
Mirtor
Ask a doctor about a prescription for Mirtor

How to use Mirtor
Leaflet attached to the packaging: information for the user
Warning! Keep the leaflet! Information on the immediate packaging in a foreign language.
Mirtor
30 mg,orally disintegrating tablets
Mirtazapine
You should carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient.
- You should keep this leaflet, so that you can read it again if necessary.
- In case of any doubts, you should consult a doctor or pharmacist.
- This medicine has been prescribed to a specific person. It should not be given to others. The medicine may harm another person, even if the symptoms of their illness are the same.
- If the patient experiences any side effects, including any side effects not listed in this leaflet, they should tell their doctor, pharmacist, or nurse. See section 4.
Table of contents of the leaflet:
- 1. What is Mirtor and what is it used for
- 2. Important information before taking Mirtor
- 3. How to take Mirtor
- 4. Possible side effects
- 5. How to store Mirtor
- 6. Contents of the packaging and other information
1. What is Mirtor and what is it used for
Mirtor belongs to a group of medicines known as antidepressants.
Mirtor is used to treat depression in adults.
Mirtor starts working after 1-2 weeks of use, and after 2-4 weeks, there is an improvement in well-being. If after 2-4 weeks of treatment, there is no improvement or the patient feels worse, they should consult a doctor. More information is provided in section 3, "When can an improvement in well-being be expected".
2. Important information before taking Mirtor
When not to take Mirtor:
- if the patient is allergic to mirtazapine or any of the other ingredients of this medicine (listed in section 6). In such a case, before taking Mirtor, the patient should contact their doctor as soon as possible.
- if the patient is currently taking or has taken in the recent past (within the last 2 weeks) monoamine oxidase inhibitors (MAOIs).
Warnings and precautions
Before starting to take Mirtor, the patient should discuss it with their doctor or pharmacist.
Before starting to take Mirtor, the patient should tell their doctor:
if they have ever had a severe skin rash or skin peeling, blisters, and/or mouth sores after taking Mirtor.
Children and adolescents
Mirtor should not normally be used in children and adolescents under 18 years of age, as its efficacy has not been established in this age group. Additionally, patients under 18 years of age have a higher risk of side effects, such as suicidal attempts, suicidal thoughts, and hostility (mainly aggression, rebellious behavior, and anger), when taking medicines of this class. However, the doctor may prescribe Mirtor to patients of this age if they consider it to be in their best interest. If the doctor has prescribed Mirtor to a patient under 18 years of age, and any doubts arise, the patient should consult their doctor. In patients under 18 years of age taking Mirtor, the doctor should be informed if any of the above symptoms develop or worsen. The long-term effects of Mirtor on safety, including growth, maturation, and cognitive development in this age group, have not been established. Additionally, in this age group, after taking mirtazapine, significant weight gain has been reported more frequently than in adults.
Suicidal thoughts and worsening of depression
Patients with depression may sometimes have thoughts of self-harm or suicide. Such symptoms or behavior may worsen at the beginning of treatment with antidepressants, as these medicines usually start working after about 2 weeks, sometimes later. These symptoms are more likely in:
- patients who have had suicidal thoughts or attempts in the past;
- young adult patients. Clinical trial data show an increased risk of suicidal behavior in people under 25 years of age with mental disorders treated with antidepressants. If suicidal thoughts or attempts occur, the patient should immediately contact their doctor or go to the hospital.
It may be helpful to inform relatives or friendsabout the depression and ask them to read this leaflet. The patient may ask them to inform them if they notice that the depression or anxiety has worsened or if there are any worrying changes in behavior.
Also, when taking Mirtor, special caution should be exercised
- If the following conditions occur or have occurred: (The patient should inform their doctor about the occurrence of the following diseases before starting treatment with Mirtor, if they have not already done so.)
