Lonquex 6mg injectable solution


How to use Lonquex 6mg injectable solution
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the Patient
Lonquex 6 mg Solution for Injection in Pre-filled Syringe
lipegfilgrastim
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor, pharmacist, or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the Pack
- What is Lonquex and what is it used for
- What you need to know before you use Lonquex
- How to use Lonquex
- Possible side effects
- Storing Lonquex
- Contents of the pack and other information
1. What is Lonquex and what is it used for
What is Lonquex
Lonquex contains the active substance lipegfilgrastim. Lipegfilgrastim is a long-acting protein produced by biotechnology in a bacterium called Escherichia coli.
It belongs to a group of proteins called cytokines and is similar to a natural protein (granulocyte-colony stimulating factor [G-CSF]) produced by your own body.
What is Lonquex used for
Lonquex is used in adults and in children from 2 years of age.
Your doctor has prescribed Lonquex to you or your child to reduce the duration of a condition called neutropenia (low white blood cell count) and the occurrence of febrile neutropenia (low white blood cell count with fever). These problems can be caused by the use of cytotoxic chemotherapy (medicines that destroy fast-growing cells).
How Lonquex works
Lipegfilgrastim stimulates the bone marrow (the tissue where new blood cells are made) to produce more white blood cells. White blood cells are important because they help your body fight infections. These cells are very sensitive to the effects of chemotherapy, which can cause their numbers to decrease in the body. If white blood cells fall to a low level, there may not be enough in the body to fight against bacteria and you may be at a higher risk of getting infections.
2. What you need to know before you use Lonquex
Do not use Lonquex
- if you or your child is allergic to lipegfilgrastim or any of the other ingredients of this medicine (listed in section 6).
Warnings and precautions
Talk to your doctor, pharmacist, or nurse before you start using Lonquex:
- if you or your child notices pain in the upper left side of the abdomen or at the top of the shoulder. It could be due to a spleen disorder (see section 4 “Possible side effects”).
- if you or your child has a cough, fever, and difficulty breathing. It could be due to a lung disorder (see section 4 “Possible side effects”).
- if you or your child has sickle cell anaemia or sickle cell disease, which is a hereditary disease characterized by red blood cells with a sickle shape.
- if you or your child has previously experienced allergic reactions to other medicines similar to this one (e.g. filgrastim, lenograstim, or pegfilgrastim from the G-CSF group). There may also be a risk of reaction to Lonquex.
Your doctor will perform regular blood tests to monitor various blood components and their concentrations. Your doctor will also periodically check your urine or your child’s urine, as other medicines similar to this one (e.g. other granulocyte-colony stimulating factors such as filgrastim, lenograstim, or pegfilgrastim) may damage the small filters in the kidneys (glomerulonephritis; see section 4 “Possible side effects”).
Tell your doctor if you or your child is receiving treatment for breast cancer or lung cancer combined with chemotherapy and/or radiotherapy and has symptoms such as tiredness, fever, easy bruising, or bleeding. These symptoms may be due to a pre-cancerous blood disorder called myelodysplastic syndrome (MDS) or a blood cancer called acute myeloid leukaemia (AML), which have been associated with another medicine like this (pegfilgrastim from the G-CSF group).
Rarely, inflammation of the aorta (the large blood vessel that carries blood from the heart to the rest of the body) has been reported with other medicines like this (e.g. filgrastim, lenograstim, or pegfilgrastim from the G-CSF group). The symptoms may include fever, abdominal pain, general discomfort, back pain, and increased inflammatory markers. Tell your doctor if you experience these symptoms.
Children and adolescents
Lonquex is not recommended in children below 2 years of age.
Other medicines and Lonquex
Tell your doctor or pharmacist if you or your child is using, has recently used, or might use any other medicines.
Pregnancy and breastfeeding
Lonquex has not been studied in pregnant women. It is important that you tell your doctor if you are pregnant, think you may be pregnant, or plan to become pregnant, as your doctor may decide that you should not use this medicine.
It is not known whether the active substance of this medicine passes into breast milk. Therefore, you must stop breastfeeding during treatment.
Driving and using machines
Lonquex has no or negligible influence on your ability to drive and use machines.
