How to use Adriblastina Pfs
Package Leaflet: Information for the User
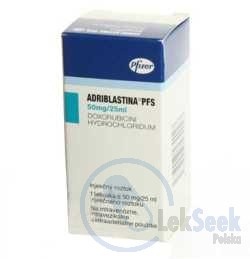
ADRIBLASTINA PFS, 2 mg/ml, Solution for Injection
Doxorubicin Hydrochloride
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
- You should keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
Contents of the pack
- 1. What ADRIBLASTINA PFS is and what it is used for
- 2. Before you are given ADRIBLASTINA PFS
- 3. How ADRIBLASTINA PFS is given
- 4. Possible side effects
- 5. How to store ADRIBLASTINA PFS
- 6. Contents of the pack and other information
1. What ADRIBLASTINA PFS is and what it is used for
ADRIABLASTINA PFS contains the active substance doxorubicin, which is a cytotoxic antibiotic belonging to the anthracycline group of anticancer agents. It may be used as a single agent or in combination with other cytotoxic agents.
ADRIABLASTINA PFS is indicated for the treatment of the following types of cancer:
- Acute lymphoblastic leukemia
- Acute myeloblastic leukemia
- Chronic leukemias
- Malignant lymphoma
- Non-Hodgkin's lymphoma
- Multiple myeloma
- Bone and soft tissue sarcomas
- Ewing's sarcoma
- Neuroblastoma
- Rhabdomyosarcoma
- Wilms' tumor
- Breast cancer
- Uterine cancer
- Ovarian cancer
- Non-seminomatous testicular cancer
- Prostate cancer
- Bladder cancer
- Lung cancer
- Stomach cancer
- Primary hepatocellular carcinoma
- Head and neck cancer
- Thyroid cancer
2. Before you are given ADRIBLASTINA PFS
When ADRIBLASTINA PFS must not be used
- In patients with hypersensitivity to doxorubicin or any of the other ingredients of this medicine (see section 6), other anthracyclines or anthracenediones,
- In patients with persistent bone marrow suppression,
- In patients with severe liver impairment,
- In patients with severe heart failure,
- In patients who have recently had a myocardial infarction,
- In patients with severe arrhythmias,
- In patients who have received maximum cumulative doses of doxorubicin, daunorubicin, epirubicin, idarubicin and/or other anthracyclines and anthracenediones.
Special warnings and precautions
Treatment with ADRIBLASTINA PFS should only be started after the acute toxic effects of any previous cytotoxic treatment have resolved. Before starting treatment with ADRIBLASTINA PFS, the patient's cardiac function should be assessed and monitored during treatment to minimize the risk of severe heart failure. The doctor should discontinue treatment at the first signs of cardiac dysfunction. Cardiac function should be assessed using the same technique throughout the observation period. Caution should be exercised when using ADRIBLASTINA PFS in patients with heart disease; with previous or concurrent radiation therapy to the mediastinum and/or pericardium; with previous treatment with other anthracyclines or anthracenediones; and concurrently with drugs that may impair cardiac contractility or cause cardiotoxicity (e.g. trastuzumab). Patients should inform their doctor if they are taking or have recently taken trastuzumab (a medicine used to treat certain types of cancer). Trastuzumab may remain in the body for up to 7 months. As trastuzumab may affect the heart, ADRIBLASTINA PFS should not be given for up to 7 months after the last dose of trastuzumab. If ADRIBLASTINA PFS is given before this time, cardiac function should be closely monitored.
Children and adolescents are particularly at risk of cardiotoxicity. In women, this risk may be greater than in men. The doctor should periodically recommend cardiac monitoring to check for these effects.
- As with other cytotoxic agents, ADRIBLASTINA PFS may cause bone marrow suppression. Before each treatment cycle with ADRIBLASTINA PFS and during each cycle, the doctor should perform blood tests, including a blood count. The main hematologic toxic effect of ADRIBLASTINA PFS is dose-dependent, reversible leukopenia (decreased white blood cell count) and/or neutropenia (decreased neutrophil count), which may require dose reduction.
