

Ibum Forte Pure

Ask a doctor about a prescription for Ibum Forte Pure

How to use Ibum Forte Pure
Leaflet attached to the packaging: patient information
IBUM FORTE PURE
200 mg/5 ml, oral suspension
Ibuprofen
It is necessary to carefully read the contents of the leaflet before using the medicine, as it contains important information for the patient.
This medicine should always be used exactly as described in this patient leaflet or as directed by a doctor or pharmacist.
- The leaflet should be kept in case it needs to be read again.
- If advice or additional information is needed, a pharmacist should be consulted.
- If the patient experiences any side effects, including any possible side effects not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
- If after 1 day (infants 3-5 months old) or 3 days (children over 6 months old, adolescents, and adults) there is no improvement or the patient feels worse, they should contact a doctor.
Table of contents of the leaflet
- 1. What is I F P and what is it used for
- 2. Important information before taking I F P
- 3. How to take I F P
- 4. Possible side effects
- 5. How to store I F P
- 6. Contents of the packaging and other information
1. What is I F P and what is it used for
I F P contains ibuprofen, a substance from the group of non-steroidal anti-inflammatory drugs (NSAIDs), with analgesic, antipyretic, and anti-inflammatory effects.
Indications for use
- Fever of various origins, including influenza, colds, and post-vaccination reactions;
- Pain of various origins with mild to moderate severity, such as:
- headaches, throat and muscle pain (e.g., with viral infections),
- toothaches, pain after dental procedures, pain due to teething,
- joint and bone pain due to injuries to the musculoskeletal system (e.g., sprains),
- pain due to soft tissue injuries,
- post-operative pain,
- ear pain occurring in middle ear inflammatory conditions.
2. Important information before taking I F P
When not to take I F P:
- if the patient is hypersensitive to ibuprofen, other non-steroidal anti-inflammatory drugs (NSAIDs), or any of the other ingredients of this medicine (listed in section 6),
- in patients with active or history of peptic ulcer disease of the stomach and/or duodenum, perforation (hole) or bleeding, also occurring after NSAID use,
- in patients who have had in the past any symptoms of allergy after taking acetylsalicylic acid or other non-steroidal anti-inflammatory drugs, such as runny nose, hives, difficulty breathing, or asthma,
- in patients with severe dehydration (caused by vomiting, diarrhea, or insufficient fluid intake),
- when taking other NSAIDs (including COX-2 inhibitors such as celecoxib or etoricoxib),
- in case of severe liver or kidney failure,
- if the patient has severe heart failure (NYHA class IV),
- if there is bleeding in the brain (cerebral hemorrhage) or other bleeding,
- if there are blood coagulation disorders, bleeding tendency, or unexplained blood disorders,
- if the patient is in the last 3 months of pregnancy.
Warnings and precautions
Before starting I F P, the patient should discuss with their doctor or pharmacist:
- if the patient is taking other painkillers from the NSAID group or acetylsalicylic acid in a daily dose above 75 mg,
- if the patient has certain skin diseases (systemic lupus erythematosus, mixed connective tissue disease),
- if the patient has gastrointestinal diseases and chronic inflammatory bowel diseases (ulcerative colitis, Crohn's disease),
- if the patient has high blood pressure and/or heart function disorders,
- if the patient has kidney function disorders,
- if the patient has liver diseases,
- after recent major surgery,
- if there is dehydration (especially in children and adolescents) due to increased risk of kidney failure,
- in case of current or past asthma, chronic rhinitis, nasal polyps, or allergic diseases, as there may be a risk of shortness of breath,
- when taking other medicines that may increase the risk of gastrointestinal side effects, such as oral corticosteroids (e.g., prednisolone), blood thinners (e.g., acenocoumarol), selective serotonin reuptake inhibitors (antidepressants), and antiplatelet agents (such as acetylsalicylic acid).
During ibuprofen use, severe skin reactions have occurred, such as exfoliative dermatitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, and drug reaction with eosinophilia and systemic symptoms (DRESS), as well as acute generalized exanthematous pustulosis (AGEP). If the patient experiences any symptoms related to these severe skin reactions described in section 4, they should immediately stop taking I F P and seek medical help.
Concomitant, long-term use of painkillers may lead to persistent serious kidney disease.
I F P may mask symptoms of existing infection or fever.
Taking anti-inflammatory or pain-relieving medicines like ibuprofen may be associated with a small increased risk of heart attack or stroke, especially when used in high doses. The recommended dose should not be exceeded, and treatment should not be prolonged.
