Doxepin Teva
Ask a doctor about a prescription for Doxepin Teva

How to use Doxepin Teva
Leaflet attached to the packaging: information for the user
Doxepin Teva 10 mg, hard capsules
Doxepin Teva, 25 mg, hard capsules
Doxepin hydrochloride
Read the leaflet carefully before taking the medicine, as it contains important information for the patient.
- Keep this leaflet, so that you can read it again if you need to.
- If you have any doubts, consult your doctor or pharmacist.
- This medicine has been prescribed to you specifically. Do not pass it on to others. The medicine may harm another person, even if their symptoms are the same as yours.
- If the patient experiences any side effects, including those not listed in this leaflet, they should tell their doctor or pharmacist. See section 4.
Table of contents of the leaflet
- 1. What is Doxepin Teva and what is it used for
- 2. Important information before taking Doxepin Teva
- 3. How to take Doxepin Teva
- 4. Possible side effects
- 5. How to store Doxepin Teva
- 6. Contents of the packaging and other information
1. What is Doxepin Teva and what is it used for
Doxepin belongs to a group of antidepressant medicines called tricyclic antidepressants. It has antidepressant and anti-anxiety effects. The mechanism of action is not fully understood.
It probably involves the inhibition of the reuptake of biogenic amines (e.g. noradrenaline) in the synaptic cleft.
The medicine is easily absorbed from the gastrointestinal tract and reaches its maximum concentration in the blood after about 2-4 hours.
The medicine is metabolized in the liver (including the formation of an active metabolite, demethylated doxepin).
Doxepin is excreted mainly in the urine, in the form of metabolites.
Indications:
- depressive states with anxiety and restlessness in the course of psychoses, including involutional depression and depressive phase in bipolar affective disorder;
- depressions and anxiety states in the course of somatic disorders and organic diseases;
- depressive-anxiety syndromes in the course of alcoholism;
- neurotic disorders with symptoms of depression or anxiety.
2. Important information before taking Doxepin Teva
When not to take Doxepin Teva
If the patient has:
- hypersensitivity to doxepin, tricyclic antidepressants or any of the other ingredients of this medicine (listed in section 6);
- mania;
- severe liver disease;
- the patient is breastfeeding;
- glaucoma;
- tendency to urinary retention;
- concomitant use of MAO inhibitors or within the last 2 weeks.
Warnings and precautions
Before starting treatment with Doxepin Teva, the patient should discuss it with their doctor or pharmacist.
Taking Doxepin Teva with buprenorphine (an opioid analgesic) may lead to serotonin syndrome, a life-threatening disease (see "Doxepin Teva and other medicines").
The doctor will use a once-daily dosing regimen with caution in patients with concomitant diseases, including those taking other medicines. This is especially important when using anticholinergic drugs.
This regimen will also be adjusted with caution in elderly patients, depending on their clinical condition. Such patients are particularly prone to side effects, such as: excitement, confusion (disorientation), orthostatic hypotension (occurring when changing position from lying or sitting to standing). The initial dose will be determined by the doctor with caution, under close control of the patient's reaction. Using half of the maintenance dose may be sufficient to achieve the desired clinical effect.
Drowsiness and increased reaction to alcohol may occur during treatment with Doxepin Teva.
If symptoms of psychosis or manic symptoms worsen, the patient should contact their doctor immediately, who may decide to reduce the dose of Doxepin Teva or add another medicine.
Although doxepin is associated with a lower risk of cardiovascular effects compared to other tricyclic antidepressants, caution is required in patients with severe cardiovascular disorders (heart block, arrhythmia, recent myocardial infarction).
Doxepin Teva should be used with caution in patients with liver and/or kidney dysfunction.
Care should be taken in patients with a history of seizures.
In patients with benign prostatic hyperplasia, the tendency to urinary retention may increase
Doxepin Teva and other medicines
The patient should tell their doctor about all medicines they are currently taking or have recently taken, as well as any medicines they plan to take.
Doxepin, like other tricyclic antidepressants, is metabolized in the liver by the cytochrome P-450 system (CYP 2D6 isoenzyme). Inhibitors or substrates of CYP2D6 (e.g. quinidine, selective serotonin reuptake inhibitors) given concomitantly may increase the concentration of tricyclic antidepressants in the blood.
When used concomitantly with other antidepressants, alcohol, or anxiolytics, the possibility of potentiation of pharmacological effects should be considered.
It is known that monoamine oxidase inhibitors can enhance the effects of other medicines and increase their side effects, so doxepin should not be given concomitantly or within 2 weeks of stopping MAO inhibitors.