- Secondary leukemia has been reported in patients treated with ADRIBLASTINA PFS.
- ADRIABLASTINA PFS may cause nausea and vomiting. Mucositis or stomatitis usually occurs soon after administration and may progress to ulcers within a few days. In most patients, this side effect resolves within the first three weeks of treatment. In patients with acute non-lymphocytic leukemia receiving combination chemotherapy with ADRIBLASTINA PFS and cytarabine given over three consecutive days, necrotizing colitis may occur, which can lead to life-threatening complications such as bleeding or infection.
- Before starting treatment with ADRIBLASTINA PFS and during treatment, the doctor should check the patient's bilirubin levels. In patients with elevated bilirubin levels, the medicine may be eliminated more slowly from the body, which may increase its overall toxic effects. In these patients, the doctor should use lower doses.
- Injection into a small vein or repeated injections into the same vein may cause vein sclerosis. Following the recommended administration procedures for ADRIBLASTINA PFS by medical personnel can help minimize the risk of phlebitis or thrombophlebitis at the injection site.
- Extravasation of ADRIBLASTINA PFS during intravenous administration may cause local pain, severe tissue damage (including blistering and severe inflammation of the subcutaneous tissue) and necrosis. If signs of extravasation occur during intravenous administration of ADRIBLASTINA PFS, the doctor should interrupt the infusion.
- ADRIABLASTINA PFS may cause hyperuricemia (elevated uric acid levels in the blood) due to the rapid breakdown of purines (nitrogenous compounds whose main metabolic product is uric acid) that accompanies the rapid destruction of cancer cells after cytostatic treatment (tumor lysis syndrome). After starting treatment, the doctor should check the patient's uric acid, potassium, phosphate, and creatinine levels.
- ADRIABLASTINA PFS may increase the toxicity of other anticancer treatments. Cyclophosphamide-induced hemorrhagic cystitis and 6-mercapto-purine-induced hepatotoxicity have been reported. Radiation-induced toxic effects (affecting the heart, mucous membranes, skin, and liver) have also been reported.
- Both men and women should use effective contraception during treatment with ADRIBLASTINA PFS and for a certain period after the end of treatment (see "Pregnancy, breastfeeding and fertility"). Patients who wish to have children after the end of treatment with doxorubicin should discuss the possibilities of preserving fertility and seek genetic counseling before starting treatment.
Children and adolescents
The doctor may consider using lower initial doses or longer intervals between cycles when using ADRIBLASTINA PFS in children.
Elderly patients
There is no need to adjust the dose in elderly patients (≥65 years). However, the doctor may consider using lower initial doses or longer intervals between cycles.
Patients with liver function disorders
ADRIABLASTINA PFS is contraindicated in patients with severe liver impairment. In patients with elevated bilirubin levels, the doctor should consider using lower doses of ADRIBLASTINA PFS.
Patients with kidney function disorders
The effect of ADRIBLASTINA PFS on kidney function has not been evaluated.
ADRIABLASTINA PFS and other medicines
Tell your doctor about all the medicines you are taking or have recently taken, as well as any medicines you plan to take. ADRIBLASTINA PFS is mainly used in combination with other cytotoxic agents. Some medicines may affect the levels of ADRIBLASTINA PFS in your body. You should inform your doctor if you are taking any of the following medicines:
- Phenobarbital - used to treat seizures and as a sedative,
- Phenytoin - used to treat seizures,
- St. John's Wort - used to treat depression and anxiety disorders,
- Cyclosporine - used to prevent transplant rejection,
- Calcium channel blockers (e.g. verapamil) - used to treat cardiovascular diseases,
- Paclitaxel - used to treat cancer,
- Sorafenib - used to treat cancer.
Pregnancy, breastfeeding and fertility
Pregnancy
If you are pregnant or breastfeeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine. You should not be given ADRIBLASTINA PFS during pregnancy. It has been shown to be toxic to the fetus.