Before taking I F P, the patient should discuss treatment with their doctor or pharmacist if:
- the patient has heart diseases, such as heart failure, angina pectoris (chest pain), has had a heart attack, coronary artery bypass grafting, has peripheral arterial disease (poor blood circulation in the legs due to narrowed or blocked arteries), or has had any stroke (including mini-stroke or transient ischemic attack - TIA);
- the patient has high blood pressure, diabetes, high cholesterol levels, or has a family history of heart disease or stroke, or smokes.
- the patient has an infection - see below, section titled "Infections".
During ibuprofen use, symptoms of allergic reaction to this medicine have occurred, including difficulty breathing, facial and neck swelling (angioedema), and chest pain.
If any of these symptoms are noticed, I F P should be stopped immediately, and medical help should be sought.
During chickenpox, I F P should be avoided.
If any of the above conditions apply to a child, a doctor should be consulted before taking I F P.
There is a risk of gastrointestinal bleeding, ulceration, or perforation, which may not be preceded by warning signs or may occur in patients who have had such warning signs.
Infections
I F P may hide symptoms of infection, such as fever and pain. As a result, I F P may delay the use of appropriate infection treatment and lead to increased risk of complications. This has been observed in bacterial pneumonia and bacterial skin infections associated with chickenpox. If the patient is taking this medicine during an infection and the infection symptoms persist or worsen, they should immediately consult a doctor.
Skin reactions
Severe skin reactions have been reported with I F P use.
If any of the following occur: any skin rash, mucosal lesions, blisters, or other signs of allergy, I F P should be discontinued, and medical help should be sought immediately, as these may be the first signs of a very severe skin reaction. See section 4.
In elderly patients, there is an increased risk of adverse reactions during NSAID use, particularly those affecting the stomach and intestines.
Patients who have previously experienced adverse reactions in the gastrointestinal tract, especially elderly patients, should report any unusual abdominal symptoms (especially gastrointestinal bleeding), especially during the initial treatment phase.
Children and adolescents
In infants under 6 months old, the medicine can only be given after consulting a doctor.
In dehydrated children and adolescents, there is a risk of kidney function disorders.
I F P and other medicines
The patient should tell their doctor or pharmacist about all medicines they are currently taking or have recently taken, as well as any medicines they plan to take.
In particular, the patient should inform their doctor or pharmacist if they are taking:
- corticosteroids (e.g., prednisolone), as they may increase the risk of gastrointestinal ulceration or bleeding,
- other NSAIDs,
- antiplatelet agents (such as acetylsalicylic acid) and selective serotonin reuptake inhibitors (antidepressants), as they increase the risk of gastrointestinal side effects,
- blood pressure medicines and diuretics, as NSAIDs may reduce their effect and increase the risk of kidney damage. In such cases, it is essential for the child to drink plenty of fluids during the day,
- lithium (a medicine used in depression), as lithium levels may increase,
- methotrexate (a medicine used in cancer or rheumatic diseases), as methotrexate levels may increase,
- tacrolimus (an immunosuppressive medicine), as there is an increased risk of toxic effects on the kidneys,
- cyclosporin (an immunosuppressive medicine), as there are limited data on increased risk of toxic effects on the kidneys,
- zydovudine (a medicine used in AIDS treatment), as I F P use may increase the risk of bleeding into joints or bleeding leading to swelling (in patients with hemophilia and positive HIV antibody test),
- sulfonylurea derivatives (oral antidiabetic medicines): there may be clinical interactions between these medicines and NSAIDs. Blood glucose monitoring is recommended;
- probenecid and sulfinpyrazone (medicines used in gout treatment): they may delay ibuprofen excretion,
- digitalis glycosides, phenytoin, and lithium: ibuprofen may increase their plasma levels,
- quinolone antibiotics: they may increase the risk of seizures,
- cholestyramine: it may delay and reduce the absorption of NSAIDs,
- voriconazole and fluconazole (antifungal medicines): they may increase NSAID exposure,
- baclofen (a muscle relaxant): toxic effects of baclofen may occur after starting ibuprofen,
- ritonavir (a medicine used in HIV therapy): ritonavir may increase NSAID plasma levels,
- aminoglycosides (a type of antibiotic): NSAIDs may decrease aminoglycoside excretion,
- mifepristone: NSAIDs should not be used within 8-12 days after mifepristone administration, as they may reduce mifepristone's effect,
- calcium channel blockers: reduced antihypertensive effect and increased risk of gastrointestinal bleeding,
- desipramine: increased desipramine toxicity, typical of tricyclic antidepressants,
- levofloxacin and ofloxacin: increased risk of serious central nervous system effects,
- thienopyridine derivatives: increased risk of bleeding due to additive anti-aggregatory and anticoagulant effects,
- bisphosphonates: increased risk of gastrointestinal side effects,
- anticoagulant medicines (i.e., blood thinners or anti-clotting agents, such as aspirin - acetylsalicylic acid, warfarin, ticlopidine),
- blood pressure-lowering medicines (ACE inhibitors, such as captopril, beta-blockers, such as atenolol, angiotensin II receptor antagonists, such as losartan). Also, some other medicines may be affected by or affect I F P treatment. Before taking I F P with other medicines, the patient should always consult their doctor or pharmacist.
