INSTANYL 200 micrograms/dose NASAL SPRAY SOLUTION


How to use INSTANYL 200 micrograms/dose NASAL SPRAY SOLUTION
Translated with AI
This page provides general information and does not replace a doctor’s consultation. Always consult a doctor before taking any medication. Seek urgent medical care if symptoms are severe.
Show originalContents of the leaflet
Introduction
Package Leaflet: Information for the User
Instanyl 50micrograms/dose nasal spray solution
Instanyl 100micrograms/dose nasal spray solution
Instanyl 200micrograms/dose nasal spray solution
fentanyl
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet, you may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, nurse or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- What is Instanyl and what is it used for.
- What you need to know before you use Instanyl
- How to use Instanyl
- Possible side effects
- Storing Instanyl
- Contents of the pack and other information
1. What is Instanyl and what is it used for
Instanyl contains the active substance fentanyl and belongs to a group of strong painkillers called opioids. Opioids work by blocking pain signals to the brain.
Instanyl acts quickly and is used to treat breakthrough pain in adult patients with cancer who are already taking opioid painkillers for their persistent pain. Breakthrough pain is a sudden pain that occurs even when you are taking your regular opioid painkillers.
2. What you need to know before you use Instanyl
Do not use Instanyl
- if you are allergic to fentanyl or any of the other ingredients of this medicine (listed in section 6);
- if you are not already using a prescribed opioid medicine every day for your persistent pain (e.g. codeine, fentanyl, hydromorphone, morphine, oxycodone, meperidine), as this may increase the risk of your breathing becoming slower and/or shallower, and even stopping;
- if you are taking a medicine that contains sodium oxybate;
- if you have short-term pain that is not breakthrough pain;
- if you have severe breathing difficulties or severe obstructive lung disease.
- if you have had previous radiotherapy to the head;
- if you have had repeated episodes of nosebleeds.
Warnings and precautions
Keep this medicine out of the sight and reach of children and in a safe place to prevent misuse. See section 5 for more information.
Talk to your doctor or pharmacist before starting Instanyl, especially:
- if you have chronic obstructive lung disease, Instanyl may affect your breathing rhythm.
- if you have heart problems, especially a slow heart rate, low blood pressure or low blood volume.
- if you have liver or kidney problems.
- if you have problems with your brain function, for example due to a brain tumour, head injury or increased pressure in the brain.
- if you have ever had adrenal insufficiency or a lack of sex hormones (androgen deficiency) when using opioids.
- if you are taking sedatives, such as benzodiazepines or related medicines (see also section “Using Instanyl with other medicines”).
- if you are taking antidepressants or antipsychotics (see also section “Using Instanyl with other medicines”).
- if you are taking medicines called partial agonist/antagonists, e.g. buprenorphine, nalbuphine and pentazocine (painkillers), as they may cause withdrawal symptoms. See section “Using Instanyl with other medicines” for more information.
- if you are using other nasal spray products, e.g. for the common cold or allergies.
Respiratory sleep disorders
Instanyl may cause respiratory sleep disorders, including sleep apnoea (pauses in breathing while sleeping) and sleep hypoxemia (low oxygen levels in the blood). Symptoms may include pauses in breathing while sleeping, waking up in the middle of the night due to lack of breath, difficulty staying asleep or excessive sleepiness during the day. If you or someone else notices these symptoms, contact your doctor to assess the possibility of reducing the dose.
It is very important that you contact your doctor or hospital immediately if you experience breathing difficulties while being treated with Instanyl.
Talk to your doctor if, while using Instanyl, you:
- feel pain or increased sensitivity to pain (hyperalgesia) that does not respond to a higher dose of the medicine as prescribed by your doctor.
- experience a combination of the following symptoms: nausea, vomiting, loss of appetite, fatigue, weakness, dizziness and low blood pressure. Together, these symptoms can be a sign of a potentially life-threatening condition called adrenal insufficiency, where the adrenal glands do not produce enough hormones.
If you experience repeated nosebleeds or notice nasal discomfort during treatment with Instanyl, you should talk to your doctor, who will assess alternative treatments for your breakthrough pain.
Long-term use and tolerance
This medicine contains fentanyl, an opioid. Repeated use of opioid painkillers can make the medicine less effective (your body gets used to it, which is known as pharmacological tolerance). You may also become more sensitive to pain when using Instanyl. This is known as hyperalgesia. Increasing the dose of Instanyl may continue to reduce pain for a while, but it can also be harmful. If you notice that the medicine is becoming less effective, talk to your doctor. Your doctor will decide whether it is better to increase the dose or gradually reduce the use of Instanyl.