Contraception in women of childbearing potential
You should always use effective contraception during treatment with ADRIBLASTINA PFS and for at least 6.5 months after the last dose. You should discuss with your doctor the contraceptive methods that are suitable for you and your partner.
Contraception in men
Men should always use effective contraception during treatment with ADRIBLASTINA PFS and for at least 3.5 months after the last dose.
Breastfeeding
You should not breastfeed during treatment with ADRIBLASTINA PFS and for at least 10 days after the last dose, as the medicine passes into human milk.
Fertility
In women, ADRIBLASTINA PFS may cause infertility, amenorrhea, or premature menopause. Ovulation and menstruation usually return after the end of treatment. In men, ADRIBLASTINA PFS may damage chromosomes in sperm. Oligospermia (low sperm count) and azoospermia (no sperm in the semen) may be permanent. Sperm count may return to normal within a few years after the end of treatment. Both men and women should seek advice on preserving fertility before starting treatment.
Driving and using machines
No studies on the effects of ADRIBLASTINA PFS on the ability to drive and use machines have been performed.
ADRIABLASTINA PFS contains sodium
ADRIABLASTINA PFS, 10 mg/5 ml (2 mg/ml) solution for injection, contains 17.7 mg of sodium (the main component of common salt) per 5 ml vial. This corresponds to 0.9% of the maximum recommended daily intake of sodium in the diet for adults. ADRIBLASTINA PFS, 50 mg/25 ml (2 mg/ml) solution for injection, contains 88.5 mg of sodium per 25 ml vial. This corresponds to 4.4% of the maximum recommended daily intake of sodium in the diet for adults. ADRIBLASTINA PFS, 200 mg/100 ml (2 mg/ml) solution for injection, contains 354 mg of sodium per 100 ml vial. This corresponds to 17.7% of the maximum recommended daily intake of sodium in the diet for adults.
3. How ADRIBLASTINA PFS is given
ADRIABLASTINA PFS should only be administered under the supervision of a doctor with experience in the use of cytotoxic agents. ADRIBLASTINA PFS is given by intravenous infusion. The doctor will determine the appropriate dose for each patient and the duration of treatment. The dose will be determined based on the patient's condition, weight, and height. Based on the patient's weight and height, the doctor will calculate the body surface area, which will be used to calculate the dose. The total dose of ADRIBLASTINA PFS administered during one cycle may vary depending on the indication and the treatment regimen used (e.g. the medicine may be given as monotherapy or in combination with other cytotoxic agents).
Overdose of ADRIBLASTINA PFS
Since the medicine will be administered under close medical supervision, overdose is unlikely. Overdose of ADRIBLASTINA PFS may lead to severe bone marrow suppression, gastrointestinal disorders, and heart problems (cardiotoxicity).
Missed dose of ADRIBLASTINA PFS
Since the medicine will be administered under close medical supervision, missed doses are unlikely. However, if a dose is missed, the patient should always inform their doctor or nurse.
Discontinuation of ADRIBLASTINA PFS
The decision to discontinue treatment is made by the doctor. Treatment should not be discontinued without consulting a doctor. If you have any further questions on the use of this medicine, ask your doctor, pharmacist, or nurse.