Taking ibuprofen with herbal products containing Ginkgo biloba and Filipendula ulmaria may increase the risk of bleeding due to additive anti-aggregatory effects. Concurrent use of ibuprofen and products containing Ephedra sinica may increase the risk of gastrointestinal mucosa damage.
Taking I F P with food, drink, and alcohol
In patients with sensitive stomachs, it is recommended to take I F P with meals.
Food slows down the absorption of ibuprofen from the gastrointestinal tract.
When taking high doses of ibuprofen and consuming alcohol, symptoms such as fatigue and headaches may occur.
Pregnancy, breastfeeding, and fertility
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a baby, they should consult their doctor or pharmacist before taking this medicine.
Pregnancy
I F P should not be taken if the patient is in the last 3 months of pregnancy, as it may harm the unborn child or cause complications during delivery.
It may cause kidney and heart problems in the unborn child.
It may increase the risk of bleeding in the mother and child and cause prolongation or delay of labor.
In the first 6 months of pregnancy, the medicine should not be used unless absolutely necessary and under medical supervision. If treatment is necessary during this period or when trying to conceive, the lowest possible dose should be used for the shortest duration.
From the 20th week of pregnancy, I F P may cause kidney problems in the unborn child if taken for more than a few days, which may lead to reduced amniotic fluid or narrowing of the fetal artery.
If treatment is necessary for a longer period, the doctor may recommend additional monitoring.
Breastfeeding
Ibuprofen passes into breast milk in small amounts. With short-term use of ibuprofen in recommended doses, harmful effects on breastfed infants seem unlikely.
Fertility
Ibuprofen may make it more difficult to become pregnant. If the patient plans to become pregnant or is having trouble becoming pregnant, they should inform their doctor.
Driving and using machines
Short-term use of the medicine has no or negligible influence on the ability to drive and use machines.
If symptoms such as vision disturbances, fatigue, dizziness, or other nervous system side effects occur, driving and operating machinery are not recommended.
I F P contains maltitol
If the patient has previously been diagnosed with intolerance to some sugars, they should consult their doctor before taking the medicine.
I F P contains 3.357 mg of sodium benzoate in 5 ml of suspension.
3. How to take I F P
This medicine should always be used exactly as described in the patient leaflet or as directed by a doctor or pharmacist.
In case of doubt, the patient should consult their doctor or pharmacist.
The medicine is for oral use. An oral syringe is included with the packaging.
Before use, the bottle should be shaken vigorously.
The daily dose of I F P strictly depends on the patient's body weight and is 20-30 mg/kg, in divided doses, according to the following table:
| Child's age (child's weight) | Single dose | Maximum daily dose |
| 3-6 months (5-7.6 kg) | 1.25 ml (50 mg) | 3 times 1.25 ml = 150 mg |
| 6-12 months (7.7-9 kg) 1-3 years (10-15 kg) 4-6 years (16-20 kg) 7-9 years (21-29 kg) 10-12 years (30-40 kg) over 40 kg | 1.25 ml (50 mg) 2.5 ml (100 mg) 3.75 ml (150 mg) 5 ml (200 mg) 7.5 ml (300 mg) 7.5-10 ml (300-400 mg) | 3-4 times 1.25 ml = 150-200 mg 3 times 2.5 ml = 300 mg 3 times 3.75 ml = 450 mg 3 times 5 ml = 600 mg 3 times 7.5 ml = 900 mg 3-4 times 7.5 ml = 900-1200 mg |
In infants under 6 months old, the medicine can only be given after consulting a doctor.
The medicine should be given at intervals of at least 6 hours.
A higher dose of the medicine than recommended should not be used.
The smallest effective dose should be used for the shortest duration necessary to relieve symptoms.
If the symptoms of infection (such as fever and pain) persist or worsen during the infection, the patient should immediately consult a doctor (see section 2).
I F P does not contain aromas, dyes, or sugar.
Information for diabetic patients: 5 ml of I F P suspension contains approximately 1119.00 mg of maltitol, which corresponds to approximately 0.07 carbohydrate units.