Certain medicines may increase the side effects of Doxepin Teva and sometimes cause very severe reactions. While taking Doxepin Teva, the patient should not take other medicines without first consulting their doctor, especially buprenorphine. This medicine may interact with Doxepin Teva and cause symptoms such as involuntary, rhythmic muscle contractions, including those that control eye movements, excitement, hallucinations, coma, excessive sweating, tremors, increased reflexes, muscle tension, and body temperature above 38°C. If such symptoms occur, the patient should contact their doctor.
Cimetidine causes significant fluctuations in the steady-state concentration of doxepin in the blood.
Doxepin should not be given in combination with sympathomimetic medicines, such as ephedrine, isoprenaline, noradrenaline, phenylephrine, or phenylpropanolamine.
Anesthetics used during surgery and tricyclic antidepressant therapy may increase the risk of arrhythmias and hypotension or hypertension. If surgery is necessary, the anesthesiologist should be informed that the patient is currently being treated with antidepressants.
Doxepin may reduce the effect of antihypertensive medicines, such as debrisoquine, betanidine, guanethidine, and possibly clonidine. To avoid affecting the action of guanethidine, the daily dose of Doxepin Teva should not exceed 150 mg. The patient should be monitored when taking any antihypertensive medicines concomitantly.
Barbiturates may accelerate the metabolism of doxepin.
Doxepin may reduce the effect of sublingual nitroglycerin.
When used concomitantly with thyroid hormones, the doctor may recommend reducing their dose.
Doxepin Teva with food and drink
To avoid stomach irritation, it is recommended to take the medicine with food, even if it is taken once a day, in the evening.
Special precautions for certain groups of patients taking the medicine
Using Doxepin Teva in children
Doxepin Teva should not be used in children under 12 years of age, as its safety in this age group has not been established.
Using Doxepin Teva in patients with liver and/or kidney dysfunction
In patients with liver and/or kidney dysfunction, caution should be exercised, and the dose may need to be reduced.
Using Doxepin Teva in elderly patients
In elderly patients, smaller doses of Doxepin Teva are usually used.
In cases where the symptoms are mild, the doctor will recommend starting treatment with a dose of 10 mg to 50 mg per day. In most patients, a satisfactory response was achieved with doxepin at a dose of 30 mg to 50 mg per day. The doctor will adjust the dose according to the individual response of the patient.
Pregnancy and breastfeeding
If the patient is pregnant or breastfeeding, thinks they may be pregnant, or plans to have a child, they should consult their doctor or pharmacist before taking this medicine.
Pregnancy
There are no data on the safety of use in pregnant women.
Breastfeeding
Doxepin and its active metabolite, demethylated doxepin, pass into breast milk. There have been reports of apnea and drowsiness in a breastfed child whose mother was taking doxepin, so this medicine is contraindicated during breastfeeding.
Driving and using machines
Doxepin may cause drowsiness and prolong reaction time. Patients who experience such reactions should not drive or operate machinery.
Doxepin Teva contains lactose
If the patient has previously been diagnosed with intolerance to some sugars, they should contact their doctor before taking the medicine.
Doxepin Teva contains sodium
This medicine contains less than 1 mmol (23 mg) of sodium per capsule, which means it is considered "sodium-free".
3. How to take Doxepin Teva
This medicine should always be taken as directed by the doctor. If in doubt, the patient should consult their doctor or pharmacist.
Dosage depends on the severity of the disease, the patient's clinical condition, and individual response to the medicine.
The dose of doxepin is 30 mg to 300 mg per day. Doses up to 100 mg per day can be taken once or in divided doses. Doses greater than 100 mg per day should be taken in 3 divided doses. The maximum single dose is 100 mg and is usually taken before bedtime.
In cases of moderate and severe disease, the doctor will usually recommend starting treatment with a dose of 75 mg per day. The response of most patients to this dose is satisfactory. If the response is not adequate, the doctor will adjust the dose individually; in severe cases, it may be increased to a maximum dose of 300 mg per day, taken in divided doses.
After achieving the desired clinical effect, the dosage will be reduced accordingly.
Optimal antidepressant effects may not be visible for 2 to 3 weeks of treatment.
If the patient feels that the effect of the medicine is too strong or too weak, they should consult their doctor.
Taking a higher dose of Doxepin Teva than recommended
Overdose symptoms
Mild clinical condition: drowsiness, stupor, blurred vision, excessive dryness of the oral mucosa.
If such symptoms occur, the medicine should be discontinued and the patient should be monitored.
