be estimated from available data):
- Mild to moderate hypersensitivity reactions, swelling of the face, mouth, throat, or tongue (angioedema)
- Ocular spasms, damage, or inflammation of the eye nerves
- Reduced white blood cell count (leukopenia), severe anemia (aplastic anemia)
- Seizures, nervous disorders, such as numbness, pain, feeling of agitation, and tingling in the arms or legs
- Toxic epidermal necrolysis
- Acute liver failure in patients with Cockayne syndrome (see the "Warnings and precautions" section of section 2)
Other adverse effects include
Frequent(may affect up to 1 in 10 people):
- Fungal infections (e.g., genital infections)
Uncommon(may affect up to 1 in 100 people):
- Darkening of urine (due to a metronidazole metabolite)
Rare(may affect up to 1 in 1000 people):
- Changes in ECG
Very rare(may affect up to 1 in 10,000 people):
- Psychotic disorders, including confusion and hallucination states
- Headache, dizziness, drowsiness, fever, alteration of vision and movement, vertigo, speech disorders, seizures
- Visual disorders, e.g., blurred vision, short-sightedness
- Liver function disorders (such as elevated serum levels of certain enzymes and bilirubin)
- Cutaneous allergic reactions, such as itching, urticaria
- Joint or muscle pain
Frequency not known(cannot be estimated from available data):
- Dizziness, nausea, diarrhea, inflammation of the tongue or mouth, belching, and bitter taste, metallic taste, pressure above the stomach, pasty tongue
- Difficulty swallowing
- Anorexia
- Sadness (depressive state)
- Drowsiness or insomnia, muscle spasms
- Redness and itching of the skin (erythema multiforme)
- Irritation of the walls of the veins (up to the point of presenting inflamed and thrombosed veins) after intravenous administration, weakness, fever
Emergency treatment of pseudomembranous enterocolitis
In the event of persistent severe diarrhea, you should inform your doctor as soon as possible because it could be due to pseudomembranous colitis, which is a serious disease that needs to be treated immediately. Your doctor will discontinue metronidazole treatment and provide appropriate treatment.
If any of these adverse effects become severe or you experience any adverse effect not listed in this leaflet, inform your doctor.
Reporting of adverse effects
If you experience adverse effects, consult your doctor, pharmacist, or nurse, even if they are not listed in this leaflet. You can also report them directly through the Spanish Pharmacovigilance System for Human Use Medicines: www.notificaram.es. By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Storage of Metronidazole Noridem
- Keep this medicine out of the sight and reach of children.
- Do not use this medicine after the expiration date stated on the carton and vial after "EXP". The expiration date is the last day of the month indicated.
- This medicine does not require special storage conditions.
After the first opening, the medicine should be used immediately. For single use.
Do not use this medicine if the packaging has leaks or the solution is not transparent.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of the packaging and medicines you no longer need. This will help protect the environment.
