
Lacosamide Fresenius Kabi
Ask a doctor about a prescription for Lacosamide Fresenius Kabi

How to use Lacosamide Fresenius Kabi
Package Leaflet: Information for the Patient
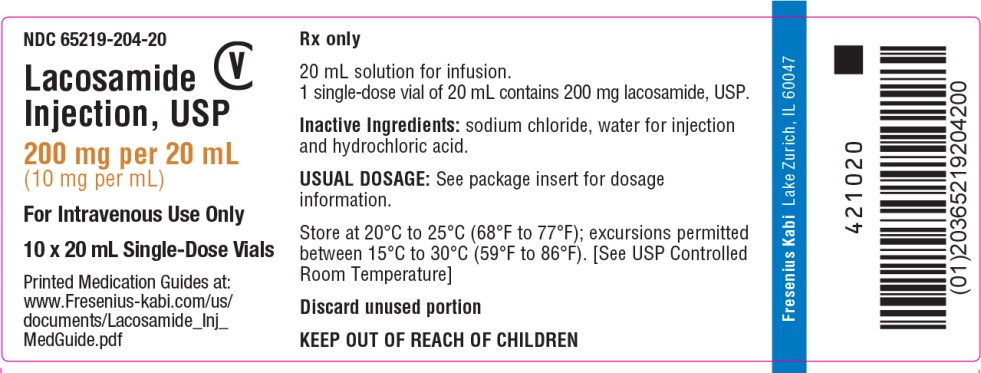
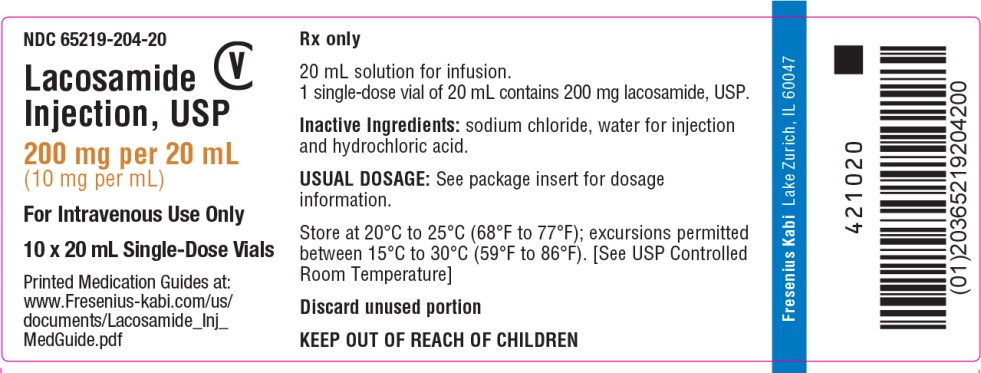
Lacosamide Fresenius Kabi, 10 mg/ml, Solution for Infusion
Lacosamide
Read the Package Leaflet Carefully Before Using the Medication, as it Contains Important Information for the Patient.
Keep this package leaflet, you may need to read it again.
In case of any doubts, consult a doctor or pharmacist.
If the patient experiences any side effects, including those not listed in this package leaflet, they should inform their doctor or pharmacist. See section 4.
Table of Contents of the Package Leaflet
- 1. What is Lacosamide Fresenius Kabi and What is it Used For
- 2. Important Information Before Using Lacosamide Fresenius Kabi
- 3. How to Use Lacosamide Fresenius Kabi
- 4. Possible Side Effects
- 5. How to Store Lacosamide Fresenius Kabi
- 6. Package Contents and Other Information
1. What is Lacosamide Fresenius Kabi and What is it Used For
What is Lacosamide Fresenius Kabi
Lacosamide Fresenius Kabi contains lacosamide. It belongs to a group of medications called "antiepileptic drugs", which are used to treat epilepsy.
This medication has been prescribed by a doctor to reduce the number of seizures.
What is Lacosamide Fresenius Kabi Used For
Lacosamide Fresenius Kabi is used:
- as monotherapy and in combination with other antiepileptic medications in adults, adolescents, and children from 2 years of age for the treatment of a type of epilepsy characterized by partial seizures and secondary generalized seizures. In this type of epilepsy, seizures initially affect only one side of the brain but may then spread to other areas on both sides of the brain.