If necessary, supportive treatment should be provided.
Severe clinical condition: drowsiness, respiratory depression, hypotension, coma, seizures, cardiac arrhythmias (tachycardia), urinary retention (urinary bladder atony), decreased gastrointestinal motility (paralytic ileus), elevated or decreased body temperature, increased reflexes.
Procedure in case of poisoning: the doctor will perform gastric lavage (if the patient is conscious) and provide symptomatic and supportive treatment (treatment of arrhythmias, anticonvulsant treatment, respiratory support). Dialysis therapy and forced diuresis are not recommended.
If a higher dose of Doxepin Teva than recommended is taken, the patient should immediately consult their doctor or pharmacist.
Missing a dose of Doxepin Teva
The patient should not take a double dose to make up for a missed dose.
If a dose is missed and the medicine is taken once a day - in the evening, the missed dose should not be taken in the morning, as the medicine may affect normal functioning during the day. If a different treatment regimen is used, the missed dose should be taken as soon as possible. If the time for the next dose is approaching, the patient should wait and take it at the scheduled time.
Stopping treatment with Doxepin Teva
If the patient has any further doubts about taking this medicine, they should consult their doctor or pharmacist.
After sudden discontinuation of tricyclic antidepressants, withdrawal symptoms may occur, including: insomnia, irritability, excessive sweating. Withdrawal symptoms in newborns whose mothers took antidepressants during the third trimester of pregnancy include: respiratory distress, seizures, and increased reflexes.
4. Possible side effects
Like all medicines, Doxepin Teva can cause side effects, although not everybody gets them.
Doxepin is well tolerated. Most side effects are mild, occur usually at the beginning of treatment, and disappear during treatment or after dose reduction, if necessary.
Some side effects, listed below, have not been reported specifically for doxepin, but due to the close similarity of pharmacological properties between tricyclic antidepressants, their occurrence should be considered.
The frequency of side effects in adults found in clinical trials is as follows:
Very common (may affect more than 1 in 10 patients)
Common (may affect up to 1 in 10 patients)
Uncommon (may affect up to 1 in 100 patients)
Rare (may affect up to 1 in 1,000 patients)
Very rare (may affect up to 1 in 10,000 patients)
Frequency not known (frequency cannot be estimated from the available data).
Very common:drowsiness, dryness of the oral mucosa, constipation.
Uncommon:headaches and dizziness, insomnia, nightmares, confusion (disorientation), excitement, feeling of numbness or paresthesia (tingling, prickling), tremors (usually mild). When using high doses (especially in elderly patients), other extrapyramidal symptoms may occur, including late dyskinesias (involuntary movements of the face and/or tongue), allergic reactions, including skin rash, facial edema, photosensitivity, itching, urticaria. When using tricyclic antidepressants, asthma symptoms may worsen.
Rare:hallucinations (delusions), ataxia (lack of coordination, especially when several central nervous system-acting medicines are given), seizures (in patients with predispositions resulting from brain damage or alcohol or drug addiction). During treatment with tricyclic antidepressants, psychotic symptoms, including mania and paranoid delusions, may worsen. Rarely, tinnitus, orthostatic hypotension, facial flushing, increased sweating, and the above-mentioned allergic skin reactions have been reported; increased eosinophil count in the blood and bone marrow disorders with symptoms such as: agranulocytosis, leukopenia, thrombocytopenia, aplastic anemia, hemolytic anemia; nausea, vomiting, indigestion, taste disorders, diarrhea, anorexia, aphthous stomatitis; syndrome of inappropriate antidiuretic hormone secretion, gynecomastia in men, gynecomastia and galactorrhea in women; urinary retention (in men with a predisposition to benign prostatic hyperplasia, symptoms may worsen); jaundice.
Very rare:vision disorders (blurred vision), accelerated heart rate, changes in electrocardiogram (ECG); hair loss; fatigue, weakness, weight gain, chills, elevated body temperature (in patients taking chlorpromazine concomitantly). Single cases: decreased or increased libido, testicular edema, increased or decreased glucose levels in the blood.
Patients taking this type of medicine have been observed to have an increased risk of fractures.
Suicidal thoughts, worsening of depression or anxiety disorders
People with depression or anxiety disorders may sometimes have thoughts of self-harm or suicide. Such symptoms or behavior may worsen at the beginning of treatment with antidepressants, as these medicines usually start to work after 2 weeks, sometimes later.