6. Package Contents and Additional Information
What Metronidazole Noridem contains
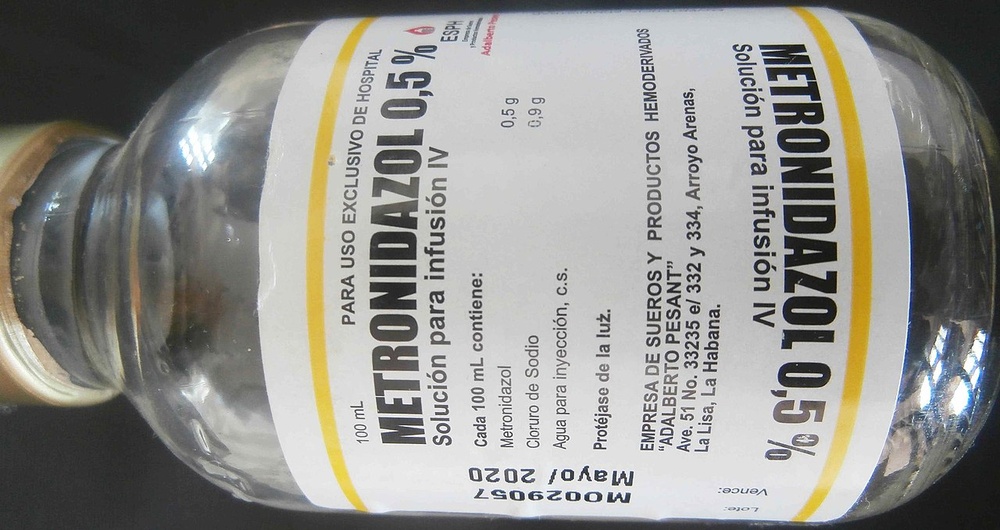
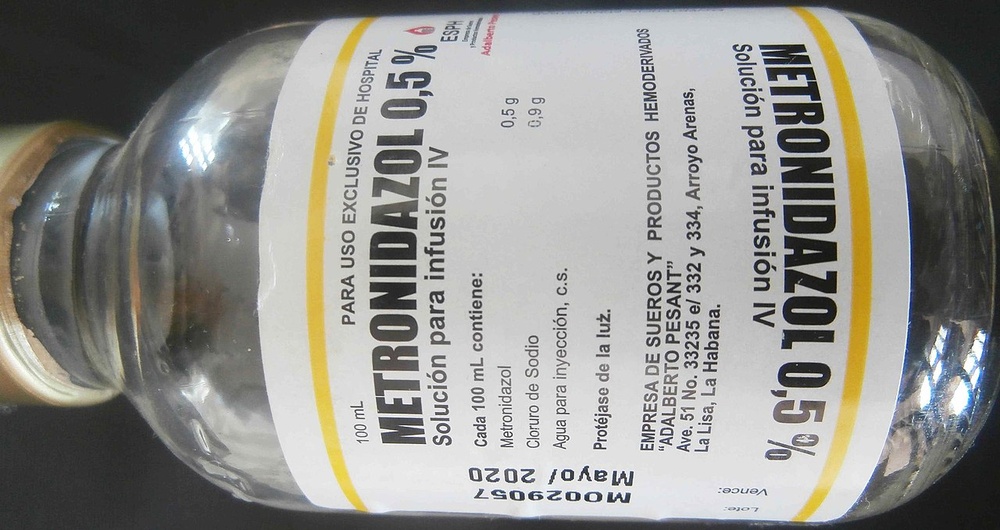
- The active ingredient is metronidazole. Each vial of solution for infusion contains 500 mg of metronidazole.
Each milliliter of solution for infusion contains 5 mg of metronidazole.
- The other ingredients (excipients) are sodium hydrogen phosphate dodecahydrate, citric acid monohydrate, sodium chloride, and water for injectable preparations.
Appearance of the product and package contents
This medicine is presented as a solution for intravenous infusion, colorless to light yellow, in a polypropylene blown vial, filled and sealed, with a capacity of 100 ml, with a sealed cap of molded plastic with a rubber gasket and a tear-off ring or a plastic cap with a double port.
Metronidazole Noridem is available in packs of 10, 20, or 24 vials.
Not all pack sizes may be marketed.
Marketing authorization holder and manufacturer
Marketing authorization holder
Noridem Enterprises Limited
Evagorou & Makariou
Mitsi Building 3, Office 115
1065 Nicosia, Cyprus
Manufacturer
DEMO S.A. PHARMACEUTICAL INDUSTRY
21st Km National Road Athens-Lamia.
14568 Greece
This medicine is authorized in the Member States of the European Economic Area and in the United Kingdom (Northern Ireland) under the following names:
Netherlands: | Metronidazole Noridem 5 mg/ml, oplossing voor infusie |
United Kingdom (Northern Ireland): | Metronidazole 500 mg/100 mL Solution for infusion |
Austria: | Metronidazole BRADEX 5 mg/ml Infusionslösung |
Belgium: | Metronidazole Noridem 500mg/100ml, oplossing voor infusie / solution pour perfusion / Infusionslösung |
France: | METRONIDAZOLE NORIDEM 500 mg/100 ml, solution pour perfusion |
Hungary: | Metronidazol Noridem 5 mg / ml oldatos infúzió |
Slovakia: | Metronidazole Noridem 5 mg/ml infúzny roztok |
Czech Republic: | Metronidazole Noridem |
Luxembourg: | METRONIDAZOLE NORIDEM 500 mg/100 ml, solution pour perfusion |
Croatia: | Metronidazol Noridem 5 mg/ml otopina za infuziju |
Slovenia: | Metronidazol Noridem Enterprises 5 mg/ml raztopina za infundiranje |
Denmark: | Metronidazole Noridem |
Spain: | Metronidazol Noridem 5 mg/ml solución para perfusión EFG |
Finland: | Metronidazole Noridem 5 mg/ml infuusioneste, liuos |
Ireland: | Metronidazole 5 mg/ml solution for infusion |
Italy: | Metronidazol Noridem |
Norway: | Metronidazole Noridem |
Poland: | Metronidazol Noridem |
Portugal: | Metronidazol Noridem |
Romania: | Metronidazol Noridem 5 mg/ml solutie perfuzabila |
Sweden: | Metronidazole Noridem |
Date of last revision of this leaflet:September 2024
Detailed information on this medicine is available on the website of the Spanish Agency for Medicines and Health Products (AEMPS) http://www.aemps.gob.es/
This information is intended only for healthcare professionals:
Posology and method of administration
Posology
The dosage regimen is adjusted according to the individual patient's response to treatment, age, and body weight, as well as the nature and severity of the disease.