Dependence and addiction
Repeated use of Instanyl can also lead to dependence, abuse and addiction, which can result in a potentially life-threatening overdose. The risk of these side effects may be greater with higher doses and longer use. Dependence or addiction can lead to a feeling of loss of control over the amount of medicine you use or how often you use it. You may feel the need to continue using the medicine even if it does not help relieve pain.
The risk of dependence or addiction varies from person to person. The risk of becoming dependent on or addicted to Instanyl may be greater if:
- you or a family member have abused alcohol, prescription medicines or illegal drugs (“addiction”).
- you smoke.
- you have ever had mood problems (depression, anxiety or personality disorder) or have been treated by a psychiatrist for other mental health problems.
If you notice any of the following symptoms while using Instanyl, it could be a sign of dependence or addiction.
- you need to use the medicine for longer than prescribed by your doctor.
- you need to use a higher dose than recommended.
- you are using the medicine for reasons other than those prescribed, e.g. “to feel calm” or “to help you sleep”.
- you have made repeated unsuccessful attempts to stop using the medicine or control its use.
- you feel unwell when you stop using the medicine (e.g. nausea, vomiting, diarrhoea, anxiety, shivering, shaking and sweating), and you feel better once you take it again (“withdrawal symptoms”).
If you notice any of these signs, talk to your doctor to determine the best treatment for you, when it is appropriate to stop the medicine and how to do it safely.
Children and adolescents
Instanyl should not be used in children and adolescents under 18 years.
Using Instanyl with other medicines
Tell your doctor or pharmacist if you are using, have recently used or might use any other medicines, including those obtained without a prescription.
Instanyl may affect or be affected by other medicines.
Special care should be taken if you are being treated with any of the following medicines:
- Other painkillers and medicines for nerve pain, such as gabapentin and pregabalin.
- any medicine that makes you sleepy (has a sedative effect) such as sleeping pills, sedatives (e.g. benzodiazepines or related medicines), medicines for anxiety, antihistamines or tranquillisers, muscle relaxants and gabapentinoids (gabapentin and pregabalin). Using these medicines at the same time as Instanyl may cause drowsiness, deep sedation and affect your ability to breathe (respiratory depression), which can lead to coma or even death. Therefore, concomitant use should only be considered when no other treatment options are available.
However, if your doctor prescribes Instanyl and sedatives, you should limit both the dose and duration of concomitant treatment.
Tell your doctor about all sedatives you are taking and follow their recommendations about the dose carefully. It may be helpful to inform your friends or family to be aware of the signs and symptoms mentioned above. Contact your doctor when you report such symptoms.
- any medicine that may change the way your body breaks down Instanyl, such as:
- ritonavir, nelfinavir, amprenavir, and fosamprenavir (medicines that help control HIV infections);
- CYP3A4 inhibitors, such as ketoconazole, itraconazole, or fluconazole (used to treat fungal infections);
- troleandomycin, clarithromycin, or erythromycin (medicines for treating bacterial infections);
- aprepitant (used to treat severe nausea);
- diltiazem and verapamil (medicines for treating high blood pressure or heart disease).
- medicines called Monoamine Oxidase Inhibitors (MAOIs), used for severe depression, even if you have been treated with one of these in the last 2 weeks.
- the risk of side effects increases if you are taking certain antidepressants or antipsychotics. Instanyl may interact with these medicines and you may experience changes in mental status (e.g. agitation, hallucinations, coma) and other effects such as body temperature above 38°C, increased heart rate, unstable blood pressure and exaggerated reflexes, muscle stiffness, lack of coordination and/or gastrointestinal symptoms (e.g. nausea, vomiting, diarrhoea). Your doctor will tell you if Instanyl is suitable for you.
- medicines called partial agonist/antagonists, e.g. buprenorphine, nalbuphine and pentazocine (painkillers). You may experience withdrawal symptoms (nausea, vomiting, diarrhoea, anxiety, shivering, shaking and sweating).
- other nasal sprays, especially oxymetazoline, xylometazoline and similar medicines, used for relieving nasal congestion.
Instanyl with food, drinks and alcohol
Do not drink alcohol while being treated with Instanyl, as it may increase the risk of serious side effects.
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before using any medicine.