The occurrence of suicidal thoughts, self-harm, or suicidal behavior is more likely if:
- the patient has had suicidal thoughts or self-harm in the past;
- the patient is a young adult; data from clinical trials indicate an increased risk of suicidal behavior in people under 25 years of age with mental disorders who were treated with antidepressants.
If the patient experiences suicidal thoughts or self-harm, they should immediately contact their doctor or go to the hospital.
It may be helpful to inform relatives or friends about depression or anxiety disorders and ask them to read this leaflet. The patient may ask their relatives or friends for help and ask them to inform them if they notice that depression or anxiety has worsened or if there are any worrying changes in behavior.
Some people taking Doxepin Teva may experience other side effects.
Reporting side effects
If side effects occur, including those not listed in this leaflet, the patient should tell their doctor or pharmacist. Side effects can be reported directly to the Department of Monitoring of Adverse Reactions to Medicinal Products, Office for Registration of Medicinal Products, Medical Devices, and Biocidal Products, Al. Jerozolimskie 181C, 02-222 Warsaw, Tel.: +48 22 49 21 301, Fax: +48 22 49 21 309, website: https://smz.ezdrowie.gov.pl. Side effects can also be reported to the marketing authorization holder.
Reporting side effects will help to gather more information on the safety of the medicine.
5. How to store Doxepin Teva
The medicine should be stored out of sight and reach of children.
Store in a temperature below 25°C. Store in the original packaging to protect from light.
Do not use this medicine after the expiry date stated on the blister and carton after: Expiry date (EXP). The expiry date refers to the last day of the month.
Medicines should not be disposed of via wastewater or household waste. The patient should ask their pharmacist how to dispose of medicines that are no longer needed. This will help protect the environment.
6. Contents of the packaging and other information
What Doxepin Teva contains
- The active substance of the medicine is 10 mg or 25 mg of doxepin in the form of doxepin hydrochloride.
- The other ingredients are: cornstarch, lactose monohydrate (see section 2 Doxepin Teva contains lactose), magnesium stearate, sodium lauryl sulfate (see section 2 Doxepin Teva contains sodium). The composition of the 10 mg hard capsule is: indigo carmine (E132), titanium dioxide (E171), gelatin, erythrosine (E127), patent blue (E131). The composition of the 25 mg hard capsule is: indigo carmine (E132), titanium dioxide (E171), gelatin, erythrosine (E127).
What Doxepin Teva looks like and contents of the packaging
Doxepin Teva, 10 mg - hard gelatin capsules, No. 4, two-colored, blue body and red cap.
Doxepin Teva, 25 mg - hard gelatin capsules, No. 4, two-colored, pink body and red cap.
The capsule filling is a white powder.
The packaging contains 30 hard capsules in 3 blisters of aluminum/PVC foil, 10 capsules per blister, in a cardboard box.
Marketing authorization holder and manufacturer
Marketing authorization holder:
Teva Pharmaceuticals Polska Sp. z o.o.
ul. Emilii Plater 53, 00-113 Warsaw
tel.: (22) 345 93 00
Manufacturer:
Teva Operations Poland Sp. z o.o.
ul. Mogilska 80
31-546 Kraków
Date of last revision of the leaflet:
- Country of registration
- Active substance
- Prescription requiredYes
- Manufacturer
- ImporterTeva Operations Polska Sp. z o.o.
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Doxepin TevaDosage form: Capsules, 25 mgActive substance: doxepinManufacturer: Teva Operations Polska Sp. z o.o.Prescription requiredDosage form: Tablets, 25 mgActive substance: amitriptylineManufacturer: Bausch Health Poland Sp. z o.o. ICN Polfa Rzeszów S.A.Prescription requiredDosage form: Tablets, 10 mgActive substance: amitriptylineManufacturer: Bausch Health Poland Sp. z o.o. ICN Polfa Rzeszów S.A.Prescription required
Alternatives to Doxepin Teva in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Doxepin Teva in Ukraine
Alternative to Doxepin Teva in Spain
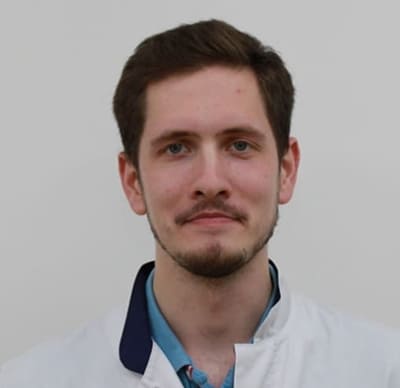
Online doctors for Doxepin Teva
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Doxepin Teva – subject to medical assessment and local rules.