- epileptic seizures. If seizures occur or their frequency increases during treatment, the medicine should be discontinued and the doctor should be contacted immediately;
- liver disease, including jaundice. If jaundice occurs, the medicine should be discontinued and the doctor should be contacted immediately;
- kidney disease;
- heart diseaseor low blood pressure;
- schizophrenia. The doctor should be contacted immediately if such psychotic disorders as paranoid symptoms worsen or increase in frequency;
- manic depression(alternating periods of elevated mood/excitement and depression). If the patient feels excessively excited, the medicine should be discontinued and the doctor should be contacted immediately;
- diabetes(may require a change in insulin or other hypoglycemic medication dose);
- eye diseases, such as increased intraocular pressure (glaucoma);
- urination difficulties, which may be due to prostate enlargement;
- certain heart conditionsthat can cause changes in heart rhythm, recent myocardial infarction, heart failure, or the use of certain medications that can cause disturbances in heart rhythm.
- If symptoms of infection occur, such as unexplained fever, sore throat, mouth sores, the medicine should be discontinued, and the doctor should be consulted immediately, and a blood morphology test should be performed. In rare cases, these symptoms may be a sign of blood cell production disorders. These symptoms are rare and usually occur after 4-6 weeks of treatment.
- Older patients are often more sensitive, especially to the side effects of antidepressants.
- Severe skin reactions, including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), have been reported during treatment with mirtazapine. If the patient notices any of the symptoms described in section 4 related to these severe skin reactions, they should stop taking the medicine and consult their doctor immediately. If the patient has ever had severe skin reactions in the past, they should not restart treatment with mirtazapine.
Mirtor with other medicines
The patient should tell their doctor or pharmacist about all medicines they are currently taking or have recently taken, as well as any medicines they plan to take.
Mirtor should not be takenin combination with:
- monoamine oxidase inhibitors (MAOIs), or within 2 weeks of stopping MAOIs. MAOIs should not be started until 2 weeks after stopping Mirtor. MAOIs include moclobemide, tranylcypromine (antidepressants), and selegiline (used in the treatment of Parkinson's disease). Care should be takenwhen taking Mirtor in combination with:
- other antidepressants, such as SSRIs, venlafaxine, and L-tryptophan or triptans(used to treat migraines), tramadol(a pain reliever), buprenorphine, linezolid(an antibiotic), lithium salts(used to treat certain psychiatric disorders), methylene blue(used to reduce high methemoglobin levels in the blood), and preparations containing St. John's Wort (Hypericum perforatum)(herbal preparations used to treat depression). In patients taking only Mirtor or in combination with these medicines, serotonin syndrome can occur very rarely. Some of its symptoms include sudden fever, sweating, increased heart rate, diarrhea, (uncontrolled) muscle spasms, chills, increased reflexes, anxiety, mood changes, loss of consciousness. The patient should contact their doctor immediately if several of these symptoms occur at the same time.
- the antidepressant nefazodone. It may increase the level of Mirtor in the blood. The patient should inform their doctor about taking this medicine. It may be necessary to reduce the dose of Mirtor, and after stopping nefazodone, increase the dose of Mirtor.
- medicines used to treat anxiety and insomnia, such as benzodiazepines;
- medicines used to treat schizophrenia, such as olanzapine;
- medicines used to treat allergies, such as cetirizine;
- medicines used to treat severe pain, such as morphine. Mirtor in combination with these medicines may increase the drowsiness they cause.
- medicines used to treat infections, such as antibacterial agents (erythromycin), antifungal agents (such as ketoconazole), and medicines used to treat HIV/AIDS (such as HIV protease inhibitors), as well as medicines used to treat stomach ulcers (such as cimetidine). If these medicines are started at the same time as Mirtor, the level of Mirtor in the blood may increase. The patient should inform their doctor about taking these medicines. It may be necessary to reduce the dose of Mirtor, and after stopping these medicines, increase the dose of Mirtor.
- antiepileptic drugs, such as carbamazepine and phenytoin;
- medicines used to treat tuberculosis, such as rifampicin. When taken with Mirtor, these medicines may decrease the level of Mirtor in the blood. The patient should inform their doctor about taking these medicines. It may be necessary to increase the dose of Mirtor, and after stopping these medicines, decrease the dose of Mirtor.