The following dosage recommendations should be followed:
Adults and adolescents:
Amebiasis
1.50 g per day (500 mg three times a day, intravenous infusions).
In the case of hepatic amebiasis, in the infectious resistant stage (abscess), the abscess should be evacuated simultaneously with metronidazole treatment. Duration of treatment: 5-10 days
Treatment of anaerobic infections
500 mg (100 ml) every 8 hours. Alternatively, 1,000-1,500 mg per day can be administered in a single dose.
The duration of treatment depends on the effect of the treatment. In most cases, a treatment period of 7 days is sufficient. If clinically indicated, treatment can be extended, although it is generally not recommended to exceed 10 days of treatment.
Prophylaxis against post-surgical infections caused by anaerobic bacteria:
500 mg, with the final administration completed approximately 1 hour before surgery. The dose is repeated after 8 and 16 hours.
Elderly patients:
Caution is recommended in the elderly patient population, especially with high doses, although available information on dose modification is limited.
Pediatric population
Amebiasis
35-50 mg/kg/day by intravenous route, divided into 3 doses, for 5-10 days. The maximum dose should not exceed 2,400 mg/day.
In the case of hepatic amebiasis, in the infectious resistant stage (abscess), the abscess should be evacuated simultaneously with metronidazole treatment.
Treatment of anaerobic infections
Children > 8 weeks to 12 years of age:
The usual daily dose is 20-30 mg/kg of body weight per day, in a single dose or divided into 7.5 mg/kg of body weight every 8 hours. The daily dose can be increased to 40 mg/kg, depending on the severity of the infection.
Neonates and infants <8 weeks of age:< p>
15 mg/kg of body weight per day, in a single dose, or divided into 7.5 mg/kg of body weight every 12 hours.
In the case of neonates with a gestational age of less than 40 weeks, metronidazole accumulation may occur during the first week of life. Therefore, it is recommended to monitor serum metronidazole concentrations after several days of treatment.
The duration of treatment is usually 7 days.
Prophylaxis against post-surgical infections caused by anaerobic bacteria:
Children <12 years:< p>
20-30 mg/kg of body weight, in a single dose, administered 1-2 hours before surgery.
Neonates with a gestational age of less than 40 weeks:
10 mg/kg of body weight, in a single dose, before surgery.
Patient with renal insufficiency
Available data are limited in this patient population. These data do not indicate the need for a dose reduction.
In patients undergoing hemodialysis, the usual dose of metronidazole should be scheduled after hemodialysis on dialysis days to compensate for the elimination of metronidazole during the procedure.
In patients with renal insufficiency undergoing intermittent peritoneal dialysis (IPD) or continuous ambulatory peritoneal dialysis (CAPD), no routine dose adjustment is necessary.
Patient with hepatic insufficiency
Since the serum half-life is prolonged and plasma clearance is delayed in severe hepatic insufficiency, patients with severe liver disease will require lower doses.
In the case of patients with hepatic encephalopathy, the daily dose should be reduced to one-third and can be administered once a day.
Method of administration
Intravenous route.
The contents of a vial should be infused intravenously slowly, i.e., 100 ml at most over a period of at least 20 minutes, although usually 1 hour.
Antibiotics prescribed simultaneously should be administered separately.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSIONDosage form: ORAL SOLUTION/SUSPENSION, 125 mg metronidazole benzoateActive substance: metronidazoleManufacturer: Laboratorios Fidia Farmaceutica S.L.Prescription requiredDosage form: TABLET, 250 mgActive substance: metronidazoleManufacturer: Laboratorios Fidia Farmaceutica S.L.Prescription requiredDosage form: INJECTABLE PERFUSION, 5 mg/mlActive substance: metronidazoleManufacturer: Altan Pharmaceuticals SaPrescription required
Alternatives to METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSION in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSION in Poland
Alternative to METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSION in Ukraine
Online doctors for METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSION
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for METRONIDAZOL NORIDEM 5 mg/ml SOLUTION FOR INFUSION – subject to medical assessment and local rules.














