

Xeomin

Ask a doctor about a prescription for Xeomin

How to use Xeomin
Leaflet attached to the packaging: Information for the user
XEOMIN, 50 units, powder for solution for injection
XEOMIN, 100 units, powder for solution for injection
XEOMIN, 200 units, powder for solution for injection
The neurotoxin Clostridium botulinumtype A (150 kD), free from complexing proteins
You should carefully read the contents of the leaflet before receiving the medicine, as it contains important information for the patient.
- You should keep this leaflet, so that you can read it again if you need to.
- If you have any doubts, you should consult a doctor or pharmacist.
- If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet:
- 1. What is XEOMIN and what is it used for
- 2. Important information before using XEOMIN
- 3. How to use XEOMIN
- 4. Possible side effects
- 5. How to store XEOMIN
- 6. Contents of the pack and other information
1. What is XEOMIN and what is it used for
XEOMIN is a medicine that contains the active substance botulinum neurotoxin type A, which, depending on the site of administration, relaxes muscles or reduces saliva production.
XEOMIN is used to treat the following conditions in adults:
- eyelid spasm (blepharospasm) and facial spasm (hemifacial spasm),
- cervical dystonia (spasmodic torticollis),
- increased muscle tone/uncontrolled stiffness of the arms, hands, and/or fingers (upper limb spasticity),
- chronic drooling (sialorrhea) due to neurological disorders.
XEOMIN is used to treat the following condition in children and adolescents from 2 to 17 years of age, with a body weight of ≥ 12 kg:
- chronic drooling (sialorrhea) due to neurological and/or neurodevelopmental disorders.
2. Important information before using XEOMIN
When not to use XEOMIN
- if the patient is allergic to botulinum neurotoxin type A or any of the other ingredients of this medicine (listed in section 6),
- if the patient has a generalized muscle disorder (e.g., myasthenia gravis, Lambert-Eaton syndrome),
- if the patient has an infection or inflammation at the planned injection site.
Warnings and precautions
Side effects may be the result of injecting botulinum neurotoxin type A into the wrong place, resulting in temporary paralysis of nearby muscle groups. Very rarely, side effects have been reported that occur in connection with the spread of the toxin to distant sites from the injection site, causing symptoms consistent with the action of botulinum toxin type A (e.g., excessive muscle weakness, swallowing disorders, and/or accidental choking on food or drinks). Patients receiving recommended doses may experience excessive muscle weakness.
If the dose is too high or the medicine is given too frequently, the risk of antibody formation may increase. Antibody formation can result in treatment failure with botulinum toxin type A, regardless of the reason for administration.
Before starting treatment with XEOMIN, you should discuss the following with your doctor or pharmacist:
- if the patient has a bleeding disorder,
- if the patient is taking substances that prevent blood clotting (e.g., coumarin, heparin, acetylsalicylic acid, clopidogrel),
- if the patient has significant weakness or muscle wasting in the muscle to be injected,
- if the patient has amyotrophic lateral sclerosis (ALS), which can lead to generalized muscle atrophy,
- if the patient has any disease that disrupts the interaction between nerves and skeletal muscles (neuromuscular disorder),
- if the patient has had swallowing difficulties,
- if the patient has had seizures,
- if the patient has had problems with botulinum toxin type A injections in the past,
- if the patient is scheduled for surgery.
You should contact your doctor or seek medical attention if you experience any of the following symptoms:
- difficulty breathing, swallowing, or speaking,
- hives, swelling, including swelling of the face or throat, wheezing, feeling of weakness, and shortness of breath (possible severe allergic reaction symptoms).
Repeated injections of XEOMIN
In cases of repeated XEOMIN injections, the efficacy of the medicine may increase or decrease. Possible causes include:
- different solution preparation procedures by the doctor,
- different lengths of treatment breaks,
- injections into a different muscle,
- marginal change in the efficacy of the active substance of XEOMIN,
- lack of response to the treatment applied. Blepharospasm (eyelid spasm) andhemifacial spasm (facial spasm)You should consult your doctor before using XEOMIN if:
- the patient has had eye surgery. The doctor will take additional precautions,
- the patient is at risk of developing a condition called narrow-angle glaucoma. This condition can cause increased intraocular pressure, which can lead to optic nerve damage. The doctor should be aware if the patient is at risk.