Instanyl should not be used during pregnancy, unless you have discussed it with your doctor.
Instanyl should not be used during labour, as fentanyl can cause serious breathing problems in the newborn.
Fentanyl can pass into breast milk and cause side effects in the baby. Do not use Instanyl if you are breast-feeding. You should not start breast-feeding until 5 days after the last dose of Instanyl.
Driving and using machines
You should not drive or use machines while being treated with Instanyl. Instanyl can cause dizziness, drowsiness and blurred vision, which can affect your ability to drive or operate machinery.
3. How to use Instanyl
Before starting treatment and regularly during treatment, your doctor will also explain what you can expect from using Instanyl, when and for how long you should use it, when you should contact your doctor and when you should stop using it (see also section 2).
Follow the instructions for administration of this medicine exactly as your doctor has told you. If you are not sure, ask your doctor or pharmacist.
The dose of Instanyl is independent of your background treatment for cancer pain.
When you start using Instanyl, your doctor will determine with you the dose that relieves your breakthrough pain.
The initial dose is one spray of 50 micrograms into one nostril each time you have a breakthrough pain episode. During the dose titration phase, your doctor may instruct you to switch to a higher dose.
If the breakthrough pain is not relieved after 10 minutes, you can use only one more spray for this episode.
In general, you should wait 4 hours before treating another episode of breakthrough pain. In exceptional cases, when a new episode occurs before 4 hours, you can use Instanyl to treat this episode, but you should wait at least 2 hours before doing so. If you regularly experience episodes of breakthrough pain separated by less than 4 hours, contact your doctor, as your background treatment for cancer pain may need to be changed.
You can use Instanyl to treat a maximum of four episodes of breakthrough pain per day.
Contact your doctor if you experience more than four episodes of breakthrough pain per day, as your background treatment for cancer pain may need to be changed.
Do not change the dose of Instanyl or your other painkillers yourself. Changes to the dose should be made with your doctor.
Instanyl has a dose counter and a time lock-out period between doses to reduce the risk of overdose and help you use it correctly. The dose counter allows you and your doctor to monitor and adjust your use. After two doses have been taken within a 60-minute period, Instanyl will be locked for a period of 2 hours, starting from the first dose, until another dose can be dispensed.
Instanyl is for nasal use.
Read the instructions for use on the back of this leaflet to learn how to use the nasal spray.
If you use more Instanyl than you should or if you think someone has used Instanyl accidentally
If you have used more Instanyl than you should, contact your doctor, hospital or emergency service to assess the risk and advise on what to do.
The symptoms of overdose are:
Drowsiness, lethargy, dizziness, decreased body temperature, decreased heart rate, difficulty coordinating arms and legs.
In severe cases, symptoms of overdose with Instanyl can include coma, sedation, convulsions or severe breathing difficulties (very slow or shallow breathing). An overdose can also cause a brain disorder known as toxic leucoencephalopathy.
If you notice any of these symptoms, seek medical help immediately.
Note for caregivers:
If you notice that the person being treated with Instanyl suddenly becomes drowsy, has breathing difficulties or has difficulty staying awake:
- seek immediate emergency help.
- while waiting for help, try to keep the person awake by talking to them or gently shaking them from time to time.
- if the person has breathing difficulties, try to get them to breathe every 5-10 seconds.
- if the person stops breathing, try to resuscitate them until emergency help arrives.
If you think someone has used Instanyl accidentally, seek medical help immediately. Try to keep the person awake until the emergency service arrives.
If someone has used Instanyl accidentally, they may experience the same symptoms as described above in case of overdose.
If you forget to use Instanyl
If you continue to experience breakthrough pain, you can use Instanyl as prescribed by your doctor. If the breakthrough pain has stopped, do not use Instanyl until the next episode of breakthrough pain occurs.
If you stop using Instanyl
You should stop using Instanyl when you no longer experience breakthrough pain. However, you should continue using your background painkiller to treat your cancer pain. If you are in doubt, consult your doctor to confirm the correct dose of your regular painkiller.
You may experience sudden withdrawal symptoms similar to possible side effects of Instanyl if you stop using it. If you experience withdrawal symptoms, talk to your doctor. Your doctor will assess whether you need medicine to reduce or eliminate these symptoms.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible Adverse Effects
Like all medicines, this medicine can cause adverse effects, although not all people suffer from them.
Frequently, adverse effects will disappear or decrease with continued use of the medicine.