Lonquex contains sorbitol
This medicine contains 30 mg of sorbitol in each pre-filled syringe.
Lonquex contains sodium
This medicine contains less than 1 mmol of sodium (23 mg) per pre-filled syringe, which is essentially “sodium-free”.
3. How to use Lonquex
Follow the administration instructions of this medication exactly as indicated by your doctor or pharmacist. In case of doubt, consult your doctor or pharmacist again.
What is the recommended dose
The recommended dose is a pre-filled syringe (6 mg of lipegfilgrastim) once per chemotherapy cycle.
The pre-filled syringe is only suitable for adults or for children who weigh 45 kg or more.
Lonquex is also available in a vial presentation for children who weigh less than 45 kg. The recommended dose will be based on their body weight and a doctor or nurse will administer the appropriate dose.
When to use Lonquex
The dose of Lonquex is usually injected approximately 24 hours after the last dose of chemotherapy, at the end of each chemotherapy cycle.
How are the injections administered?
This medication is administered in the form of an injection using a pre-filled syringe. The injection is administered into the tissue just below the skin (subcutaneous injection).
Your doctor may suggest that you learn to self-inject this medication or administer the injection to your child. Your doctor or nurse will indicate how to do it. Do not attempt to self-administer Lonquex or administer it to your child without having received the necessary training for it. The necessary information to use the pre-filled syringe can be found in the section "Information for self-injection or injecting your child". However, the proper treatment of your disease or your child's disease requires constant and close collaboration with your doctor.
Information for self-injection or injecting your child
This section contains information on how to self-administer or administer to your child an injection of Lonquex under the skin. It is essential that you do not attempt to self-administer or administer the injection to your child unless you have received special training from your doctor or nurse. If you have doubts about self-administering the injection or wish to ask a question, ask your doctor or nurse for help.
How to use Lonquex
You must self-administer or administer the injection to your child in the tissue just below the skin. This procedure is called subcutaneous injection.
Necessary equipment
To self-administer or administer the injection to your child in the tissue under the skin, you will need:
- a pre-filled syringe of Lonquex;
- a cotton swab with alcohol;
- a piece of gauze or a sterile gauze pad;
- a container for sharp objects (a plastic container provided by the hospital or pharmacy) in which to safely dispose of used syringes.
What to do before the injection
- Remove the medication from the refrigerator.
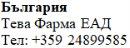
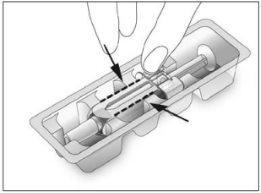
- Open the blister pack and remove the pre-filled syringe (see Figure 1). Do not grasp the pre-filled syringe by the plunger or the needle cover.
- Check the expiration date on the label of the pre-filled syringe (EXP). Do not use it if the date is after the last day of the month indicated.
- Check the appearance of Lonquex. It should be a clear and colorless liquid. If it contains particles or is cloudy, do not use it.
- Do not shake Lonquex vigorously, as this may alter its activity.
- For a more comfortable injection:
- let the pre-filled syringe rest for 30 minutes to reach room temperature (not above 25°C) or
- hold it gently in your hand for a few minutes.
Do notheat Lonquex in any other way (e.g., do not heat it in the microwave or in hot water).
- Do notremove the needle cover from the syringe until you are ready to administer the injection.
- Find a comfortable and well-lit place. Place everything you need easily accessible (the pre-filled syringe of Lonquex, a cotton swab with alcohol, a piece of gauze or a sterile gauze pad, and the container for sharp objects).
- Wash your hands thoroughly.
 1
1
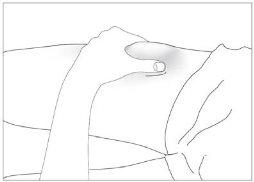
Where to administer the injection
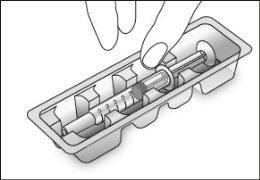
The most suitable places for the injection are:
- the upper part of the thighs;
- the abdomen (see the gray areas in Figure 2), avoiding the skin that immediately surrounds the navel.