- in combination with other antiepileptic medications in adults, adolescents, and children from 4 years of age for the treatment of primary generalized tonic-clonic seizures (grand mal seizures involving loss of consciousness) in patients with generalized idiopathic epilepsy (a type of epilepsy considered to have a genetic basis).
2. Important Information Before Using Lacosamide Fresenius Kabi
When Not to Use Lacosamide Fresenius Kabi
if the patient is allergic to lacosamide or any of the other ingredients of this medication (listed in section 6). In case of doubt about the existence of an allergy, consult a doctor.
if the patient has a certain type of heart rhythm disorder (called second or third degree atrioventricular block).
If any of the above situations apply to the patient, they should not use Lacosamide Fresenius Kabi. In case of doubt, before using this medication, consult a doctor or pharmacist.
Warnings and Precautions
Before starting treatment with Lacosamide Fresenius Kabi, the patient should consult a doctor if:
the patient thinks about self-harm or suicide. In some patients treated with antiepileptic medications, such as lacosamide, thoughts of self-harm or suicidal thoughts have occurred. If such thoughts occur, the patient should immediately contact their doctor.
the patient has a heart condition that affects the heart rhythm - often it is slowed, accelerated, or irregular (i.e., atrioventricular block, atrial fibrillation, and atrial flutter).
the patient has severe heart disease, such as heart failure or has had a heart attack.
the patient often experiences dizziness or falls. Lacosamide Fresenius Kabi may cause dizziness, which can increase the risk of accidental injury or falls.
Therefore, caution should be exercised until the body gets used to the action of the medication.
If any of the above situations occur (or there are doubts about them), before starting treatment with Lacosamide Fresenius Kabi, the patient should consult a doctor or pharmacist.
If the patient is using Lacosamide Fresenius Kabi and experiences new types of seizures or worsening of existing seizures, they should inform their doctor.
If the patient is using Lacosamide Fresenius Kabi and experiences symptoms of abnormal heart rhythm (such as slow, fast, irregular heartbeat, palpitations, shortness of breath, dizziness, fainting), they should immediately contact their doctor (see section 4).
Children
Lacosamide is not recommended for children under 2 years of age with epilepsy characterized by partial seizures, and it is not recommended for children under 4 years of age with primary generalized tonic-clonic seizures. The efficacy and safety of the medication in this age group are not yet known.
Lacosamide Fresenius Kabi and Other Medications
The patient should inform their doctor or pharmacist about all medications they are currently using or have recently used, as well as any medications they plan to use.
Particularly, the patient should inform their doctor or pharmacist about the use of any of the following medications that affect heart function, as lacosamide also affects heart function:
medications used for heart conditions;
medications that may cause prolongation of the PQ interval (visible in the electrocardiogram EKG), such as medications used to treat epilepsy or pain, e.g., carbamazepine, lamotrigine, or pregabalin;
medications used in the treatment of certain types of heart rhythm disorders or heart failure.
If any of the above situations occur (or there are doubts about them), before starting treatment with Lacosamide Fresenius Kabi, the patient should consult a doctor or pharmacist.
The patient should also inform their doctor or pharmacist about the use of any of the following medications, as they may decrease or increase the effectiveness of Lacosamide Fresenius Kabi:
- medications used for fungal infections, such as fluconazole, itraconazole, or ketoconazole;
- medications used for HIV infection, such as ritonavir;
- medications used for bacterial infections, such as clarithromycin or rifampicin;
- a herbal remedy used for mild anxiety and depression - St. John's Wort. If any of the above situations occur (or there are doubts about them), before starting treatment with Lacosamide Fresenius Kabi, the patient should consult a doctor or pharmacist.
Lacosamide Fresenius Kabi with Alcohol
For safety reasons, the patient should not drink alcohol while using Lacosamide Fresenius Kabi.
Pregnancy and Breastfeeding
Women of childbearing age should discuss the use of contraception with their doctor.
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a child, they should consult their doctor or pharmacist before using this medication.
Lacosamide Fresenius Kabi is not recommended during pregnancy or breastfeeding, as its effect on the course of pregnancy and the unborn child or newborn is not known.
It is also not known whether Lacosamide Fresenius Kabi passes into human milk. The patient should urgently consult their doctor if they become pregnant or plan to become pregnant. The doctor will help decide whether Lacosamide Fresenius Kabi can be used.
The patient should not stop treatment without consulting their doctor, as this may increase the frequency of seizures. The severity of the mother's symptoms may also harm the child.