Interrupt treatment and contact your doctor, hospital, or emergency service immediately if:
- you experience a severe and sudden allergic reaction with difficulty breathing, inflammation, feeling of dizziness, increased heart rate, sweating, or loss of consciousness.
- you experience severe breathing difficulties.
- you have a whistling sound when inhaling.
- you have convulsive pain.
- you experience extreme dizziness.
These adverse effects can be very serious.
Other adverse effects observed after using Instanyl:
Frequent(may affect up to 1 in 10 people):
Drowsiness, dizziness even with difficulty maintaining balance, headache, throat irritation, nausea, vomiting, flushing, intense heat sensation, excessive sweating.
Infrequent(may affect up to 1 in 100 people):
Insomnia, lethargy, muscle convulsions, strange or unpleasant sensation in the skin, taste alteration, motion-induced dizziness, low blood pressure, severe respiratory problems, nasal bleeding, nasal ulcer, runny nose, constipation, mouth inflammation, dry mouth, skin discomfort, skin itching, fever.
Unknown(frequency cannot be estimated from available data):
Allergic reaction, falls, diarrhea, seizures (epileptic crisis), loss of consciousness, inflammation of arms or legs, seeing or hearing things that are not real (hallucinations), delirium (symptoms may include a combination of agitation, restlessness, disorientation, confusion, fear, seeing or hearing things that do not really exist, sleep disorders, nightmares), pharmacological tolerance, drug dependence (addiction), drug abuse (see section 2), fatigue, general malaise, withdrawal syndrome (which can manifest with the appearance of the following adverse effects: nausea, vomiting, diarrhea, anxiety, chills, tremors, and sweating), breathing difficulties.
Cases have also been observed of patients who have developed a perforation in the nasal septum – the structure that separates the nostrils.
You should inform your doctor if you suffer from repeated episodes of nasal bleeding or nose discomfort.
Prolonged treatment with fentanyl during pregnancy can cause withdrawal symptoms in the newborn, which can be potentially fatal (see section 2).
Reporting of Adverse Effects
If you experience any type of adverse effect, consult your doctor or pharmacist, even if it is a possible adverse effect not listed in this prospectus. You can also report them directly through the Spanish System of Pharmacovigilance of Medicines for Human Use: https://www.notificaRAM.es. By reporting adverse effects, you can contribute to providing more information on the safety of this medicine.
5. Conservation of Instanyl
The analgesic contained in Instanyl is very potent and can be fatal in children. Instanyl must be kept out of sight and reach of children. The child-resistant safety cap on the nasal spray must always be replaced after each use.
Keep this medicine in a safe and protected place, inaccessible to other people. This medicine can cause serious harm and even be fatal for people who use it accidentally or intentionally when not prescribed to them.
Do not use Instanyl after the expiration date stated on the packaging after CAD or EXP. The expiration date is the last day of the indicated month.
Store below 30°C. Keep the nasal spray in a vertical position. Do not freeze. If the Instanyl nasal spray freezes, the device may break. You should check the spray button before use if you are unsure how it has been stored.
Instanyl packages that have exceeded the expiration date or are no longer to be used may still contain enough medication to harm other people, especially children.
| This device is labeled in accordance with the Directive on Waste Electrical and Electronic Equipment (WEEE). Medicines should not be thrown away through drains or into the trash. Any used or unused nasal spray must be returned to the pharmacy or disposed of according to local regulations, or returned to the pharmacy. Ask your pharmacist how to dispose of packages and medicines that are no longer needed. This will help protect the environment. This will help protect the environment. |
6. Package Contents and Additional Information
Composition of Instanyl
The active ingredient is fentanyl citrate. The content is:
50 micrograms/dose: 1 ml contains fentanyl citrate equivalent to 500 micrograms of fentanil. A spray (100 microliters) contains 50 micrograms of fentanyl.
100 micrograms/dose: 1 ml contains fentanyl citrate equivalent to 1,000 micrograms of fentanyl. A spray (100 microliters) contains 100 micrograms of fentanyl.
200 micrograms/dose: 1 ml contains fentanyl citrate equivalent to 2,000 micrograms. A spray (100 microliters) contains 200 micrograms of fentanyl.
The other components are sodium dihydrogen phosphate dihydrate, disodium phosphate dihydrate, and purified water.
Appearance of Instanyl and Package Contents
Instanyl DoseGuard is a nasal spray solution. The solution is transparent and colorless. It contains a nasal spray with a dosing pump, an electronic indicator, a dose counter, an integrated lock mechanism, and a child-resistant safety cap.