 2
2
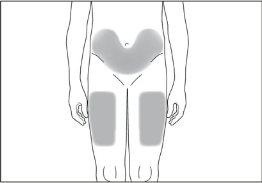
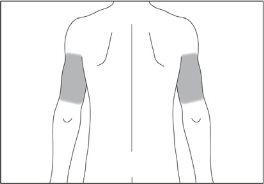
If someone else is going to administer the injection to you or you are going to administer the injection to your child, you can also use the following places:
- the posterior and lateral area of the upper part of the arms (see the gray areas in Figures 3 and 4).
 3
3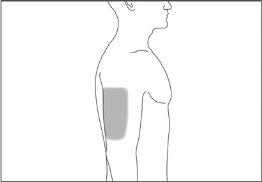 4
4
How to prepare the injection
Before self-administering or administering an injection of Lonquex to your child, you must perform the following steps:
- Disinfect the skin at the injection site using a cotton swab with alcohol.
- Hold the syringe and gently remove the needle cover without twisting it. Pull it straight as shown in Figures 5 and 6. Do not touch the needle or push the plunger.
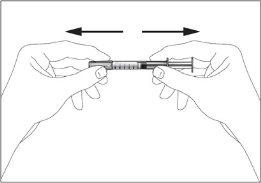 5
5 6
6
- You may notice small air bubbles in the pre-filled syringe. If there are any, hold the syringe with the needle facing up (see Figure 7), gently tap the syringe with your fingers until they rise to the top of the syringe. With the syringe facing up, expel all the air from it by slowly pushing the plunger up.
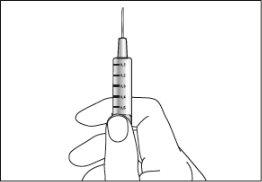 7
7
- Now you can use the pre-filled syringe.
How to self-administer or administer the injection to your child
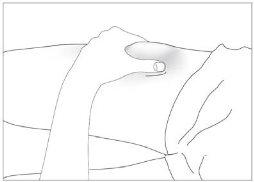
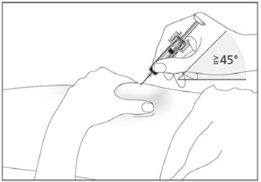
- Pinch the disinfected skin between your index and thumb fingers without squeezing it (see Figure 8).
- Insert the needle completely into the skin as indicated by your doctor or nurse. The angle between the syringe and the skin should not be too narrow (at least 45°, see Figure 9).
- Inject the liquid into the tissue slowly and evenly, keeping the skin pinched at all times.
- After injecting the liquid, remove the needle and release the skin.
- Press on the injection site with a piece of gauze or a sterile gauze pad for several seconds.
- Use each syringe for a single injection. Do not use any remaining Lonquex in the syringe.
 8
8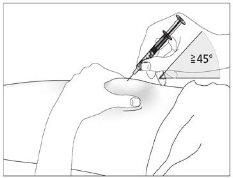 9
9
Remember
If you have any problems, ask your doctor or nurse for help and advice.
Disposal of used syringes
- Do not replace the needle cover on used needles.
- Insert the used syringes into the container for sharp objects and keep this container out of sight and reach of children.
- Dispose of the full container for sharp objects as indicated by your doctor, pharmacist, or nurse.
- Never throw away used syringes in the regular household trash.
Information for self-injection or injecting your child
This section contains information on how to self-administer or administer to your child an injection of Lonquex under the skin. It is essential that you do not attempt to self-administer or administer the injection to your child unless you have received special training from your doctor or nurse. If you have doubts about self-administering the injection or wish to ask a question, ask your doctor or nurse for help.
How to use Lonquex
You must self-administer or administer the injection to your child in the tissue just below the skin. This procedure is called subcutaneous injection.
Necessary equipment
To self-administer or administer the injection to your child in the tissue under the skin, you will need:
- a pre-filled syringe of Lonquex;
- a cotton swab with alcohol;
- a piece of gauze or a sterile gauze pad.
What to do before the injection
- Remove the medication from the refrigerator.
- Open the blister pack and remove the pre-filled syringe (see Figure 1). Do not grasp the pre-filled syringe by the plunger or the needle cover. This could damage the safety device.