Driving and Operating Machines
The patient should not drive a car, ride a bike, or use tools or operate machines until they are sure how the medication affects them. This is because Lacosamide Fresenius Kabi may cause dizziness or blurred vision.
Lacosamide Fresenius Kabi Contains Sodium
The medication contains 59.8 mg of sodium (the main component of table salt) in each vial, which corresponds to 3% of the recommended maximum daily sodium intake for an adult.
3. How to Use Lacosamide Fresenius Kabi
This medication should always be used as directed by a doctor or pharmacist. In case of doubt, the patient should consult a doctor or pharmacist.
Using Lacosamide Fresenius Kabi
Treatment with Lacosamide Fresenius Kabi can be started with:
- oral administration or
- intravenous infusion (iv.), during which the doctor or nurse administers the medication into the patient's vein. The infusion time is from 15 to 60 minutes. Intravenous infusion is usually used for a short time when the medication cannot be administered orally. The doctor will decide how many days the patient will receive infusions. There are data on the use of lacosamide in infusion twice a day for up to 5 days. In long-term treatment, lacosamide is used in tablets and syrup.
When changing the method of administration from infusion to oral (and vice versa), the total daily dose and frequency of administration remain unchanged.
Lacosamide should be used twice a day (approximately every 12 hours).
The medication should be used at approximately the same time every day.
What Dose to Use
The following are the usual recommended doses of lacosamide for patients of different age groups and body weights. The doctor may prescribe a different dose if the patient has kidney or liver function disorders.
Adolescents and Children with a Body Weight of at Least 50 kg and Adults
Using Lacosamide Fresenius Kabi alone
The usual initial dose of lacosamide is 50 mg twice a day.
Treatment can also be started with a dose of 100 mg of lacosamide twice a day.
The doctor may increase the administered dose twice a day by 50 mg every week until a maintenance dose is reached, which is from 100 mg to 300 mg twice a day.
Using Lacosamide Fresenius Kabi with other antiepileptic medications
The usual initial dose of lacosamide is 50 mg twice a day.
The doctor may increase the administered dose twice a day by 50 mg every week until a maintenance dose is reached, which is from 100 mg to 200 mg twice a day.
In patients with a body weight of at least 50 kg, the doctor may decide to start administering lacosamide with a single loading dose of 200 mg. Then, after 12 hours, the patient will start using a fixed maintenance dose.
Children and Adolescents with a Body Weight Below 50 kg
Using in the treatment of partial seizures:note that lacosamide is not recommended for use in children under 2 years of age.
Using in the treatment of primary generalized tonic-clonic seizures: note that lacosamide is not recommended for use in children under 4 years of age.
Using Lacosamide Fresenius Kabi alone
The doctor will determine the dose of lacosamide based on the patient's body weight.
The usual initial dose of lacosamide is 1 mg (0.1 ml) per kilogram of body weight, twice a day.
The doctor may increase the administered dose twice a day by 1 mg (0.1 ml) per kilogram of body weight every week until a maintenance dose is reached.
The dosage tables, including the recommended maximum dose, are presented below for informational purposes only. The doctor will calculate the appropriate dose for the patient.
Doses used twice a dayin children from 2 years of age with a body weight from 10 kg to
below 40 kg:
Doses used twice a dayin children and adolescents with a body weight from 40 kg to
below 50 kg:
Using Lacosamide Fresenius Kabi with other antiepileptic medications
The doctor will determine the appropriate dose of lacosamide based on the patient's body weight.
In children and adolescents with a body weight from 10 kg to below 50 kg, the usual initial dose is 1 mg (0.1 ml) per kilogram of body weight, twice a day.