4. Possible side effects
Like all medicines, ADRIBLASTINA PFS can cause side effects, although not everybody gets them. The following side effects have been reported:
- Infection
- Leukopenia (low white blood cell count), neutropenia (low neutrophil count), anemia, thrombocytopenia (low platelet count)
- Decreased appetite
- Mucositis or stomatitis, diarrhea, vomiting, nausea
- Palmar-plantar erythrodysesthesia (hand-foot syndrome), alopecia
- Fever, weakness, chills
- Decreased ejection fraction, abnormal ECG, abnormal liver enzymes, weight gain
The following side effects have also been reported:
- Sepsis
- Conjunctivitis
- Heart failure, tachycardia
- Esophagitis, abdominal pain
- Urticaria, rash, hyperpigmentation, nail hyperpigmentation
- Injection site reaction
The following side effects have also been reported, but their frequency is unknown:
- Thrombosis
- Acute lymphocytic leukemia, acute myeloblastic leukemia
- Anaphylactic reaction
- Dehydration, hyperuricemia
- Keratitis, increased lacrimation
- Atrioventricular block, tachyarrhythmia, bundle branch block
- Shock, hemorrhage, thrombophlebitis, phlebitis, heat stroke
- Gastrointestinal bleeding, gastric ulcer, colitis, mucosal discoloration
- Photosensitivity, radiation recall reaction, pruritus, skin disorders
- Urine discoloration
- Amenorrhea, oligospermia, azoospermia
- Malaise
Reporting of side effects
If you experience any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly to the national reporting system via the contact details below. By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store ADRIBLASTINA PFS
Keep this medicine out of the sight and reach of children. Do not use this medicine after the expiry date which is stated on the label and carton after EXP. The expiry date refers to the last day of that month. Store in a refrigerator (2°C - 8°C). Protect from light. Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help protect the environment.
6. Contents of the pack and other information
What ADRIBLASTINA PFS contains
The active substance is doxorubicin hydrochloride (Doxorubicini hydrochloridum). 1 ml of solution contains 2 mg of doxorubicin hydrochloride. The other ingredients are sodium chloride (see section 2 "ADRIABLASTINA PFS contains sodium"), water for injections, hydrochloric acid for pH adjustment to 3.0.
What ADRIBLASTINA PFS looks like and contents of the pack
Clear, red solution. Packaging: 1 polypropylene vial of 5 ml, 25 ml or 100 ml, closed with a rubber stopper and aluminum cap and plastic flip-off cap, in a cardboard box. 1 glass vial of 5 ml, 25 ml or 100 ml, closed with a chlorobutyl rubber stopper and aluminum seal and non-transparent, colored, plastic flip-off cap. Each vial is packaged in a transparent, plastic protective cover, in a cardboard box.
Marketing Authorization Holder
Pfizer Europe MA EEIG, Boulevard de la Plaine 17, 1050 Bruxelles, Belgium
Importer
Pfizer Service Company BV, Hoge Wei 10, 1930 Zaventem, Belgium
For further information about this medicine, please contact
Pfizer Polska Sp. z o.o., tel. 22 335 61 00
Date of last revision of the leaflet
Detailed and up-to-date information on this product can be obtained by scanning the QR code on the outer packaging using a mobile device. The same information is also available at the URL: https://www.pfizer.pl/ulotka-adriblastinapfs and on the website of the Office for Registration of Medicinal Products, Medical Devices and Biocidal Products http://www.urpl.gov.pl .
Information intended for healthcare professionals only
Doxorubicin is administered by intravenous infusion. The doxorubicin solution is inactive when given orally and should not be administered intramuscularly or intraperitoneally. The total dose of doxorubicin per cycle may vary depending on the indication and the treatment regimen used (e.g. the medicine may be given as monotherapy or in combination with other cytotoxic agents). Doxorubicin should be administered by intravenous infusion in 0.9% sodium chloride solution or 5% glucose solution over a period of not less than 3 minutes and not more than 10 minutes to minimize the risk of thrombosis or extravasation. Rapid intravenous injections (bolus) are not recommended due to the risk of extravasation, which may occur even with proper placement of the intravenous line confirmed by aspiration of blood. Standard dose schedules: When doxorubicin is used as a single agent, the recommended initial dose is 60-90 mg/m² given as a single dose or divided over 3 consecutive days or on the 1st and 8th days of the treatment cycle. If toxic effects resolve, treatment cycles should be repeated every 3-4 weeks. It has also been shown that doxorubicin is effective when given at a dose of 10-20 mg/m² once a week. When