- Check the expiration date on the label of the pre-filled syringe (EXP). Do not use it if the date is after the last day of the month indicated.
- Check the appearance of Lonquex. It should be a clear and colorless liquid. If it contains particles or is cloudy, do not use it.
- Do not shake Lonquex vigorously, as this may alter its activity.
- For a more comfortable injection:
- let the pre-filled syringe rest for 30 minutes to reach room temperature (not above 25°C) or
- hold it gently in your hand for a few minutes.
Do notheat Lonquex in any other way (e.g., do not heat it in the microwave or in hot water).
- Do notremove the needle cover from the syringe until you are ready to administer the injection.
- Find a comfortable and well-lit place. Place everything you need easily accessible (the pre-filled syringe of Lonquex, a cotton swab with alcohol, and a piece of gauze or a sterile gauze pad).
- Wash your hands thoroughly.
 1
1
Where to administer the injection
The most suitable places for the injection are:
- the upper part of the thighs;
- the abdomen (see the gray areas in Figure 2), avoiding the skin that immediately surrounds the navel.
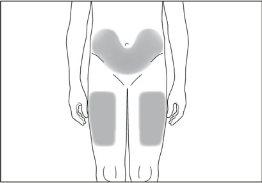 2
2
If someone else is going to administer the injection to you or you are going to administer the injection to your child, you can also use the following places:
- the posterior and lateral area of the upper part of the arms (see the gray areas in Figures 3 and 4).
 3
3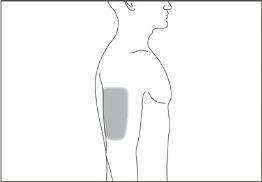 4
4
How to prepare the injection
Before self-administering or administering an injection of Lonquex to your child, you must perform the following steps:
- Disinfect the skin at the injection site using a cotton swab with alcohol.
- Hold the syringe and gently remove the needle cover without twisting it. Pull it straight as shown in Figures 5 and 6. Do not touch the needle or push the plunger.
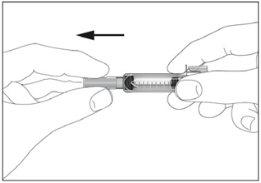 5
5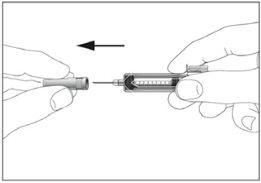 6
6
- You may notice small air bubbles in the pre-filled syringe. If there are any, hold the syringe with the needle facing up (see Figure 7), gently tap the syringe with your fingers until they rise to the top of the syringe. With the syringe facing up, expel all the air from it by slowly pushing the plunger up.
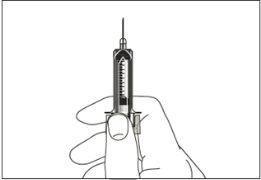 7
7
- Now you can use the pre-filled syringe.
How to self-administer or administer the injection to your child
- Pinch the disinfected skin between your index and thumb fingers without squeezing it (see Figure 8).
- Insert the needle completely into the skin as indicated by your doctor or nurse. The angle between the syringe and the skin should not be too narrow (at least 45°, see Figure 9).
- Inject the liquid into the tissue slowly and evenly, keeping the skin pinched at all times (see Figure 10).
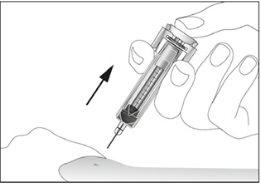
- Push the plunger to the maximum to inject all the liquid. With the plunger still pressed to the maximum, remove the needle from the skin (see Figure 11). Then, release the plunger. The safety device will activate immediately. The entire needle and syringe will automatically retract and be covered, so you cannot prick yourself (see Figure 12).
- Press on the injection site with a piece of gauze or a sterile gauze pad for several seconds.
- Each pre-filled syringe is for single use.
 8
8
 9
9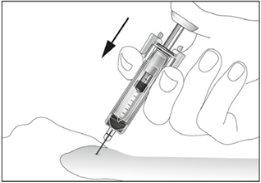 10
10
 11
11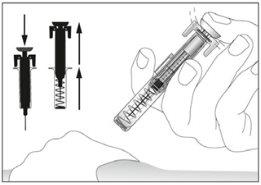 12
12
Remember
If you have any problems, ask your doctor or nurse for help and advice.