| Body Weight | Week 1. Initial Dose: 0.1 ml/kg body weight. | Week 2. 0.2 ml/kg body weight. | Week 3. 0.3 ml/kg body weight. | Week 4. 0.4 ml/kg body weight. | Week 5. 0.5 ml/kg body weight. | Week 6. Maximum Recommended Dose: 0.6 ml/kg body weight. |
| 10 kg | 1 ml | 2 ml | 3 ml | 4 ml | 5 ml | 6 ml |
| 15 kg | 1.5 ml | 3 ml | 4.5 ml | 6 ml | 7.5 ml | 9 ml |
| 20 kg | 2 ml | 4 ml | 6 ml | 8 ml | 10 ml | 12 ml |
| 25 kg | 2.5 ml | 5 ml | 7.5 ml | 10 ml | 12.5 ml | 15 ml |
| 30 kg | 3 ml | 6 ml | 9 ml | 12 ml | 15 ml | 18 ml |
| 35 kg | 3.5 ml | 7 ml | 10.5 ml | 14 ml | 17.5 ml | 21 ml |
| Body Weight | Week 1. Initial Dose: 0.1 ml/kg body weight. | Week 2. 0.2 ml/kg body weight. | Week 3. 0.3 ml/kg body weight. | Week 4. 0.4 ml/kg body weight. | Week 5. Maximum Recommended Dose: 0.5 ml/kg body weight. |
| 40 kg | 4 ml | 8 ml | 12 ml | 16 ml | 20 ml |
| 45 kg | 4.5 ml | 9 ml | 13.5 ml | 18 ml | 22.5 ml |
The doctor may increase the administered dose twice a day by 1 mg (0.1 ml) per kilogram of body weight every week until a maintenance dose is reached.
The dosage tables, including the recommended maximum dose, are presented below for informational purposes only. The doctor will calculate the appropriate dose for the patient.
Doses used twice a dayin children from 2 years of age with a body weight from 10 kg to
below 20 kg:
Doses used twice a dayin children and adolescents with a body weight from 20 kg to
below 30 kg:
Doses used twice a dayin children and adolescents from 4 years of age with a body weight from
30 kg to below 50 kg:
Stopping Lacosamide Fresenius Kabi
If the doctor decides to stop using Lacosamide Fresenius Kabi, they will gradually reduce the dose of the medication. This is to prevent the recurrence of epilepsy or its exacerbation.
In case of doubts related to the use of this medication, the patient should consult a doctor or pharmacist.
4. Possible Side Effects
Like all medications, Lacosamide Fresenius Kabi can cause side effects, although not everybody gets them.
Side effects from the nervous system, such as dizziness, may be stronger after a single loading dose.
The Patient Should Inform Their Doctor or Pharmacist if They Experience Any of the Following Symptoms:
Very Common(may occur more often than in 1 in 10 patients):
headache;
dizziness or nausea (vomiting);
double vision.
Common(may occur less often than in 1 in 10 patients):
short muscle jerks or muscle groups (myoclonic seizures);
| Body Weight | Week 1. Initial Dose: 0.1 ml/kg | Week 2. 0.2 ml/kg body weight. | Week 3. 0.3 ml/kg body weight. | Week 4. 0.4 ml/kg body weight. | Week 5. 0.5 ml/kg body weight. | Week 6. Maximum Recommended Dose: 0.6 ml/kg body weight. |
| 10 kg | 1 ml | 2 ml | 3 ml | 4 ml | 5 ml | 6 ml |
| 15 kg | 1.5 ml | 3 ml | 4.5 ml | 6 ml | 7.5 ml | 9 ml |
| Body Weight | Week 1. Initial Dose: 0.1 ml/kg body weight. | Week 2. 0.2 ml/kg body weight. | Week 3. 0.3 ml/kg body weight. | Week 4. 0.4 ml/kg body weight. | Week 5. Maximum Recommended Dose: 0.5 ml/kg body weight. |
| 20 kg | 2 ml | 4 ml | 6 ml | 8 ml | 10 ml |
| 25 kg | 2.5 ml | 5 ml | 7.5 ml | 10 ml | 12.5 ml |
| Body Weight | Week 1. Initial Dose: 0.1 ml/kg body weight. | Week 2. 0.2 ml/kg body weight. | Week 3. 0.3 ml/kg body weight. | Week 4. Maximum Recommended Dose: 0.4 ml/kg body weight. |
| 30 kg | 3 ml | 6 ml | 9 ml | 12 ml |
| 35 kg | 3.5 ml | 7 ml | 10.5 ml | 14 ml |
| 40 kg | 4 ml | 8 ml | 12 ml | 16 ml |
| 45 kg | 4.5 ml | 9 ml | 13.5 ml | 18 ml |
difficulty with coordination or walking;
balance disorders, tremors, numbness (paresthesia), muscle cramps, tendency to fall or bruise;
memory disorders, thinking disorders, difficulty finding words, confusion;
rapid uncontrolled eye movements (nystagmus), blurred vision;
a feeling of spinning (dizziness), a feeling of being drunk;
vomiting, dry mouth, constipation, indigestion, excess gas in the stomach or intestines, diarrhea;
decreased sensation and sensitivity to stimuli, speech difficulties, attention disorders;
ringing in the ears, such as buzzing, ringing, or whistling;
irritability, difficulty sleeping, depression;
drowsiness, fatigue, or weakness (asthenia);
itching, rash.