Information for patients with allergies: it does not contain aromas or dyes.
Duration of use
I F P is intended for short-term use.
If after 1 day (infants 3-5 months old) or 3 days (children over 6 months old, adolescents, and adults) there is no improvement or the patient feels worse, they should contact a doctor.
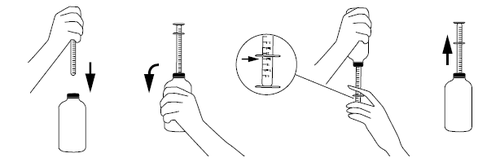
Dosing instructions using the oral syringe:
- before the first use of the syringe, it must be washed in warm (not boiling) water with a detergent,
- after opening the bottle, the oral syringe should be placed on the cork in the bottle neck,
- to fill the oral syringe, the bottle should be shaken vigorously, turned upside down, and the syringe plunger should be slowly pushed down, drawing the suspension to the desired volume marked on the scale,
- to accurately measure the dose, the collar of the oral syringe should be set to the scale mark on the plunger,
- the bottle should be turned right side up, and the oral syringe should be carefully removed from the cork (as shown in the picture),
- the tip of the oral syringe should be placed in the child's mouth, and then, slowly pressing the plunger, the contents should be carefully emptied (the child should be held upright or sitting),
- after use, the bottle should be closed, and the oral syringe should be washed in warm (not boiling) water with a detergent and dried.
Taking a higher dose of I F P than recommended
If the patient has taken a higher dose of I F P than recommended or if a child has accidentally taken the medicine, they should always consult a doctor or go to the nearest hospital to get an opinion on possible health risks and advice on what to do.
Symptoms may include nausea, stomach pain, vomiting (which may contain blood), headaches, ringing in the ears, disorientation, and nystagmus. After taking a large dose, drowsiness, chest pain, palpitations, loss of consciousness, seizures (mainly in children), weakness, and dizziness may occur, as well as blood in the urine, feeling cold, and breathing difficulties.
Missing a dose of I F P
A double dose should not be taken to make up for a missed dose.
If the patient has any further doubts about taking this medicine, they should consult their doctor or pharmacist.
4. Possible side effects
Like all medicines, I F P can cause side effects, although not everybody gets them.
The risk of side effects can be minimized by using the smallest effective dose for the shortest duration necessary to relieve symptoms.
If side effects occur or in case of doubts, the patient should stop taking the medicine and talk to their doctor as soon as possible.
Elderly patients taking this medicine are at increased risk of adverse reactions.
The patient should stop taking I F P and immediately consult a doctor if they experience:
- symptoms of gastrointestinal bleeding, such as severe stomach pain, black stools, vomiting blood or coffee ground-like particles;
- symptoms of rare but severe allergic reactions, such as worsening of asthma, unexplained wheezing or shortness of breath, swelling of the face, tongue, or throat, difficulty breathing, rapid heartbeat, or a drop in blood pressure leading to shock. Symptoms may occur even after the first dose. If any of these symptoms occur, the patient should immediately contact a doctor;
- symptoms of severe skin reactions, such as:
- red, non-raised, target-like, or circular patches on the torso, often with blisters in the center, peeling skin, ulcers in the mouth, throat, nose, genitals, and eyes. These severe skin rashes may be preceded by fever and flu-like symptoms (exfoliative dermatitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis);
- widespread rash, high fever, and swollen lymph nodes (DRESS syndrome);
- red, scaly rash with bumps under the skin and blisters, usually in skin folds, on the torso, and upper limbs, with fever occurring at the beginning of treatment (acute generalized exanthematous pustulosis).
Other possible side effects include:
Frequent(occurring in 1 to 10 patients in 100):
- heartburn, stomach pain, nausea, vomiting, bloating with gas, diarrhea, constipation.
Uncommon(occurring in 1 to 10 patients in 1,000):
- gastritis, colitis, and exacerbation of Crohn's disease (inflammatory bowel disease);
- headaches, dizziness, insomnia, restlessness, or fatigue;
- vision disturbances;
- stomach ulcers, which may bleed or perforate;
- mouth ulcers and/or swelling and irritation of the mouth;
- allergic reactions with rash and itching, asthma attacks (with possible drop in blood pressure).
Rare(occurring in 1 to 10 patients in 10,000):
- tinnitus (ringing in the ears).