The nasal spray comes in three different sizes: 3.2 ml (equivalent to 20 doses), 4.3 ml (equivalent to 30 doses), and 5.3 ml (equivalent to 40 doses).
Only some package sizes may be marketed.
The labeling of the three Instanyl concentrations is differentiated by color:
For 50 micrograms/dose, the labeling is orange.
For 100 micrograms/dose, the labeling is purple.
For 200 micrograms/dose, the labeling is greenish-blue.
Marketing Authorization Holder
Istituto Gentili S.r.l.
Via San Giuseppe Cottolengo 15
20143 Milano
Italy
Manufacturer
Curida AS
Solbærvegen 5
NO-2409 Elverum
Norway
Date of Last Revision of this Leaflet
August 2024
Detailed information on this medicinal product is available on the European Medicines Agency website http://www.ema.europa.eu.
INSTRUCTIONS FOR USE OF INSTANYL
Read the following instructions carefully to learn how to use the Instanyl nasal spray.
Important Information Before Use:
- Do not modify the medical device.
- Do not allow liquids to enter the medical device.
The Instanyl nasal spray includes:
- An integrated lock function that controls how often the nasal spray can be used
- A child-resistant safety cap, which must be placed when the nasal spray is not in use
- An electronic indicator that
- shows how many times the nasal spray needs to be pressed (prepared) before using the product
- shows the number of doses remaining
- shows if the nasal spray is blocked or ready to be used
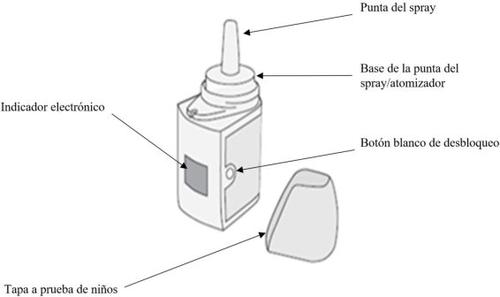
How to Remove and Replace the Child-Resistant Safety Cap
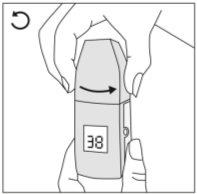
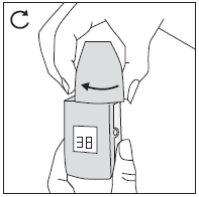
| Remove the child-resistant cap by pressing on both sides and then twisting it counterclockwise to lift it off. To replace it, place the safety cap over the tip of the nasal spray and twist it clockwise. When you hear a click, the child-resistant cap will be in place. Always replace the cap over the nasal spray after use. |
Preparing the Instanyl Nasal Spray
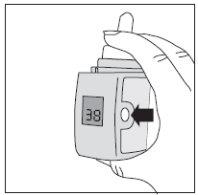
| Before using the nasal spray for the first time, you must prime it until the indicator shows the number of doses. The instructions for preparing the medical device are included below (“Priming Steps”). Note: To press the spray, place two fingers on either side of the base of the spray tip and your thumb underneath the device. Then, squeeze. Warning: During this priming process, some of the medication will be expelled. Consequently:
Priming Steps:
The nasal spray is now ready for use. Note: Depending on your prescription, the initial number will be 20, 30, or 40. |
Re-Priming the Instanyl Nasal Spray (after 7 days or more) | |
| If you have not used Instanyl for 7 days or more, you must re-prime the nasal spray by pressing it again until the next dose is taken. This will be indicated by a letter “P” on the indicator. |
| Steps to Re-Prime the Nasal Spray:
|
|
|
|
Warning: During this priming process, some of the medication will be expelled. Consequently:
|
|
|
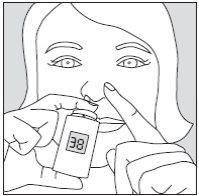
How to Use the Instanyl Nasal Spray
The nasal spray can only be used when the lock symbol does not appear on the indicator. | |
|
Note: You will hear a “click” sound when the atomizer is pressed and the nasal spray has dispensed its dose.