Uncommon(may occur less often than in 1 in 100 patients):
slow heart rate, palpitations, irregular heartbeat, or other changes in heart electrical activity (conduction disorders);
excessive well-being, seeing and (or) hearing non-existent things;
allergic reaction after taking the medication, hives;
abnormal liver blood test results (indicating abnormal liver function, liver damage);
thoughts of self-harm or suicide or attempted suicide: the patient should immediately inform their doctor;
feeling angry or agitated;
thinking disorders or loss of contact with reality;
severe allergic reactions causing swelling of the face, throat, hands, feet, ankles, or lower legs;
fainting;
involuntary movements (dyskinesia).
Frequency Not Known(frequency cannot be estimated from the available data):
abnormal rapid heart rhythm (tachyarrhythmia);
sore throat, high fever, and frequent infections. Blood tests may show a significant decrease in the number of a certain type of white blood cell (agranulocytosis);
severe skin reaction, which may be accompanied by high fever and flu-like symptoms, rash on the face, spreading rash, swollen lymph nodes (enlarged lymph nodes). Blood tests may show increased liver enzyme levels and an increased number of one type of white blood cell (eosinophilia);
widespread rash with blisters and peeling skin, occurring mainly in the area of the mouth, eyes, nose, and genitals (Stevens-Johnson syndrome) and a more severe form of rash causing skin peeling over more than 30% of the body surface (toxic epidermal necrolysis);
seizures.
Additional Side Effects Related to Intravenous Infusion
Local side effects may occur, such as:
Common(may occur less often than in 1 in 10 patients):
Pain, discomfort, or irritation at the injection site.
Uncommon(may occur less often than in 1 in 100 patients):
Redness at the injection site.
Additional Side Effects in Children
Additional side effects in children included fever, runny nose (nasopharyngitis), sore throat (pharyngitis), decreased appetite, behavioral changes, the child does not behave as usual (abnormal behavior), and lack of energy (lethargy). Drowsiness is a very common side effect in children and may occur in more than 1 in 10 children.
Reporting Side Effects
If side effects occur, including those not listed in this package leaflet, the patient should inform their doctor, pharmacist, or nurse. Side effects can be reported directly to the Department of Drug Safety Monitoring of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products
Al. Jerozolimskie 181C
02-222 Warsaw
phone: +48 22 49 21 301
fax: +48 22 49 21 309
website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
Reporting side effects will help to gather more information on the safety of the medication.
5. How to Store Lacosamide Fresenius Kabi
The medication should be stored out of sight and reach of children.
Do not use this medication after the expiry date stated on the carton and vial after "EXP". The expiry date refers to the last day of the month stated.
Do not store above 25°C.
Each vial of Lacosamide Fresenius Kabi should be used only once (single use).
Unused portions of the solution should be discarded.
Only clear solutions without visible particles and color changes should be used.
Medications should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medications they no longer use. This will help protect the environment.
6. Package Contents and Other Information
What Lacosamide Fresenius Kabi Contains
The active substance of the medication is lacosamide.
1 ml of the solution for infusion contains 10 mg of lacosamide.
1 vial contains 20 ml of the solution for infusion, which corresponds to 200 mg of lacosamide.
The other ingredients are sodium chloride, hydrochloric acid 0.86%, and water for injections.
What Lacosamide Fresenius Kabi Looks Like and What the Package Contains
Lacosamide Fresenius Kabi, 10 mg/ml, solution for infusion is a clear, colorless solution.
Lacosamide Fresenius Kabi is available in packages: 1 vial, 5 vials, and 10 vials. Each vial contains 20 ml of the solution for infusion.
Not all package sizes may be marketed.
Marketing Authorization Holder
Fresenius Kabi Polska Sp. z o.o.
Al. Jerozolimskie 134
02-305 Warsaw
Manufacturer
Fresenius Kabi Deutschland GmbH
Pfingstweide 53
61169 Friedberg
Germany
Labesfal - Laboratórios Almiro, S.A.