If you use more Lonquex than you should
If you use more Lonquex than you should, consult your doctor.
If you forget to use Lonquex
If you have missed an injection, contact your doctor to find out when you should inject or have your child injected with the next dose.
If you have any other questions about the use of this medication, ask your doctor, pharmacist, or nurse.
4. Possible adverse effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them.
More serious adverse effects
- Rarely (may affect up to 1 in 100 people), allergic reactions, such as skin rash, elevated and itchy areas on the skin, and severe allergic reactions with weakness, low blood pressure, difficulty breathing, and swelling of the face have been reported. If you think you are experiencing this type of reaction, you should stop injecting Lonquex and seek immediate medical attention.
- Rare cases of increased spleen size and spleen rupture with other medicines similar to Lonquex have been reported. Some cases of spleen rupture were fatal. It is essential that you contact your doctor immediately if you notice pain in the upper left side of the abdomen or in the left shoulder,as these symptoms may be related to a spleen problem.
- Cough, fever, and difficulty or pain when breathing may be signs of rare, severe pulmonary adverse effects, such as pneumonia and acute respiratory distress syndrome, which can be fatal. If you have a fever or any of these symptoms, it is essential that you contact your doctor immediately.
- Contact your doctor immediately if you experience any of the following symptoms: swelling that may be associated with less frequent urination, difficulty breathing, swelling, and feeling of abdominal fullness, and a general feeling of tiredness. These symptoms usually develop very quickly.
These may be symptoms of a disease with an unknown frequency (cannot be estimated from the available data) called "capillary leak syndrome", which causes blood to leak from the small blood vessels in your body and requires urgent medical attention.
Other adverse effects
Very common (may affect more than 1 in 10 people)
- Musculoskeletal pain, such as bone pain and pain in the joints, muscles, limbs, chest, neck, or back. Inform your doctor if you experience intense musculoskeletal pain.
- Nausea.
Common (may affect up to 1 in 10 people)
- Decrease in blood platelets, which increases the risk of bleeding or bruising.
- Headache.
- Skin reactions, such as redness or rash.
- Low potassium levels in the blood, which can cause muscle weakness, fasciculations, or heart rhythm disturbances.
- Chest pain.
- Blood-tinged cough.
Rare (may affect up to 1 in 100 people)
- Increased white blood cells.
- Local reactions at the injection site, such as pain or hardening.
- Some changes in the blood may occur, but they will be detected in routine blood tests.
- Pulmonary bleeding.
Frequency not known (frequency cannot be estimated from the available data)
- Inflammation of the aorta (the large blood vessel that carries blood from the heart to the rest of the body), see section 2.
Adverse effects observed with similar medicines, but not yet with Lonquex
- Sickle cell crisis in patients with sickle cell anemia.
- Painful, elevated, red-purple lesions on the limbs, and sometimes on the face and neck, accompanied by fever (Sweet's syndrome).
- Inflammation of the blood vessels in the skin.
- Damage to the small filters in the kidneys (glomerulonephritis; see section 2 under the heading "Warnings and precautions").
Reporting adverse effects
If you experience any adverse effects, consult your doctor, pharmacist, or nurse, even if they are possible adverse effects not listed in this leaflet. You can also report them directly through the national reporting system included in Appendix V. By reporting adverse effects, you can help provide more information on the safety of this medicine.
5. Storage of Lonquex
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiration date stated on the outer packaging and on the label of the pre-filled syringe after EXP. The expiration date is the last day of the month indicated.
Store in a refrigerator (between 2°C and 8°C).
Do not freeze.
Keep the pre-filled syringe in the outer packaging to protect it from light.
Do not use this medicine if you notice that it is cloudy or contains particles.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of the packaging and any unused medicine. This will help protect the environment.
6. Package contents and additional information
Composition of Lonquex
- The active substance is lipegfilgrastim. Each pre-filled syringe contains 6 mg of lipegfilgrastim.