Remember to press and release the white button on the side of the nasal spray before spraying it. Remember to always place the child-resistant safety cap on the nasal spray and close it after each use. Remember to keep the nasal spray upright at all times. |
| The nasal spray allows up to two doses for each episode of pain. After the second dose, which can be administered 10 minutes after the first, the nasal spray will be blocked. The lock or block symbol will appear on the indicator, along with a clock symbol showing a countdown, indicating the time remaining before the nasal spray can be used again (each black mark equals 10 minutes). When this time period has passed, the lock or block symbol will start flashing. Then the nasal spray will be ready for use when the next episode of pain occurs. You must wait 4 hours before treating the next episode of pain. You can use Instanyl to treat up to 4 episodes of pain per day. If you experience more than 4 episodes of pain per day, you should contact your doctor, as your pain treatment may need to be revised. When the nasal spray is empty, the indicator will show “0” and the lock symbol will appear. Disposal Do not dispose of the Instanyl nasal spray down the drain or with household waste. Any used or unused nasal spray must be returned to the pharmacy or disposed of according to local regulations. Consult your pharmacist for guidance on how to dispose of the medication. |
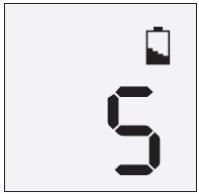
| Low Battery Level If the indicator shows a battery symbol, this means that the battery charge is about to run out. The number of doses shown on the indicator will change to “5”. This is the approximate number of doses that the nasal spray can dispense before the battery is too low and the indicator turns off. If the battery symbol appears on the indicator, it is recommended that the patient contact their doctor or pharmacist to obtain a new nasal spray. |
Explanation of the Symbols Shown on the Electronic Indicator | |
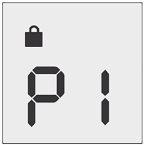
| The nasal spray must be pumped 5 times (primed) before it can be used (see the section “Preparing the Instanyl Nasal Spray”). The indicator shows a value that decreases (P5, P4, P3, P2, and P1) after each actuation. The nasal spray is ready when the indicator shows the number of doses (i.e., 20, 30, or 40). When priming, the above safety warning instructions must be taken into account (see the section “Priming Steps”). |
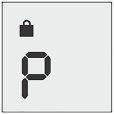
| The nasal spray has not been used for 7 days or more and must be re-primed by pressing it once into the air in a well-ventilated area before use (see the information below). The “P” symbol will disappear from the indicator when the nasal spray is re-primed by actuating it once. When re-priming, the above safety warning instructions must be taken into account (see the section “Steps to Re-Prime the Nasal Spray”). |
| LOCK SYMBOL The nasal spray is blocked and cannot be used. When the lock period ends, the lock symbol will start flashing. The lock symbol will disappear from the indicator when the white button on the side of the nasal spray is pressed. At that time, the nasal spray can be used again when the next episode of pain occurs. |
| CLOCK SYMBOL WITH COUNTDOWN Shows how much time is left on the lock period. The countdown clock shows a descending countdown. Each black mark equals 10 minutes: the maximum lock period is 2 hours. The CLOCK SYMBOL WITH COUNTDOWN is shown along with the LOCK SYMBOL. It is recommended to wait 4 hours before treating the next episode of pain. |
| Shows the number of doses remaining in the nasal spray. After each dose, this number decreases on the indicator. Depending on the model, the initial number may be 20, 30, or 40. |
| BATTERY SYMBOL The battery charge is about to run out. The number of doses shown on the indicator changes to 5. This is the approximate number of doses that the nasal spray can dispense before the battery level is too low and the indicator turns off. The battery cannot be recharged, and the user should contact their doctor or pharmacist to obtain a new nasal spray. |
If you notice that the nasal indicator is not working as described in the “Instructions for Use”, you should contact your doctor or pharmacist.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- This information is for reference only and does not constitute medical advice. Always consult a doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to INSTANYL 200 micrograms/dose NASAL SPRAY SOLUTIONDosage form: TRANSDERMAL PATCH, 12 MCG/HActive substance: fentanylManufacturer: Aristo Pharma Iberia S.L.Prescription requiredDosage form: BUCCAL/SUCKING TABLET, 1200 microgramsActive substance: fentanylManufacturer: Ferrer Internacional S.A.Prescription requiredDosage form: BUCCAL/SUCKING TABLET, 1600 microgramsActive substance: fentanylManufacturer: Ferrer Internacional S.A.Prescription required
Online doctors for INSTANYL 200 micrograms/dose NASAL SPRAY SOLUTION
Discuss questions about INSTANYL 200 micrograms/dose NASAL SPRAY SOLUTION, including use, safety considerations and prescription review, subject to medical assessment and local regulations.
Frequently Asked Questions