doxorubicin is used in combination with other cytotoxic agents with similar toxicity, the recommended dose is 30-60 mg/m² per cycle. Adjuvant treatment of breast cancer: In a large randomized study conducted by the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-15, patients with early-stage breast cancer with axillary lymph node involvement received combination chemotherapy with doxorubicin 60 mg/m² and cyclophosphamide 600 mg/m², both given intravenously on day 1 of each 21-day treatment cycle. Four cycles were administered. Dose modifications: Hepatic impairment: The dose should be reduced in patients with the following bilirubin levels: - Bilirubin 1.2-3 mg/dl: 50% of the recommended initial dose - Bilirubin >3 mg/dl: 25% of the recommended initial dose Doxorubicin should not be administered to patients with severe liver impairment. Other special populations: Reduced initial doses or longer intervals between cycles may be considered in patients who have received prior systemic anticancer therapy or radiation therapy, children, elderly patients, obese patients, or patients with bone marrow infiltration. Doxorubicin should not be mixed with other medicines. Contact with alkaline solutions should be avoided, as this may cause hydrolysis of doxorubicin. Doxorubicin should not be mixed with heparin due to chemical incompatibility, which may lead to precipitation. Doxorubicin should not be mixed with fluorouracil (e.g. in the same intravenous infusion bag or through a Y-connector) due to reported incompatibility, which may lead to precipitation. If combination therapy with doxorubicin and fluorouracil is recommended, the intravenous line should be flushed between administrations of these medicines. Storage of the solution for injection in the refrigerator may cause the formation of a gel-like substance. The gel-like substance will return to a slightly viscous solution after 2 to 4 hours at room temperature (15°C - 25°C). Any unused medicine or waste material should be disposed of in accordance with local regulations. The following safety precautions should be observed for all anticancer agents:
- Personnel should be trained in the proper technique for preparing and administering the medicine.
- Pregnant women should not perform any tasks that involve the handling of the medicine.
- Workers who come into contact with doxorubicin should wear protective clothing: goggles, gowns, single-use gloves, and masks.
- Preparation of the infusion solution should be performed in a specially designated area (preferably in a laminar flow cabinet). The work surface should be protected with a single-use, absorbent paper with a plastic protective layer.
- All materials used for preparation, administration, and disposal of the medicine, including gloves, should be placed in special containers for high-risk waste and disposed of at very high temperatures.
- In case of accidental contamination with the medicine, objects should be washed with a sodium hypochlorite solution (1%) and then rinsed with plenty of water.
- All used sanitary materials should be disposed of in the same way.
- In case of accidental contact of the medicine with the skin, the skin should be thoroughly cleaned with plenty of water and soap or a sodium bicarbonate solution. The skin should not be scrubbed with a brush.
- In case of accidental contact of the medicine with the eyes, the eyes should be tilted and flushed with plenty of water for at least 15 minutes. Then, a sodium bicarbonate solution should be used. The patient should consult a doctor.
- After removing gloves, hands should always be washed.
- Country of registration
- Active substance
- Prescription requiredNo
- ImporterPfizer Service Company BV
- This information is for reference only and does not constitute medical advice. Always consult a licensed doctor before taking any medication. Oladoctor is not responsible for medical decisions based on this content.
- Alternatives to Adriblastina PfsDosage form: Concentrate, 2 mg/mlActive substance: doxorubicinManufacturer: Ebewe Pharma Ges.m.b.H Nfg. KG Fareva Unterach GmbHPrescription requiredDosage form: Concentrate, 2 mg/mlActive substance: doxorubicinPrescription not requiredDosage form: Solution, 2 mg/mlActive substance: epirubicinManufacturer: medac Gesellschaft fuer klinische Spezialpraeparate mbHPrescription required
Alternatives to Adriblastina Pfs in other countries
The best alternatives with the same active ingredient and therapeutic effect.
Alternative to Adriblastina Pfs in Spain
Alternative to Adriblastina Pfs in Ukraine
Online doctors for Adriblastina Pfs
Discuss dosage, side effects, interactions, contraindications, and prescription renewal for Adriblastina Pfs – subject to medical assessment and local rules.