During treatment, minor bleeding into the soft tissues of the eyelid may occur. The doctor may reduce the risk of this by gently pressing the injection site immediately after administration.
After injecting XEOMIN into the eye muscle, the frequency of blinking may be reduced, which can lead to prolonged exposure of the transparent front part of the eye (cornea).
This exposure can lead to damage to its surface and inflammation (corneal ulcer).
Cervical dystonia (spasmodic torticollis)
After injection, the patient may experience swallowing difficulties, ranging from mild to severe. This can lead to breathing problems and a higher risk of choking on foreign substances or fluids. Foreign substances in the lungs can cause inflammation or infection (pneumonia). The doctor will provide special treatment if necessary (e.g., artificial feeding).
Swallowing difficulties may last up to two or three weeks after injection, and in one case, they were reported to last up to five months.
If the patient has not been active for a long time, their activity should start gradually after XEOMIN injection.
Increased muscle tone/uncontrolled stiffness of the arms, hands, and/or fingers (upper limb spasticity)
XEOMIN may be used to treat increased muscle tone/uncontrolled stiffness that occurs in various parts of the upper limb, such as the arm or hand.
XEOMIN is effective in combination with standard treatment methods.
XEOMIN should be used with these other methods.
It is unlikely that this medicine will improve the range of motion in joints if the surrounding muscles have lost their ability to stretch.
If the patient has not been active for a long time, their activity should start gradually after XEOMIN injection.
Chronic drooling (sialorrhea)
Some medicines (e.g., clozapine, aripiprazole, pyridostigmine) may cause excessive saliva production. It is recommended to consider replacing, reducing, or even stopping the treatment with the medicine that causes drooling before using XEOMIN to treat drooling.
The efficacy and safety of using XEOMIN in patients with drooling caused by medicines have not been studied.
If dry mouth occurs in connection with the use of XEOMIN, the doctor will consider reducing the dose.
As a result of the reduced amount of saliva produced after using XEOMIN, health problems in the mouth may occur, such as tooth decay or worsening of existing problems.
Before starting treatment with XEOMIN for chronic drooling, you should consult a dentist. The dentist may decide to use measures to prevent tooth decay if necessary.
Children and adolescents
This medicine should not be used in children under 2 years of age, in children with a body weight of less than 12 kg, or in children and adolescents for the treatment of conditions other than chronic drooling, as the use of XEOMIN has not been studied in these patient groups. Therefore, its use is not recommended in these patients.
XEOMIN and other medicines
You should tell your doctor or pharmacist about all medicines that the patient is currently taking or has recently taken, as well as any medicines that the patient plans to take.
The effect of XEOMIN may be increased:
- by medicines used to treat certain infectious diseases (e.g., spectinomycin or aminoglycoside antibiotics [e.g., neomycin, kanamycin, tobramycin]),
- by other medicines that relax muscles (e.g., muscle relaxants from the tubocurarine group). This type of medicine is used, among other things, in general anesthesia. Before surgery, you should inform the anesthesiologist that you have taken XEOMIN.
- in the case of chronic drooling treatment: by other medicines that reduce saliva production (e.g., anticholinergic medicines, such as atropine, glycopyrronium, or scopolamine) or as a result of radiation therapy to the head and neck, including the salivary glands. You should inform your doctor if you are or will be undergoing radiation therapy.
In such cases, the use of XEOMIN requires special caution.
The effect of XEOMIN may be reduced by:
- certain antimalarial and anti-rheumatic medicines (known as aminochinolines).
Pregnancy, breastfeeding, and fertility
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a child, they should consult their doctor or pharmacist before using this medicine.
XEOMIN should not be used during pregnancy, unless the doctor decides that it is absolutely necessary and that the expected benefit of using it outweighs the potential risk to the fetus.
XEOMIN is not recommended for use in breastfeeding women.
Driving and using machines
You should not drive or perform other potentially hazardous activities if you experience drooping eyelids, weakness (asthenia), muscle weakness, dizziness, or vision disturbances. In case of doubt, you should consult your doctor.
3. How to use XEOMIN
XEOMIN can only be administered by doctors with the appropriate specialized knowledge in the use of botulinum neurotoxin type A.
The optimal dose, frequency of administration, and number of injection sites will be determined by the doctor individually for the patient. The effect of the initial XEOMIN treatment should be evaluated, which may lead to dose adjustment until the desired effect of the medicine is achieved. The intervals between treatments will be determined by the doctor based on the individual needs of the patient.
If the patient feels that the effect of XEOMIN is too strong or too weak, they should contact their doctor. If no effect is visible, alternative treatment should be considered.
Blepharospasm (eyelid spasm)and hemifacial spasm (facial spasm)
The recommended initial dose is up to 25 units per eye, and the recommended total dose per treatment session is up to 50 units per eye. The onset of action of the medicine is usually observed within four days after injection. The effect of the medicine lasts for approximately 3-5 months after each treatment, but it may last significantly longer or shorter. The interval between treatment sessions should not be less than 12 weeks.
Using the medicine more frequently than every three months does not provide additional benefits.
If the patient has hemifacial spasm, the doctor will follow the recommendations for treating blepharospasm limited to one side of the face. The treatment of hemifacial spasm will concern the upper part of the face, as injecting XEOMIN into the lower part of the face may lead to an increased risk of side effects, such as significant local muscle weakness.
Cervical dystonia (spasmodic torticollis)
The recommended dose per injection site is up to 50 units, and the recommended maximum dose per first treatment session is up to 200 units. The doctor may use doses of up to 300 units in subsequent treatment sessions, depending on the response to treatment. The onset of action of the medicine is usually observed within seven days after injection. The effect of the medicine lasts for approximately 3-4 months after each treatment, but it may last significantly longer or shorter. Treatment can be repeated no earlier than 10 weeks.
Increased muscle tone/uncontrolled stiffness of the arms, hands, and/or fingers (upper limb spasticity)
The recommended dose is up to 500 units per treatment session. No more than 250 units should be administered to the arm muscles. Patients reported that they felt the onset of action within four days after administration. They experienced a reduction in muscle tone within four weeks. In general, the treatment effect lasted for 12 weeks, but it may last significantly longer or shorter. The interval between treatment sessions should be at least 12 weeks.
Chronic drooling (sialorrhea, adults)
The recommended dose is up to 100 units per treatment session. The recommended dose should not be exceeded. The interval between treatment sessions should be at least 16 weeks.
Chronic drooling (sialorrhea, children/adolescents)
The recommended dose per treatment session depends on body weight. The maximum dose should not be exceeded, which is 75 units. The interval between treatment sessions should be at least 16 weeks.
Method of administration
XEOMIN in the form of a solution is used for intramuscular injections (intramuscular administration) or for injection into the gland (into the salivary gland) (see information intended for healthcare professionals at the end of this leaflet). In adults, the appropriate salivary glands can be located using anatomical landmarks or ultrasound examination; however, for safety reasons, the ultrasound method is preferred. In children and adolescents, the ultrasound method should be used.
Before injection, children and adolescents may be given a local anesthetic (e.g., topical anesthetic cream), a sedative, or a sedative in combination with an anesthetic.
Using a higher dose of XEOMIN than recommended
Symptoms of overdose
Symptoms of overdose do not occur immediately after injection and may include general weakness, drooping eyelids, double vision, breathing difficulties, speech disorders, and paralysis of the respiratory muscles or swallowing difficulties, which can lead to pneumonia.
Procedure in case of overdose
If symptoms of overdose occur, the patient or someone from their environment should immediately call for emergency assistance; hospitalization may be required. Medical care and respiratory support may be necessary for several days.
In case of any further doubts related to the use of this medicine, you should consult a doctor, pharmacist, or nurse.
4. Possible side effects
Like all medicines, XEOMIN can cause side effects, although not everybody gets them.
Usually, side effects occur within the first week after treatment and are temporary. Side effects may be related to the medicine, the injection procedure, or both. Side effects may be limited to the area around the injection site (e.g., local muscle weakness, local pain, inflammation, tingling sensation [paresthesia], reduced sensation [hypoesthesia], increased sensitivity to touch, swelling [edema], soft tissue swelling [edema], redness of the skin [erythema], itching, local infection, hematoma, bleeding, and/or bruising).
Injection of the medicine may cause pain. Pain or fear of injection can lead to fainting, nausea, ringing in the ears (tinnitus), or low blood pressure.
Side effects, such as excessive muscle weakness or swallowing difficulties, may be caused by a decrease in muscle tone distant from the XEOMIN injection site.
Swallowing difficulties may cause aspiration of foreign substances into the respiratory system, resulting in pneumonia, which can be life-threatening.
XEOMIN may cause an allergic reaction. Rarely, severe and/or sudden allergic reactions (anaphylactic shock) or allergic reactions to the serum present in the medicine (serum sickness) have been reported, causing, for example, breathing difficulties (dyspnea), hives (urticaria), or soft tissue swelling (edema). Some of these reactions have been observed after the use of conventional botulinum toxin type A complex. They occurred when the toxin was administered alone or in combination with other medicines that cause similar reactions. An allergic reaction may cause the following symptoms:
- breathing, swallowing, or speech difficulties due to swelling of the face, lips, mouth, or throat,
- swelling of the hands, feet, or ankles.
In case of any of the above symptoms, you should immediately inform your doctor or seek help from your loved ones and go to the emergency room of the nearest hospital.
During the use of XEOMIN, the following side effects have been observed.
Blepharospasm (eyelid spasm)
Very common (may occur in more than 1 in 10 patients):
drooping eyelids
Common (may occur in up to 1 in 10 patients):
dry eye syndrome, blurred vision, vision disturbances, dry mouth, pain at the injection site
Uncommon (may occur in up to 1 in 100 patients):
headache, facial muscle weakness (facial nerve palsy), double vision, increased tearing, swallowing difficulties (dysphagia), fatigue, muscle weakness, rash
Hemifacial spasm (facial spasm)
During the treatment of hemifacial spasm, you can expect the same side effects as in blepharospasm.
Cervical dystonia (spasmodic torticollis)
Very common (may occur in more than 1 in 10 patients):
swallowing difficulties (dysphagia)
Common (may occur in up to 1 in 10 patients):
neck pain, muscle weakness, muscle pain, stiffness and muscle spasms, headache, dizziness, pain at the injection site, weakness (asthenia), dry mouth, nausea, increased sweating, upper respiratory tract infections, weakness (pre-syncope)
Uncommon (may occur in up to 1 in 100 patients):
speech disorders (dysphonia), shortness of breath (dyspnea), rash
Treatment of spasmodic torticollis may cause swallowing difficulties of varying severity.
This can lead to the entry of foreign substances into the lungs, which may require medical intervention.
Swallowing difficulties may last for two to three weeks after injection, but one case of lasting up to five months has been reported. The occurrence of swallowing difficulties seems to be dose-dependent.
Increased muscle tone/uncontrolled stiffness of the arms, hands, and/or fingers (upper limb spasticity)
Common (may occur in up to 1 in 10 patients):
dry mouth
Uncommon (may occur in up to 1 in 100 patients):
headache, reduced sensation (hypoesthesia), muscle weakness, limb pain, general weakness (asthenia), muscle pain, swallowing difficulties (dysphagia), nausea
Frequency not known (frequency cannot be estimated from the available data):
pain at the injection site
Chronic drooling (sialorrhea, adults)
Common (may occur in up to 1 in 10 patients):
dry mouth, swallowing difficulties (dysphagia), tingling sensation (paresthesia)
Uncommon (may occur in up to 1 in 100 patients):
thickened saliva, speech disorders, taste disturbances
Severe and persistent dry mouth (lasting more than 110 days) has been reported, which can lead to further complications, such as gum inflammation, swallowing difficulties, and tooth decay.
Chronic drooling (sialorrhea, children/adolescents)
Uncommon (may occur in up to 1 in 100 patients):
swallowing difficulties (dysphagia)
Frequency not known (frequency cannot be estimated from the available data):
dry mouth, thickened saliva, mouth pain, tooth decay
Post-marketing experience
After the medicine was placed on the market, the following side effects have been observed during the use of XEOMIN, with an unknown frequency of occurrence, regardless of the treated area: flu-like symptoms, reduction of muscle mass after injection, and hypersensitivity reactions, such as swelling, soft tissue swelling (edema, including edema in areas distant from the injection site), redness, itching, rash (local and generalized), and shortness of breath.
Reporting side effects
If you experience any side effects, including any side effects not listed in this leaflet, you should tell your doctor or pharmacist. Side effects can be reported directly to the Department of Adverse Reaction Monitoring of Medicinal Products, Medical Devices, and Biocidal Products
Al. Jerozolimskie 181C
- 02 - 222 Warsaw Tel.: + 48 22 49 21 301 Fax: + 48 22 49 21 309 Website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
Reporting side effects allows for the collection of more information on the safety of the medicine.
5. How to store XEOMIN
The medicine should be stored out of sight and reach of children.
Do not use this medicine after the expiry date stated on the carton and label of the vial after "EXP". The expiry date refers to the last day of that month.
The abbreviation "Lot" on the packaging means batch number.
Unopened vial: Do not store above 25°C.
Reconstituted solution: Chemical and physical stability of the solution has been demonstrated for 24 hours at a temperature of 2°C to 8°C.
From a microbiological point of view, the medicine should be used immediately. If it is not used immediately, the user is responsible for the storage conditions and the storage time before reuse, which should not exceed 24 hours at a temperature of 2°C to 8°C, unless reconstitution was performed under controlled aseptic conditions.
The doctor should not use XEOMIN if the solution is cloudy or contains undissolved medicine residues.
To learn about the disposal instructions, you should look for information in the section intended for healthcare professionals at the end of this leaflet.
6. Contents of the pack and other information
What XEOMIN contains
- The active substance of XEOMIN is Clostridium botulinumtype A neurotoxin (150 kD), free from complexing proteins. XEOMIN, 50 units, powder for solution for injectionOne vial contains 50 units of Clostridium botulinumtype A neurotoxin (150 kD), free from complexing proteins*. XEOMIN, 100 units, powder for solution for injectionOne vial contains 100 units of Clostridium botulinumtype A neurotoxin (150 kD), free from complexing proteins*. XEOMIN, 200 units, powder for solution for injectionOne vial contains 200 units of Clostridium botulinumtype A neurotoxin (150 kD), free from complexing proteins*. * Botulinum neurotoxin type A, purified from cultures of Clostridium botulinum bacteria(Hall strain).
- The other ingredients of the medicine are: human albumin, sucrose.
What XEOMIN looks like and contents of the pack
XEOMIN is a powder for solution for injection. The powder is white.
After reconstitution, the solution is clear and colorless.
XEOMIN, 50 units, powder for solution for injection:
Pack sizes: 1, 2, 3, or 6 vials.
XEOMIN, 100 units, powder for solution for injection:
Pack sizes: 1, 2, 3, 4, or 6 vials.
XEOMIN, 200 units, powder for solution for injection:
Pack sizes: 1, 2, 3, 4, or 6 vials.
Not all pack sizes may be marketed.
Marketing authorization holder
Merz Pharmaceuticals GmbH
Eckenheimer Landstrasse 100
60318 Frankfurt/Main
Germany
Tel: +49-69/1503-1
Fax: +49-69/1503-200
Manufacturer
Merz Pharma GmbH & Co. KGaA
Eckenheimer Landstrasse 100
60318 Frankfurt/Main
Germany
Tel: +49-69/1503-1
Fax: +49-69/1503-200
This medicinal product is authorized in the Member States of the European Economic Area under the following names:
XEOMIN: Austria, Bulgaria, Cyprus, Croatia, Czech Republic, Denmark, Estonia, Germany, Greece, Finland, France, Hungary, Ireland, Iceland, Italy, Latvia, Liechtenstein, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden
XEOMEEN: Belgium
Date of last revision of the leaflet: 22.04.2024
Information intended for healthcare professionals only: Instructions for preparing the solution for injection:
XEOMIN is reconstituted before administration using 9 mg/ml (0.9%) sodium chloride solution for injection.
XEOMIN can only be used for the treatment of one patient per treatment session.
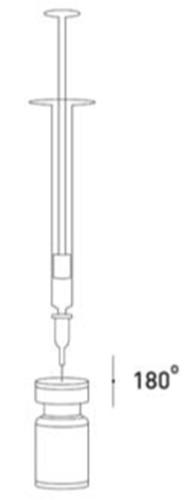
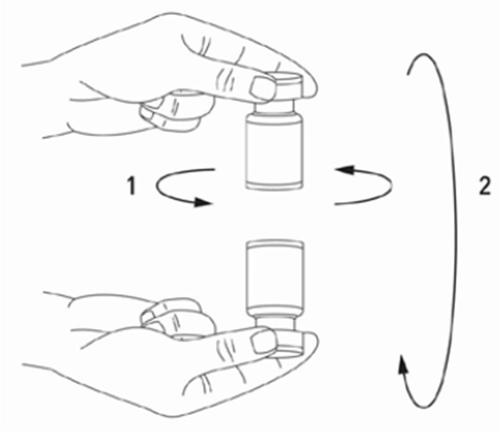
It is good practice to prepare the solution and prepare the syringe over a paper towel covered with foil in case of medicine spillage. The syringe should be filled with the appropriate amount of sodium chloride solution (see the table of dilutions). To prepare the solution, it is recommended to use a short-cut 20-27 G needle. The needle, at a right angle, should puncture the rubber stopper, after which the solvent will be slowly drawn into the vial by vacuum. The vial should be discarded if the solvent is not drawn into the vial by vacuum. The syringe should be disconnected from the vial and the XEOMIN mixed with the solvent by gently swirling the vial and rotating it/tapping it - without making sudden movements. If necessary, the needle used to prepare the solution should remain in the vial, and the appropriate amount of solution should be drawn up using a new, sterile syringe suitable for injecting the medicine.