- anticoagulants, such as warfarin. Mirtor may increase the effect of warfarin. The patient should inform their doctor about taking these medicines. When taking Mirtor in combination with these medicines, it is recommended to monitor blood tests.
- medicines that may affect heart rhythm, such as certain antibiotics and antipsychotic medicines.
Mirtor with food and alcohol
Drinking alcohol while taking Mirtor may cause drowsiness. It is best to avoid consuming alcohol during treatment with Mirtor.
Mirtor can be taken with or without food.
Pregnancy and breastfeeding
If the patient is pregnant, breastfeeding, thinks they may be pregnant, or plans to have a child, they should consult their doctor or pharmacist before taking this medicine.
Limited experience with the use of Mirtor in pregnant women does not indicate an increased risk. However, caution should be exercised when using the medicine during pregnancy.
If Mirtor is taken during pregnancy or shortly before birth, it is recommended to monitor the newborn for possible side effects.
Similar medicines (from the SSRI group) taken by pregnant women may increase the risk of a serious condition in the child, called persistent pulmonary hypertension of the newborn (PPHN), which causes rapid breathing and blue discoloration of the skin. These symptoms usually occur within the first day of life. If this happens, the patient should contact their midwife and/or doctor immediately.
Driving and using machines
Mirtor may reduce alertness and ability to concentrate. During treatment with Mirtor, the patient should avoid performing potentially hazardous tasks that require continuous attention, such as driving or operating machinery.
If the doctor has prescribed Mirtor to a patient under 18 years of age, the patient should make sure that the medicine does not affect their concentration and alertness before participating in traffic (e.g., cycling).
Mirtor contains aspartame (E 951), a source of phenylalanine
This medicine contains aspartame, which is a source of phenylalanine. Each 30 mg orally disintegrating tablet contains 6 mg of aspartame. Aspartame may be harmful to patients with phenylketonuria. This is a rare genetic disorder in which phenylalanine accumulates in the body due to its improper excretion.
3. How to take Mirtor
This medicine should always be used as directed by the doctor or pharmacist. In case of doubts, the patient should consult their doctor or pharmacist.
Mirtor is available in 15 mg, 30 mg, and 45 mg doses.
Dosage
The recommended initial dose is 15 or 30 mg per day.After a few days of treatment, the doctor may recommend increasing the dose to the most suitable for the patient (from 15 to 45 mg per day). Usually, the same dose of the medicine is used in patients of different ages. However, older patients or patients with kidney and liver diseases may be prescribed a different dose of Mirtor by their doctor.
When to take Mirtor
Mirtor should be taken daily at the same time, preferably in a single dose in the evening, before bedtime. However, the doctor may recommend taking two doses divided throughout the day - one in the morning and one in the evening before sleep. The larger dose should be taken in the evening, before bedtime.
Information about taking orally disintegrating tablets:
Mirtor tablets should be taken orally.
1. Do not crush the orally disintegrating tablet
To avoid crushing the orally disintegrating tablet, do not press on the blister (Figure A).
Figure A
2. Separate the blister with the tablet
Each blister contains 6 pockets with tablets, separated by a perforated line. The patient should bend the blister and separate one pocket along the perforated line (Figure 1).
3. Remove the foil
The patient should carefully remove the covering foil, starting from the corner marked with an arrow (Figures 2 and 3).
4. Remove the orally disintegrating tablet
The patient should remove the orally disintegrating tablet with dry hands from the packaging and place it on their tongue. (Figure 4).
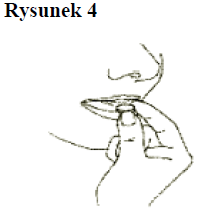
The tablet dissolves quickly and can be swallowed without drinking water.
When can an improvement in well-being be expected
The first signs of the medicine's effect can be expected after 1-2 weeks of treatment, and after 2-4 weeks, an improvement in well-being may occur.
It is essential to discuss the effects of Mirtor with the doctor during the first few weeks of treatment:
- After 2 to 4 weeks from the start of Mirtor treatment, the patient should discuss the treatment effects with their doctor. If there is no adequate clinical response, the doctor may increase the dose. After another 2 to 4 weeks, the patient should again discuss the treatment effects with their doctor. Treatment should be continued until the symptoms have completely disappeared, which usually takes 4 to 6 months.