Each milliliter of solution contains 10 mg of lipegfilgrastim.
- The other ingredients (excipients) are glacial acetic acid, sodium hydroxide (see section 2 "Lonquex contains sodium"), sorbitol (E420) (see section 2 "Lonquex contains sorbitol"), polysorbate 20, and water for injections.
Appearance of the product and package contents
Each pre-filled syringe contains 0.6 ml of solution.
Not all pack sizes may be marketed.
Marketing authorization holder
Teva B.V.
Swensweg 5
2031 GA Haarlem
Netherlands
Manufacturer
Teva Biotech GmbH
Dornierstraße 10
89079 Ulm
Germany
Merckle GmbH
Graf-Arco-Straße 3
89079 Ulm
Germany
Merckle GmbH Graf-Arco-Straße 3 89079 Ulm Germany |
You can obtain more information about this medicine by contacting the local representative of the marketing authorization holder:
België/Belgique/Belgien Teva Pharma Belgium N.V./S.A./AG Tel: +32 38207373 | Lietuva UAB Teva Baltics Tel: +370 52660203 |
| Luxembourg/Luxemburg Teva Pharma Belgium N.V./S.A./AG Belgique/Belgien Tel: +32 38207373 |
Ceská republika Teva Pharmaceuticals CR, s.r.o. Tel: +420 251007111 | Magyarország Teva Gyógyszergyár Zrt. Tel: +36 12886400 |
Danmark Teva Denmark A/S Tlf: +45 44985511 | Malta Teva Pharmaceuticals Ireland Ireland Tel: +44 2075407117 |
Deutschland TEVA GmbH Tel: +49 73140208 | Nederland Teva Nederland B.V. Tel: +31 8000228400 |
Eesti UAB Teva Baltics Eesti filiaal Tel: +372 6610801 | Norge Teva Norway AS Tlf: +47 66775590 |
Ελλάδα Specifar A.B.E.E. Τηλ: +30 2118805000 | Österreich ratiopharm Arzneimittel Vertriebs-GmbH Tel: +43 1970070 |
España Teva Pharma, S.L.U. Tel: +34 913873280 | Polska Teva Pharmaceuticals Polska Sp. z o.o. Tel: +48 223459300 |
France Teva Santé Tél: +33 155917800 | Portugal Teva Pharma - Produtos Farmacêuticos, Lda. Tel: +351 214767550 |
Hrvatska Pliva Hrvatska d.o.o. Tel: +385 13720000 | România Teva Pharmaceuticals S.R.L. Tel: +40 212306524 |
Ireland Teva Pharmaceuticals Ireland Tel: +44 2075407117 | Slovenija Pliva Ljubljana d.o.o. Tel: +386 15890390 |
Ísland Alvogen ehf. Sími: +354 5222900 | Slovenská republika TEVA Pharmaceuticals Slovakia s.r.o. Tel: +421 257267911 |
Italia Teva Italia S.r.l. Tel: +39 028917981 | Suomi/Finland Teva Finland Oy Puh/Tel: +358 201805900 |
Κύπρος Specifar A.B.E.E. Ελλάδα Τηλ: +30 2118805000 | Sverige Teva Sweden AB Tel: +46 42121100 |
Latvija UAB Teva Baltics filiale Latvija Tel: +371 67323666 | United Kingdom (Northern Ireland) Teva Pharmaceuticals Ireland Ireland Tel: +44 2075407117 |
Date of last revision of this leaflet: {month YYYY}
Detailed information on this medicine is available on the European Medicines Agency website: http://www.ema.europa.eu.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Lonquex 6mg injectable solutionDosage form: INJECTABLE, 6 mg/0.6 mLActive substance: lipegfilgrastimManufacturer: Teva B.V.Prescription requiredDosage form: INJECTABLE, 12 IU/0.2 mlActive substance: filgrastimManufacturer: Accord Healthcare S.L.U.Prescription requiredDosage form: INJECTABLE, 0.3 mg / prefilled syringeActive substance: filgrastimManufacturer: Accord Healthcare S.L.U.Prescription required
Online doctors for Lonquex 6mg injectable solution
Discuss questions about Lonquex 6mg injectable solution, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions