How to use Fingolimod Reddi
Leaflet accompanying the packaging: information for the user
Fingolimod Reddy, 0.5 mg, hard capsules
Fingolimodum
Read the leaflet carefully before taking the medicine, as it contains important information for the patient.
- Keep this leaflet, so you can read it again if you need to.
- If you have any doubts, consult your doctor or pharmacist.
- This medicine has been prescribed specifically for you. Do not pass it on to others. The medicine may harm another person, even if their symptoms are the same.
- If the patient experiences any side effects, including any possible side effects not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet:
- 1. What is Fingolimod Reddy and what is it used for
- 2. Important information before taking Fingolimod Reddy
- 3. How to take Fingolimod Reddy
- 4. Possible side effects
- 5. How to store Fingolimod Reddy
- 6. Contents of the pack and other information
1. What is Fingolimod Reddy and what is it used for
What is Fingolimod Reddy
Fingolimod Reddy contains the active substance fingolimod.
What is Fingolimod Reddy used for
Fingolimod Reddy is used in adults and children and adolescents (aged 10 years and older) to treat relapsing-remitting multiple sclerosis (MS), particularly in:
- patients who have not responded to MS treatment or
- patients who have rapidly evolving, severe MS.
Fingolimod Reddy does not cure MS, but it helps reduce the number of relapses and slows down the progression of disability caused by MS.
What is multiple sclerosis
MS is a chronic disease of the central nervous system (CNS), consisting of the brain and spinal cord. In MS, the inflammatory process destroys the nerve sheath (called myelin) in the CNS, preventing it from functioning properly. This phenomenon is called demyelination.
How Fingolimod Reddy works
Fingolimod helps protect the CNS from immune system attacks by reducing the ability of certain white blood cells (lymphocytes) to move freely in the patient's body and preventing them from entering the brain and spinal cord. In this way, the medicine reduces nerve damage caused by MS. Fingolimod also weakens some immune responses of the body.
2. Important information before taking Fingolimod Reddy
When not to take Fingolimod Reddy
- if the patient is allergic to fingolimod or any of the other ingredients of this medicine (listed in section 6).
- if the patient has a reduced immune response (due to immunodeficiency syndrome, disease, or taking medicines that suppress the immune system);
- if the patient has a severe active infection or chronic active infection, such as hepatitis or tuberculosis;
- if the patient has an active malignant disease;
- if the patient has severe liver disease;
- if the patient has had a heart attack, angina pectoris, stroke, or symptoms of stroke within the last 6 months;
- if the patient has a certain type of irregular or abnormal heartbeat (arrhythmia), which includes patients who have had an electrocardiogram (ECG) showing a prolonged QT interval before starting treatment with fingolimod;
- if the patient is currently taking or has recently taken medicines for irregular heartbeat, such as quinidine, disopyramide, amiodarone, or sotalol;
- if the patient is pregnant or breastfeeding or is of childbearing age and not using effective contraception. If this situation occurs or the patient has doubts, they should consult their doctor before taking Fingolimod Reddy.
Warnings and precautions
Before starting treatment with Fingolimod Reddy, the patient should discuss the following with their doctor:
- if the patient has severe respiratory disorders during sleep (sleep apnea);
- if the patient has been informed that their ECG is abnormal;
- if the patient has symptoms of slow heart rate (e.g., dizziness, nausea, or palpitations);
- if the patient is taking or has recently taken medicines that slow down the heart rate(such as beta blockers, verapamil, diltiazem, or ivabradine, digoxin, cholinesterase inhibitors, or pilocarpine);
- if the patient has had sudden loss of consciousness or fainting in the past;
- if the patient plans to be vaccinated;
- if the patient has never had chickenpox;
- if the patient has or has had vision problemsor other symptoms of macular edema (a condition where the macula, the part of the eye responsible for central vision, becomes swollen) or uveitis (inflammation of the uvea, the middle layer of the eye), or if the patient has diabetes, which can cause vision problems;
- if the patient has liver disease;
- if the patient has high blood pressure that cannot be controlled with medication;
- if the patient has severe lung disease or a cough typical of smokers. If any of these situations occur or the patient has doubts, they should consult their doctor before taking Fingolimod Reddy.Low heart rate (bradycardia) and irregular heartbeat On starting treatment or after the first dose of 0.5 mg, fingolimod slows down the heart rate. As a result, the patient may feel dizzy, tired, or have palpitations or low blood pressure. If these symptoms are severe, the patient should inform their doctor immediately, as they may require immediate treatment.Fingolimod may also cause irregular heartbeat, especially after the first dose. Irregular heartbeat usually returns to normal within less than one day. Low heart rate usually returns to normal within one month. During this period, no clinically significant effect on heart rate is expected.
The doctor will ask the patient to stay in the doctor's office or clinic for at least 6 hours after taking the first dose of fingolimod or after the first dose of 0.5 mg if the treatment is changed from a daily dose of 0.25 mg, with hourly measurements of pulse and blood pressure, so that if any side effects occur at the start of treatment, appropriate treatment can be given. Before the first dose of fingolimod and after the 6-hour observation period, the patient will have an ECG. During this time, the doctor may continuously monitor the patient's heart activity using an electrocardiogram. If after 6 hours of observation, the patient has a very slow or decreasing heart rate or if the ECG shows abnormalities, there may be a need for longer monitoring of the patient's condition (for at least 2 hours longer or possibly until the next day), until these symptoms resolve. The same procedure may be recommended if the patient resumes treatment with fingolimod after a break in treatment, depending on how long the break lasted and how long the patient took fingolimod before the break. If the patient has irregular or abnormal heartbeat, or risk factors for these events, or abnormal ECG or heart disease, or heart failure, fingolimod may not be suitable for them. If the patient has a history of sudden loss of consciousness or slow heart rate, fingolimod may not be suitable for them. The patient may need to consult a cardiologist (a heart specialist) who will advise on how to start treatment with fingolimod, including how to monitor the patient at night. If the patient is taking medicines that can slow down the heart rate, fingolimod may not be suitable. The patient may need to consult a cardiologist who will check if the patient can switch to other medicines that do not slow down the heart rate, to allow treatment with Fingolimod Reddy. If such a change in treatment is not possible, the cardiologist will advise the patient on how to start treatment with fingolimod, taking into account monitoring until the next day after administration of the first dose of fingolimod. Patients who have never had chickenpox If the patient has never had chickenpox, the doctor will check the patient's immunity to the varicella-zoster virus. If the patient is not protected against the virus, they may need to be vaccinated before starting treatment with fingolimod. If this situation occurs, the doctor will delay the start of treatment with Fingolimod Reddy for one month after the full vaccination course. Infections Fingolimod reduces the number of white blood cells (especially lymphocytes). White blood cells fight infections. While taking fingolimod (and for 2 months after stopping treatment), the patient may be more prone to infections. Any existing infections may worsen. Infections can be severe and life-threatening. If the patient thinks they have an infection, have a fever, feel flu-like symptoms, have shingles, or have a headache with stiff neck, sensitivity to light, nausea, and (or) confusion or seizures (which may be symptoms of meningitis and (or) encephalitis caused by fungal or viral infections), they should contact their doctor immediately, as this condition can be severe. If the patient experiences any of the above symptoms after starting treatment with fingolimod, they should inform their doctor immediately. Before, during, and after treatment, the doctor will order blood tests to monitor liver function. If the test results indicate liver function disorders, treatment with fingolimod may be discontinued. High blood pressure The doctor may regularly check the patient's blood pressure, as fingolimod can cause a slight increase in blood pressure. Lung disease Fingolimod has a minor effect on lung function. Patients with severe lung disease or a cough typical of smokers are at greater risk of side effects. Blood cell count The expected effect of fingolimod is a decrease in the number of white blood cells in the blood. Their number usually returns to normal within 2 months after stopping treatment. If blood tests need to be performed, the patient should inform their doctor that they are taking fingolimod. Otherwise, the doctor may not be able to interpret the test results, and in the case of certain tests, the doctor may order more blood to be drawn than usual. Before starting treatment with fingolimod, the doctor will check if the patient has a sufficient number of white blood cells in the blood to start treatment and may order regular blood tests. If there are not enough white blood cells, it may be necessary to discontinue treatment with fingolimod. Reversible posterior encephalopathy syndrome (PRES) In patients with MS treated with fingolimod, there have been rare reports of a condition called reversible posterior encephalopathy syndrome (PRES). The symptoms of this condition may include severe headache, confusion, seizures, and (or) vision changes. If the patient experiences any of these symptoms while taking fingolimod, they should inform their doctor immediately, as this condition can be severe. Cancer In patients with MS treated with fingolimod, there have been reports of skin cancers. If the patient notices any lumps on their skin (e.g., shiny lumps with a pearl-like color), spots, or open sores that do not heal within a few weeks, they should inform their doctor immediately. Symptoms of skin cancer may include abnormal growths or changes in skin tissue (e.g., new moles) that change color, shape, or size over time. Before starting treatment with fingolimod, it is necessary to examine the patient's skin for any lumps. The treating doctor will also perform regular skin checks during treatment with fingolimod. If skin problems occur, the treating doctor may refer the patient to a dermatologist, who may decide on the need for regular visits after consulting with them. Exposure to sunlight and protection against ultraviolet radiation Fingolimod weakens the immune system. This increases the risk of developing malignant tumors, especially skin cancers. The patient should limit their exposure to sunlight and ultraviolet radiation by:
- wearing protective clothing.
- regularly applying sunscreen with a high level of protection against ultraviolet radiation.
Unusual changes in the brain associated with MS relapse In patients treated with fingolimod, there have been rare reports of unusually large changes in the brain associated with MS relapse. In the case of a severe MS relapse, the treating doctor will consider performing an MRI to assess this condition and decide on the possible need to discontinue treatment with fingolimod. Changing treatment from other medicines to fingolimod The doctor may change treatment directly from interferon beta, glatiramer acetate, or dimethyl fumarate to Fingolimod Reddy if there are no symptoms of abnormalities caused by previous treatment. The doctor may order a blood test to rule out these abnormalities. After stopping treatment with natalizumab, it may be necessary to wait 2 to 3 months before starting treatment with fingolimod. When changing treatment from teriflunomide, the doctor may advise the patient to wait for some time or undergo an accelerated elimination procedure for the medicine. Patients previously treated with alemtuzumab require careful evaluation and discussion with their doctor before deciding whether fingolimod is suitable for them. Women of childbearing age If fingolimod is used during pregnancy, it may harm the unborn child. Before starting treatment with fingolimod, the doctor will inform the patient about the risk and ask them to perform a pregnancy test to ensure they are not pregnant and
the patient must use effective contraception during treatment with fingolimod and for 2 months after stopping treatmentto avoid becoming pregnant. The patient should discuss effective contraception methods with their doctor. The doctor will give the patient a card explaining why they should not become pregnant while taking fingolimod.
If the patient becomes pregnant while taking fingolimod, they should inform their doctor immediately.
The doctor will decide whether to discontinue treatment(see "Discontinuing Fingolimod Reddy" in section 3 and section 4 "Possible side effects"). The patient will also need to undergo prenatal check-ups. Breastfeeding Do not breastfeed while taking fingolimod. Fingolimod may pass into breast milk, posing a risk of severe side effects to the baby.
Driving and using machines
The doctor will inform the patient whether their condition allows them to drive vehicles safely, including cycling and operating machinery. It is not expected that fingolimod will affect the ability to drive vehicles and operate machinery. However, at the start of treatment, the patient must stay in the doctor's office or clinic for 6 hours after taking the first dose of fingolimod. During this time and potentially after it, the ability to drive vehicles and operate machinery may be impaired.
Fingolimod Reddy contains sodium.
The medicine contains less than 1 mmol (23 mg) of sodium per capsule, which means it is essentially "sodium-free".
3. How to take Fingolimod Reddy
Treatment with fingolimod will be supervised by a doctor with experience in treating multiple sclerosis. This medicine should always be taken exactly as prescribed by the doctor. If the patient has any doubts, they should consult their doctor. The recommended dose is:
Adults:
The dose is one 0.5 mg capsule per day.
Children and adolescents (aged 10 years and older):
The dose depends on body weight:
- children and adolescents with a body weight of 40 kg or less: one 0.25 mg capsule per day. Fingolimod Reddy 0.5 mg hard capsules are not suitable for children with a body weight of 40 kg or less. Other medicines containing fingolimod are available in lower strengths (0.25 mg capsules).
- children and adolescents with a body weight over 40 kg: one 0.5 mg capsule per day.
Children and adolescents starting treatment with one 0.25 mg capsule per day and later reaching a stable body weight over 40 kg will be advised by their doctor to switch to one 0.5 mg capsule per day. In this case, it is recommended to repeat the observation period as after the first dose of the medicine. Do not exceed the recommended dose. Fingolimod Reddy is intended for oral use. Fingolimod Reddy should be taken once a day, with a glass of water. Fingolimod Reddy capsules should always be swallowed whole, without opening. Fingolimod Reddy can be taken with or without food. Taking Fingolimod Reddy at the same time every day will help the patient remember to take their medicine. If the patient has any questions about the duration of treatment with Fingolimod Reddy, they should consult their doctor or pharmacist.
Taking a higher dose of Fingolimod Reddy than recommended
If the patient has taken too much of the medicine, they should contact their doctor immediately.
Missing a dose of Fingolimod Reddy
If the patient has been taking fingolimod for less than 1 month and has missed a dose for the whole day, they should contact their doctor before taking the next dose. The doctor may decide to keep the patient under observation during the next dose. If the patient has been taking fingolimod for at least 1 month and has missed taking the medicine for more than 2 weeks, they should contact their doctor before taking the next dose. The doctor may decide to keep the patient under observation during the next dose. However, if the patient has missed taking the medicine for up to 2 weeks, they can take the next dose as planned. Do not take a double dose to make up for a missed dose.
Discontinuing Fingolimod Reddy
Do not stop taking Fingolimod Reddy or change the dose without consulting the doctor first. Fingolimod remains in the body for up to 2 months after stopping treatment. During this time, the number of white blood cells (lymphocytes) may also be reduced, and side effects described in this leaflet may still occur. After stopping treatment with fingolimod, the patient should wait 6-8 weeks before starting new MS treatment. In patients resuming treatment with fingolimod after a break of more than 2 weeks, the effect on heart rate observed after the first dose may recur, and monitoring of the patient's condition in the doctor's office or clinic will be necessary due to the restart of treatment. Do not resume treatment with fingolimod after a break of more than 2 weeks without consulting the treating doctor. The treating doctor will decide whether and how to monitor the patient after stopping treatment with fingolimod. If the patient thinks their MS is getting worse after stopping treatment with fingolimod, they should inform their doctor immediately. This situation can be serious. If the patient has any further doubts about using this medicine, they should consult their doctor or pharmacist.
4. Possible side effects
Like all medicines, Fingolimod Reddy can cause side effects, although not everybody gets them. Some side effects may be serious or become serious
Common(may affect up to 1 in 10 people):
- cough with expectoration, unspecified unpleasant feeling in the chest, fever (symptoms of respiratory disorders)
- herpesvirus infections (shingles or herpes) with symptoms such as blisters, burning, itching, or pain on the skin, usually on the upper body or face. Other symptoms may include fever and weakness at the onset of infection, followed by numbness, itching, or red spots with severe pain
- slow heart rate (bradycardia), irregular heartbeat
- a type of skin cancer called basal cell carcinoma (BCC), which often appears as a pearl-like nodule, although it can have other appearances
- it is known that depression and anxiety occur more frequently in the population of patients with MS and have also been reported in children and adolescents treated with fingolimod.
- weight loss.
Uncommon(may affect up to 1 in 100 people):
- pneumonia with symptoms such as fever, cough, difficulty breathing
- macular edema (swelling in the center of the field of vision in the retina, at the back of the eye) with symptoms such as shadows or blind spots in the center of the field of vision, blurred vision, difficulty perceiving colors and details
- reduced platelet count, which increases the risk of bleeding or bruising
- malignant melanoma (a type of skin cancer that usually develops from an unusual mole). Possible symptoms of melanoma include moles whose size, shape, elevation, or color changes over time or new moles that appear. Moles can be itchy, bleed, or ulcerate
- seizures, epileptic fits (more common in children and adolescents than in adults)
Rare(may affect up to 1 in 1,000 people):
- a condition called posterior reversible encephalopathy syndrome (PRES). Symptoms may include severe headache, confusion, seizures, and (or) vision changes
- lymphoma (a type of cancer affecting the lymphatic system)
- squamous cell carcinoma: a type of skin cancer that can appear as a hard, red nodule, covered with a scab, or a fresh ulcer in the place of an existing scar
Very rare(may affect up to 1 in 10,000 people):
- abnormalities in the ECG recording (T-wave inversion)
- a tumor associated with human herpesvirus 8 (Kaposi's sarcoma)
Frequency not known(frequency cannot be estimated from the available data):
- allergic reactions, including symptoms such as rash or itchy hives, swelling of the lips, tongue, or face, which are more likely to occur on the day of starting treatment with fingolimod
- liver disease symptoms (including liver failure) such as yellowing of the skin or whites of the eyes (jaundice), nausea or vomiting, pain in the right upper abdomen, dark (brown) urine, decreased appetite, fatigue, and abnormal liver function test results. In very rare cases, liver failure can lead to liver transplantation.
- risk of a rare brain infection called progressive multifocal leukoencephalopathy (PML). Symptoms of PML may be similar to those of an MS relapse. They may also include symptoms that the patient is not aware of, such as changes in mood or behavior, transient memory lapses, difficulty speaking or communicating, which the doctor should evaluate to rule out PML. Therefore, if the patient thinks their MS is getting worse or if the patient or their relatives notice any new or unusual symptoms, it is very important to inform their doctor as soon as possible
- fungal infections (cryptococcal infections), including cryptococcal meningitis, with symptoms such as headache, stiff neck, sensitivity to light, nausea, and (or) confusion
- cancer of the Merkel cells (a type of skin cancer). Possible symptoms of Merkel cell carcinoma include a painless nodule with a raw meat or blue-red color, usually located on the face, head, or neck. Merkel cell carcinoma can also appear as a hard, painless nodule or mass. Prolonged sun exposure and weakened immune system can affect the risk of developing Merkel cell carcinoma
- after stopping treatment with fingolimod, MS symptoms may recur and worsen compared to the period before treatment and during treatment.
- autoimmune hemolytic anemia (a condition where red blood cells are destroyed).
If the patient experiences any of these side effects, they should inform their doctor immediately. Other side effects
Very common(may affect more than 1 in 10 people):
- flu-like infection with symptoms such as fatigue, chills, sore throat, joint or muscle pain, fever
- feeling of pressure or pain in the cheeks and forehead (sinusitis)
- headache
- diarrhea
- back pain
- increased liver enzyme activity in blood tests
- cough
Common(may affect up to 1 in 10 people):
- fungal skin infections (dermatophyte infections) (ringworm)
- dizziness
- severe headache, usually accompanied by nausea, vomiting, and sensitivity to light (migraine symptoms)
- low white blood cell count (lymphocytes, leukocytes)
- weakness
- itchy, red, burning rash (rash)
- itching
- increased triglyceride levels in the blood
- hair loss
- shortness of breath
- depression
- blurred vision (see also the section on macular edema under "Some side effects may be or become serious")
- high blood pressure (fingolimod may cause a mild increase in blood pressure)
- muscle pain
- joint pain
Uncommon(may affect up to 1 in 100 people):
- low white blood cell count (neutrophils)
- depressive mood
- nausea
Rare(may affect up to 1 in 1,000 people):
- lymphoma (a type of cancer affecting the lymphatic system)
Frequency not known(frequency cannot be estimated from the available data):
- peripheral edema
If any of these symptoms occur with a high intensity, the patient should inform their doctor. Reporting side effects If side effects occur, including any side effects not listed in this leaflet, the patient should inform their doctor or pharmacist. Side effects can be reported directly to the Department of Drug Safety Monitoring of the Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products: Al. Jerozolimskie 181C, 02-222 Warsaw, phone: +48 22 49-21-301, fax: +48 22 49-21-309, website: https://smz.ezdrowie.gov.pl. Side effects can also be reported to the marketing authorization holder. By reporting side effects, more information can be collected on the safety of the medicine.
5. How to store Fingolimod Reddy
Keep the medicine out of the sight and reach of children. Do not use this medicine after the expiry date stated on the carton and blister after "Expiry date" / "EXP". The expiry date refers to the last day of the month stated. There are no special precautions for storing the medicine. Do not use this medicine if the packaging is damaged or shows signs of opening. Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Contents of the pack and other information
What Fingolimod Reddy contains
The active substance of the medicinal product is fingolimod.
Each capsule contains 0.5 mg of fingolimod (as fingolimod hydrochloride).
The other ingredients are:
Capsule filling: betacyclodextrin, magnesium stearate.
Capsule shell: yellow iron oxide (E172), titanium dioxide (E171), gelatin, sodium lauryl sulfate.
Printing ink: shellac, black iron oxide (E172), potassium hydroxide.
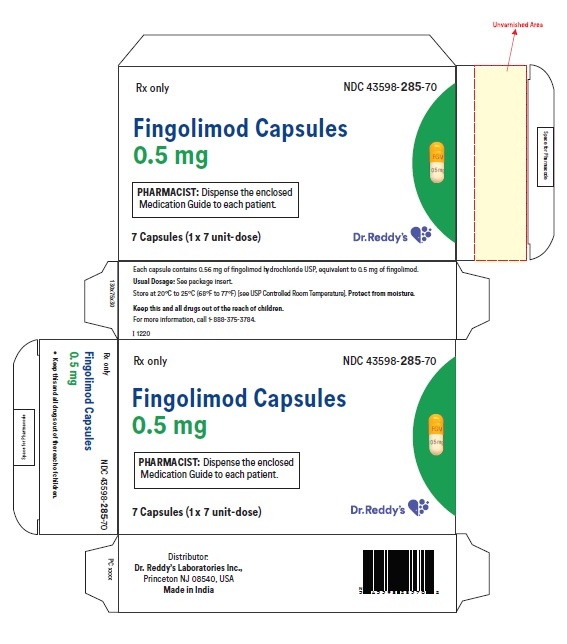
What Fingolimod Reddy looks like and what the pack contains
Fingolimod Reddy 0.5 mg hard capsules are white to off-white hard gelatin capsules,
size 3, with a dark yellow opaque cap with a black printing “FGM” and a white opaque body with a black printing “0.5 mg”.
Fingolimod Reddy 0.5 mg hard capsules are available in packs containing 28 capsules.
Marketing Authorisation Holder
Reddy Holding GmbH
Kobelweg 95
86156 Augsburg
Germany
Tel.: +49 821 74881 0
Manufacturer/Importer
betapharm Arzneimittel GmbH
Kobelweg 95
86156 Augsburg
Germany
Pharmadox Healthcare Ltd.
KW20A Kordin Industrial Park
Paola PLA 3000
Malta
Rual Laboratories SRL
Splaiul Unirii nr 313, building H, 1st floor, sector 3
030138 Bucharest
Romania
DR. REDDY'S LABORATORIES ROMANIA SRL
Daniel Danielopolu, no 30 - 32, Space 2, Floor 5, Sector 1
014134 Bucharest
Romania
This medicinal product is authorised in the Member States of the European Economic Area
under the following names:
Belgium:
Fingolimod Reddy 0.5 mg hard capsules
Denmark:
Fingolimod Reddy
Finland:
Fingolimod Reddy 0.5 mg hard capsules
Netherlands:
Fingolimod Reddy 0.5 mg hard capsules
Germany:
Fingolimod beta 0.5 mg hard capsules
Norway:
Fingolimod Reddy
Poland:
Fingolimod Reddy
Portugal:
Fingolimod Reddy 0.5 mg capsules
Czech Republic:
Fingolimod Reddy
Romania:
Fingolimod Dr. Reddy’s 0.5 mg capsules
Slovakia:
Fingolimod Reddy 0.5 mg hard capsules
Sweden:
Fingolimod Reddy 0.5 mg hard capsules
Date of last revision of the leaflet: May 2024
- Country of registration
- Active substance
- Prescription requiredYes
- ImporterBetapharm Arzneimittel GmbH Dr Reddy’s Laboratories Romania SRL Pharmadox Healthcare Ltd. Rual Laboratories SRL
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Fingolimod ReddiDosage form: Capsules, 0.5 mgActive substance: fingolimodPrescription requiredDosage form: Capsules, 0.5 mgActive substance: fingolimodPrescription not requiredDosage form: Capsules, 0.5 mgActive substance: fingolimodPrescription required
Alternatives to Fingolimod Reddi in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Fingolimod Reddi in Spain
Alternative to Fingolimod Reddi in Ukraine
Online doctors for Fingolimod Reddi
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Fingolimod Reddi – subject to medical assessment and local rules.