What to do if a higher than recommended dose of Mirtor is taken
If the patient or anyone else has taken a higher dose of Mirtor than recommended, they should immediately consult their doctor.
Expected signs of Mirtor overdose (without other medicines and without alcohol) include drowsiness, disorientation, and rapid heartbeat. Signs of overdose may include changes in heart rhythm (rapid heartbeat, irregular heartbeat) and/or fainting. These may be symptoms of life-threatening ventricular arrhythmias, known as "torsades de pointes".
What to do if a dose of Mirtor is missed
If a dose is missed that is supposed to be taken once a day
- the patient should not take a double dose to make up for the missed tablet. They should take the next dose at the usual time.
If the medicine is supposed to be taken twice a day
- if the morning dose is missed - the patient should take it together with the evening dose;
- if the evening dose is missed - the patient should not take it together with the morning dose; they should skip it and continue treatment, taking the usual morning and evening doses;
- if both doses are missed - the patient should not try to make them up; they should skip them. The next day, they should continue treatment, taking the usual morning and evening doses.
Stopping treatment with Mirtor
The patient should only stop taking Mirtor under the strict guidance of their doctor.
The patient should not stop taking the medicine too early, as this may cause the illness to recur. If an improvement occurs, the patient should discuss it with their doctor. The doctor will inform them when they can stop treatment.
Suddenly stopping treatment with Mirtor, even if the symptoms of depression have disappeared, may cause nausea, dizziness, restlessness, or anxiety and headache. These symptoms will not occur during gradual discontinuation of the medicine. The doctor will inform the patient how to gradually reduce the dose of Mirtor.
If the patient has any further doubts about taking this medicine, they should consult their doctor or pharmacist.
4. Possible side effects
Like all medicines, Mirtor can cause side effects, although not everybody gets them.
In case of any of the following serious side effects, the patient should stop taking Mirtor and immediately consult their doctor.
Uncommon(may affect up to 1 in 100 people):
- increased mood and increased mental activity (mania)
Rare(may affect up to 1 in 1,000 people):
- yellowing of the whites of the eyes and skin, which may indicate liver problems (jaundice); Frequency not known(frequency cannot be estimated from the available data):
- signs of infection, such as sudden and unexplained high fever, sore throat, and mouth sores (agranulocytosis). In rare cases, mirtazapine may cause blood cell production disorders. In some people, it may cause a temporary decrease in the number of white blood cells (granulocytopenia). In rare cases, mirtazapine may cause a decrease in the number of white blood cells, red blood cells, and platelets (aplastic anemia), a decrease in platelets (thrombocytopenia), or an increase in white blood cells (eosinophilia).
- seizures (convulsions)
- a combination of symptoms such as unexplained fever, sweating, increased heart rate, diarrhea, (uncontrolled) muscle spasms, chills, increased reflexes, anxiety, mood changes, loss of consciousness. In very rare cases, these symptoms may indicate the development of serotonin syndrome.
- thoughts of self-harm or suicidal thoughts
- severe skin reactions:
- red spots resembling a target or round spots, often with central blisters on the torso, skin peeling, mouth sores, and genital and eye lesions. The occurrence of such severe skin rashes is often preceded by fever and flu-like symptoms (Stevens-Johnson syndrome, toxic epidermal necrolysis).
- widespread rash, high body temperature, and enlarged lymph nodes (DRESS or drug hypersensitivity syndrome).