Zona Industrial do Lagedo
3465-157 Santiago de Besteiros
Portugal
To obtain more detailed information, the patient should contact the marketing authorization holder:
Fresenius Kabi Polska Sp. z o.o.
Al. Jerozolimskie 134
02-305 Warsaw
phone: +48 22 345 67 89
This Medication is Authorized in the Member States of the European Economic Area and in the United Kingdom (Northern Ireland) Under the Following Names:
| Member State | Medication Name |
| Austria | Lacosamid Fresenius Kabi 10 mg/ml Infusionslösung |
| Bulgaria | Lacosamide Fresenius Kabi 10 mg/ml solution for infusion |
| Cyprus | Lacosamide Fresenius Kabi 10mg/ml διάλυμα για έγχυση |
| Czech Republic | Lacosamide Fresenius Kabi |
| Estonia | Lacosamide Fresenius Kabi |
| Finland | Lacosamide Fresenius Kabi 10 mg/ml solution for infusion |
| France | LACOSAMIDE FRESENIUS KABI 10 mg/ml, solution pour perfusion |
| Greece | Lacosamide Fresenius Kabi 10mg/ml solution for infusion |
| Spain | Lacosamida Fresenius Kabi 10 mg/ml solución para perfusión EFG |
| Ireland | Lacosamide Fresenius Kabi 10mg/ml solution for infusion |
| Liechtenstein | Lacosamid Fresenius Kabi 10 mg/ml Infusionslösung |
| Lithuania | Lacosamide Fresenius Kabi 10 mg/ml infuzinis tirpalas |
| Luxembourg | Lacosamide Fresenius Kabi 10 mg/ml Infusionslösung |
| Latvia | Lacosamide Fresenius Kabi 10 mg/ml šķīdums infūzijām |
| Malta | Lacosamide Fresenius Kabi 10 mg/ml solution for infusion |
| Germany | Lacosamide Fresenius Kabi 10 mg/ml Infusionslösung |
| Norway | Lacosamide Fresenius Kabi |
| Poland | Lacosamide Fresenius Kabi |
| Portugal | Lacosamida Fresenius Kabi |
| Romania | Lacosamid Fresenius Kabi 10 mg/ml soluție perfuzabilă |
| Slovakia | Lacosamide Fresenius Kabi 10 mg/ml |
| Hungary | Lacosamide Fresenius Kabi 10 mg/ml oldatos infúzió |
| United Kingdom (Northern Ireland) | Lacosamide Fresenius Kabi 10 mg/ml solution for infusion |
| Italy | Lacosamide Fresenius Kabi |
Date of Last Revision of the Package Leaflet:23.12.2023
--------------------------------------------------------------------------------------------------------------------
Information Intended for Healthcare Professionals Only:
Each vial of Lacosamide Fresenius Kabi should be used only once (single use).
Unused portions of the solution should be discarded (see section 3).
Lacosamide Fresenius Kabi can be administered without prior dilution or can be diluted with the following solutions: sodium chloride 9 mg/ml (0.9%), glucose 50 mg/ml (5%), or Ringer's solution with lactate.
For the diluted medication, chemical and physical stability has been demonstrated for 7 days at a temperature up to 25°C and stored in glass containers or bags (PVC or non-PVC).
From a microbiological point of view, the medication should be used immediately. If not used immediately, the responsibility for the storage time and conditions lies with the user. The solution should not be stored for more than 24 hours at a temperature between 2°C and 8°C, unless it was prepared in controlled and validated aseptic conditions.
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterFresenius Kabi Deutschland GmbH Labesfal - Laboratórios Almiro, S.A.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Lacosamide Fresenius KabiDosage form: Tablets, 50 mgActive substance: lacosamideManufacturer: Symphar Sp. z o.o.Prescription requiredDosage form: Tablets, 100 mgActive substance: lacosamideManufacturer: Symphar Sp. z o.o.Prescription requiredDosage form: Tablets, 150 mgActive substance: lacosamideManufacturer: Symphar Sp. z o.o.Prescription required
Alternatives to Lacosamide Fresenius Kabi in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Lacosamide Fresenius Kabi in Spain
Alternative to Lacosamide Fresenius Kabi in Ukraine
Online doctors for Lacosamide Fresenius Kabi
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Lacosamide Fresenius Kabi – subject to medical assessment and local rules.