Very rare(occurring in less than 1 patient in 10,000):
- esophagitis or pancreatitis, intestinal obstruction;
- severe skin reactions, including rash with redness and blisters, which may peel and be accompanied by fever and flu-like symptoms (exfoliative dermatitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis). In rare cases, severe skin infections have occurred during chickenpox;
- reduced urine output and swelling (possible acute kidney failure or kidney inflammation). Kidney damage or increased urea levels in the blood (first symptoms are reduced urine output, cloudy urine, blood in the urine, back pain, possible swelling of the legs and general malaise);
- blood disorders (first symptoms are fever, sore throat, superficial mouth ulcers, flu-like symptoms, severe fatigue, nosebleeds, and unexplained bruising);
- psychotic reactions and depression;
- worsening of infection due to masking of symptoms. If infection symptoms occur or worsen during I F P use, the patient should consult a doctor;
- swelling, high blood pressure, palpitations, heart failure, heart attack;
- liver function disorders or hepatitis. Liver failure or damage, especially during long-term use, manifested by yellowing of the skin and eyes or pale stools and dark urine;
- symptoms of aseptic meningitis with neck stiffness, headaches, malaise, or changes in consciousness. Patients with autoimmune diseases (systemic lupus erythematosus, mixed connective tissue disease) are more prone to adverse reactions. The patient should immediately consult a doctor if these symptoms occur.
Frequency not known(frequency cannot be estimated from available data):
- chest pain, which may be a sign of a potentially severe allergic reaction known as Kounis syndrome;
- severe skin reactions known as DRESS syndrome. Symptoms of DRESS syndrome include skin rash, fever, swollen lymph nodes, and increased eosinophil count (a type of white blood cell);
- red, scaly rash with bumps under the skin and blisters, usually in skin folds, on the torso and upper limbs, with fever occurring at the beginning of treatment (acute generalized exanthematous pustulosis). If such symptoms occur, the patient should stop taking I F P and seek medical help immediately. See also section 2;
- skin becomes sensitive to light.
Taking medicines like I F P may be associated with a small increased risk of heart attack (myocardial infarction) or stroke.
Reporting side effects
If the patient experiences any side effects, including any possible side effects not listed in this leaflet, they should tell their doctor or pharmacist, or nurse.
Side effects can be reported directly to the Department of Drug Safety Monitoring of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products:
Aleje Jerozolimskie 181C, 02-222 Warsaw,
phone: +48 22 49 21 301, fax: +48 22 49 21 309,
website: https://smz.ezdrowie.gov.pl
Side effects can also be reported to the marketing authorization holder.
By reporting side effects, more information can be collected on the safety of this medicine.
5. How to store I F P
There are no special precautions for storage of the medicinal product.
Shelf life after first opening of the immediate packaging: 12 months.
The medicine should be stored out of sight and reach of children.
This medicine should not be used after the expiry date stated on the packaging. The expiry date refers to the last day of the month stated.
Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines no longer required. This will help protect the environment.
6. Contents of the packaging and other information
What I F P contains
- The active substance of I F P is ibuprofen. 5 ml of suspension contains 200 mg of ibuprofen.
- Other ingredients (excipients) are: liquid maltitol (E 965), glycerol (E 422), xanthan gum, sodium saccharin (E 954), sodium benzoate (E 211), fumaric acid, disodium phosphate dodecahydrate, purified water.
What I F P looks like and contents of the pack
The medicine is a white suspension.
The packaging consists of a type III glass bottle, brown in color, with a capacity of 100 mL, closed with a PE cap and a tamper-evident closure, containing 100 g of oral suspension, in a cardboard box. An oral syringe is included with the packaging.
Marketing authorization holder and manufacturer
"PRZEDSIĘBIORSTWO PRODUKCJI FARMACEUTYCZNEJ HASCO-LEK" S.A.
51-131 Wrocław, ul. Żmigrodzka 242 E
Information about the medicine
phone: 22 742 00 22
e-mail: [email protected]
Date of last revision of the leaflet:
- Country of registration
- Active substance
- Prescription requiredNo
- Manufacturer
- ImporterPrzedsiębiorstwo Produkcji Farmaceutycznej HASCO-LEK S.A.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Ibum Forte PureDosage form: Suspension, 40 mg/mlActive substance: ibuprofenManufacturer: Laboratorios Basi - Industria Farmaceutica, S.A.Prescription not requiredDosage form: Tablets, 400 mgActive substance: ibuprofenPrescription not requiredDosage form: Tablets, 600 mgActive substance: ibuprofenManufacturer: Aristo Pharma GmbHPrescription required
Alternatives to Ibum Forte Pure in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Ibum Forte Pure in Spain
Alternative to Ibum Forte Pure in Ukraine
Online doctors for Ibum Forte Pure
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Ibum Forte Pure – subject to medical assessment and local rules.