Other possible side effects include:
Very common
- increased appetite and weight gain
- calmness or drowsiness
- headache
- dry mouth
Common
- lethargy
- dizziness
- seizures or tremors
- nausea
- diarrhea
- vomiting
- constipation
- rash or skin eruptions
- joint pain, muscle pain
- back pain
- dizziness or fainting when changing body position quickly (orthostatic hypotension)
- swelling (usually of the ankles or feet) due to fluid accumulation (edema)
- fatigue
- intensive dreams
- disorientation
- feeling of anxiety
- sleep disturbances
- memory disturbances, which usually resolve after stopping treatment
Uncommon
- abnormal skin sensations, such as burning, tingling, or numbness (paresthesia)
- restless legs syndrome
- fainting
- numbness in the mouth (oral hypoesthesia)
- low blood pressure
- nightmares
- agitation
- hallucinations
- urge to move
Rare
- muscle twitching or spasms (clonic muscle spasms)
- aggressive behavior
- abdominal pain and nausea, which may indicate pancreatitis
Frequency not known(frequency cannot be estimated from the available data):
- abnormal sensations in the mouth (oral paresthesia)
- mouth swelling
- generalized swelling
- local swelling
- low sodium levels in the blood
- improper secretion of antidiuretic hormone
- severe skin reactions (blistering skin disease, polymorphic erythema)
- sleepwalking (somnambulism)
- speech disorders
- increased creatine kinase levels in the blood
- urination difficulties (urinary retention)
- muscle pain, stiffness, and/or weakness
- darkening or discoloration of urine (rhabdomyolysis)
- increased prolactin levels in the blood (hyperprolactinemia, including breast enlargement and/or milk secretion from the nipples)
- prolonged or painful erections
Additional side effects in children and adolescents
The following side effects were commonly observed in clinical trials with children under 18 years of age: significant weight gain, hives, and increased triglyceride levels in the blood.
Reporting side effects
If any side effects occur, including any side effects not listed in the leaflet, the patient should tell their doctor, pharmacist, or nurse. Side effects can be reported directly to the Department of Adverse Reaction Monitoring of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, tel.: +48 22 49 21 301, fax: +48 22 49 21 309, website: https://smz.ezdrowie.gov.pl.
By reporting side effects, more information can be collected on the safety of the medicine.
5. How to store Mirtor
The medicine should be stored in a place that is out of sight and reach of children.
The medicine should not be used after the expiry date stated on the packaging.
The expiry date refers to the last day of the specified month.
There are no special precautions for storage.
The medicine should not be used if any discoloration or other signs of deterioration are noticed.
Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Contents of the packaging and other information
What Mirtor contains
- The active substance of Mirtor is mirtazapine. Each orally disintegrating tablet contains 30 mg of mirtazapine.
- Other ingredients of the medicine are crospovidone, mannitol (E 421), microcrystalline cellulose, aspartame (E 951), strawberry-guarana flavor, peppermint flavor, colloidal anhydrous silica, magnesium stearate.
What Mirtor looks like and contents of the packaging
Orally disintegrating tablet, 30 mg: white, round, marked with "37" on one side and "A" on the other side.
30 or 90 tablets in a cardboard box.
For more detailed information, the patient should contact the marketing authorization holder or the parallel importer.
Marketing authorization holder in the Czech Republic, the country of export:
Orion Corporation, Orionintie 1/A, FI-02200 Espoo, Finland
Manufacturer:
Orion Corporation Orion Pharma, Orionintie 1, FI-02200 Espoo, Finland
Parallel importer:
InPharm Sp. z o.o., ul. Strumykowa 28/11, 03-138 Warsaw
Repackaged by:
InPharm Sp. z o.o. Services sp. k., ul. Chełmżyńska 249, 04-458 Warsaw
Marketing authorization number in the Czech Republic, the country of export:30/415/06-C
Parallel import authorization number: 265/22 Date of leaflet approval: 29.06.2022
[Information about the trademark]
- Country of registration
- Active substance
- Prescription requiredYes
- Marketing authorisation holder (MAH)Orion Corporation
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to MirtorDosage form: Tablets, 15 mgActive substance: mirtazapinePrescription requiredDosage form: Tablets, 30 mgActive substance: mirtazapinePrescription requiredDosage form: Tablets, 45 mgActive substance: mirtazapinePrescription required
Alternatives to Mirtor in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Mirtor in Hiszpania
Alternative to Mirtor in Ukraina
Online doctors for Mirtor
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Mirtor – subject to medical assessment and local rules.