After reconstitution, XEOMIN is a clear, colorless solution.
XEOMIN should not be used if the reconstituted solution (prepared as described above) is cloudy or contains undissolved medicine residues.
Efforts should be made to use the correct volume of solvent required to prepare the desired dose, to avoid accidental overdose. If different types of XEOMIN vials are used during one injection procedure, caution should be exercised to use the appropriate amount of solvent required to achieve the specific number of units per 0.1 ml. The amount of solvent is different for XEOMIN 50 units, XEOMIN 100 units, and XEOMIN 200 units. Each syringe should also be properly labeled.
Possible concentrations for XEOMIN 50, 100, and 200 units are shown in the following table:

| Obtained dose (units per 0.1 ml) | Added solvent (9 mg/ml (0.9%) sodium chloride solution for injection) | ||
| Vial containing 50 units | Vial containing 100 units | Vial containing 200 units | |
| 20 units | 0.25 ml | 0.5 ml | 1 ml |
| 10 units | 0.5 ml | 1 ml | 2 ml |
| 8 units | 0.625 ml | 1.25 ml | 2.5 ml |
| 5 units | 1 ml | 2 ml | 4 ml |
| 4 units | 1.25 ml | 2.5 ml | 5 ml |
| 2.5 units | 2 ml | 4 ml | not applicable |
| 2 units | 2.5 ml | 5 ml | not applicable |
| 1.25 units | 4 ml | not applicable | not applicable |
Disposal instructions
Solution for injection stored for more than 24 hours and unused solution for injection should be discarded.
Procedures for the safe disposal of vials, syringes, and used materials
Unused vials, reconstituted solution residues, and/or syringes should be subjected to steam sterilization. Alternatively, any remaining XEOMIN can be inactivated by adding one of the following solutions: 70% ethanol, 50% isopropanol, 0.1% SDS (anionic detergent), diluted sodium hydroxide (0.1 N NaOH), or diluted sodium hypochlorite solution (at least 0.1% NaOCl).
After inactivation, the used vials, syringes, and materials should not be emptied but should be placed in appropriate containers and disposed of in accordance with local regulations.
Recommendations for procedures in case of unforeseen incidents during the administration of botulinum toxin type A
- Any spillage of the medicine should be removed immediately: in the case of powder using an absorbent material soaked in one of the above solutions, or in the case of the reconstituted medicine using a dry absorbent material.
- The contaminated surface should be wiped with an absorbent material soaked in one of the above solutions and then dried.
- If the vial is broken, proceed according to the above instructions. Carefully collect the broken glass fragments, avoiding cuts.
- If the medicine comes into contact with the skin, the area of contact should be rinsed with a large amount of water.
- In case of eye contact, the eyes should be thoroughly rinsed with a large amount of water or eye wash solution.
- If the medicine gets into a wound, cut, or crack in the skin, the area should be thoroughly rinsed with a large amount of water. Appropriate medical measures should be taken, depending on the injected dose. The instructions for preparing and disposing of the medicine should be strictly followed.
- Country of registration
- Active substance
- Prescription requiredYes
- ImporterMerz Pharma GmbH & Co. KGaA
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to XeominDosage form: Solution, 200 U Speywood/mlActive substance: botulinum toxinPrescription requiredDosage form: Powder, 125 Speywood unitsActive substance: botulinum toxinPrescription requiredDosage form: Powder, 125 Speywood unitsActive substance: botulinum toxinPrescription required
Alternatives to Xeomin in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Xeomin in Ukraine
Alternative to Xeomin in Spain
Online doctors for Xeomin
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Xeomin – subject to medical assessment and local rules.














